Nowadays surgical trainees are faced with a more reduced surgical practice, due to legal limitations and work hourly constraints. Also, currently surgeons are expected to dominate more complex techniques such as laparoscopy. Simulation emerges as a complementary learning tool in laparoscopic surgery, by training in a safe, controlled, and standardised environment, without jeopardising patient's safety. Simulation's objective is that the skills acquired should be transferred to the operating room, allowing reduction of learning curves. The use of simulation has increased worldwide, becoming an important tool in different surgical residency programmes and laparoscopic training courses. For several countries, the approval of these training courses are a prerequisite for the acquisition of surgeon title certifications. This article reviews the most important aspects of simulation in laparoscopic surgery, including the most used simulators and training programmes, as well as the learning methodologies and the different key ways to assess learning in simulation.
Hoy en día los cirujanos en formación se ven enfrentados a un menor entrenamiento quirúrgico debido a limitaciones legales y restricciones horarias, sumadas a la exigencia actual de dominar técnicas más complejas como la laparoscopia. La simulación surge como una herramienta complementaria de aprendizaje en cirugía laparoscópica, mediante el entrenamiento en un ambiente seguro, controlado y estandarizado, sin comprometer la seguridad del paciente. El objetivo de la simulación es que las habilidades adquiridas sean transferidas al quirófano, permitiendo disminuir las curvas de aprendizaje. Programas de simulación se han incorporado progresivamente en todo el mundo en residencias quirúrgicas y cursos de entrenamiento en cirugía laparoscópica, exigiéndose como requisito en algunos países para certificar la especialidad. En este artículo se revisan los aspectos más importantes de la simulación en cirugía laparoscópica, incluyendo los tipos de simuladores y programas de entrenamiento conocidos, así como las metodologías de aprendizaje y escalas de evaluación utilizadas.
The aim of this review is to show the most important aspects of simulation in laparoscopic surgery and, particularly, its role in teaching this surgical technique.
BackgroundNowadays, the world is faced with a challenge in terms of surgical training. At present, surgical residency programmes worldwide have to deal with several problems which make the learning of surgical trainees more complicated. There have been constraints for residents on hours devoted to the operating room due to a reduction in working hours, the low incidence of certain diseases in some centres, and the quality and safety policies regarding patients’ medical care.1–4
Laparoscopic surgery is currently required among the basic skill set that a surgeon must have.5,6 However, the learning of this technique is limited due to is higher complexity compared to open surgery and the lower number of cases to which a surgeon is exposed during training, and they are forced to complete the learning curve during their specialty career. In addition to the foregoing, nowadays there are also an increasing number of available laparoscopic procedures and new technologies, which results in even practising surgeons having to look for new methods of continuous training and learning, without jeopardising patient safety.
The traditional surgical learning paradigm is based on the performance of procedures supervised by a more experienced tutor, under the adage of “first watch, then assist and then operate”. This training model, with all its virtues, has the inconvenience of being dependent on the tutor's technical level and the speed with which skills are transferred from the professor. Furthermore, early exposure of trainee surgeons to performing more complex procedures, considering their training technical level, may result in an unsatisfactory learning experience for the apprentice and his/her tutor, without mentioning the potential consequences for the patient and the related ethical aspects.7,8
Simulation, a Valuable Learning Tool in Laparoscopic SurgerySimulation emerges as a complementary tool to traditional training for the acquisition of surgical skills, allowing reduction of learning curves in a safe and controlled environment.1,2,8 The aviation industry has a long history of research in simulation and transfer of skills in a real scenario. It has shown that approximately 2h of a virtual simulation programme (derived from virtual reality, which provides the user with the feeling of actually being there) are equivalent to 1h of a real flight.9 This largely effective experience may be suggested for teaching surgery, especially for minimally invasive procedures.
Training simulations offer the opportunity to learn in a structured environment and in an effective way, without jeopardising patient safety. It provides all students with equal access to fictitious clinical scenarios that promote deliberate and repeated practise of the procedure,10 as well as a standardised and monitored assessment, with previously defined, clear objectives. Finally, simulation enables effective feedback by the educator.11
Simulation has been incorporated into several medical fields, including undergraduate teaching through simulated patients, fictitious clinical scenarios, and training in procedures such as venipuncture, cricothyroidotomies, and pleurostomies.12 In our field, a training programme has also been implemented to perform successful laparoscopic bowel anastomoses, which may be performed by residents and surgeons at any time during their training.13–15
This is how, in laparoscopic surgery, simulation has come to play a key role in surgical training, for both trainee residents and surgeons who want to receive training in minimally invasive new techniques before implementing them in patients, such as single-port laparoscopy, natural orifice transluminal endoscopic surgery (NOTES), or the incorporation of new laparoscopic technologies and instrument sets. Laparoscopic simulation may even be used for basic training during medical school. The long learning curve featured by this technique, together with the high risks and costs of learning complex techniques such as intracorporeal suture in patients, has led to the development of specialised simulation centres, enabling surgeons to learn in a safe and effective way.13,16 Surgical skill training prior to surgical procedures has shown a more effective learning in the operating room, allowing the apprentice to focus on the technical details of the procedure, without the need of learn all of them for the first time in a patient.17–20
As far as training simulation constraints are concerned, this type of programme requires specialised laboratories, with accredited tutors trained in this new learning methodology. This implies high implementation and maintenance costs, which are not affordable for all centres. Moreover, current simulators are not reliable enough, due to the scarce tactile feedback (tactile feeling which simulates contact with objects, also known as haptic force feedback) virtual simulators have and to the limitations of simulated procedures in bench models. Finally, in training simulations the student usually receives training in a certain task under “ideal” conditions and in a repeated way, all of which may generate false confidence in the surgeon upon entering the operating room, due to thinking that the procedure is easier than it really is.19,20 Based on the above, training simulations should be used as a complement to traditional training and never as an alternative excluding it.20
The following paragraphs focus on showing the most important aspects of simulation in laparoscopic surgery, including the different types of well-known simulators and simulation programmes, as well as different training methodologies.
SimulatorsThere are several simulation alternatives in laparoscopic surgery. For the purposes of this review, they will be divided into 2 categories: those using inanimate objects and those using live animals.
Inanimate Models- a)
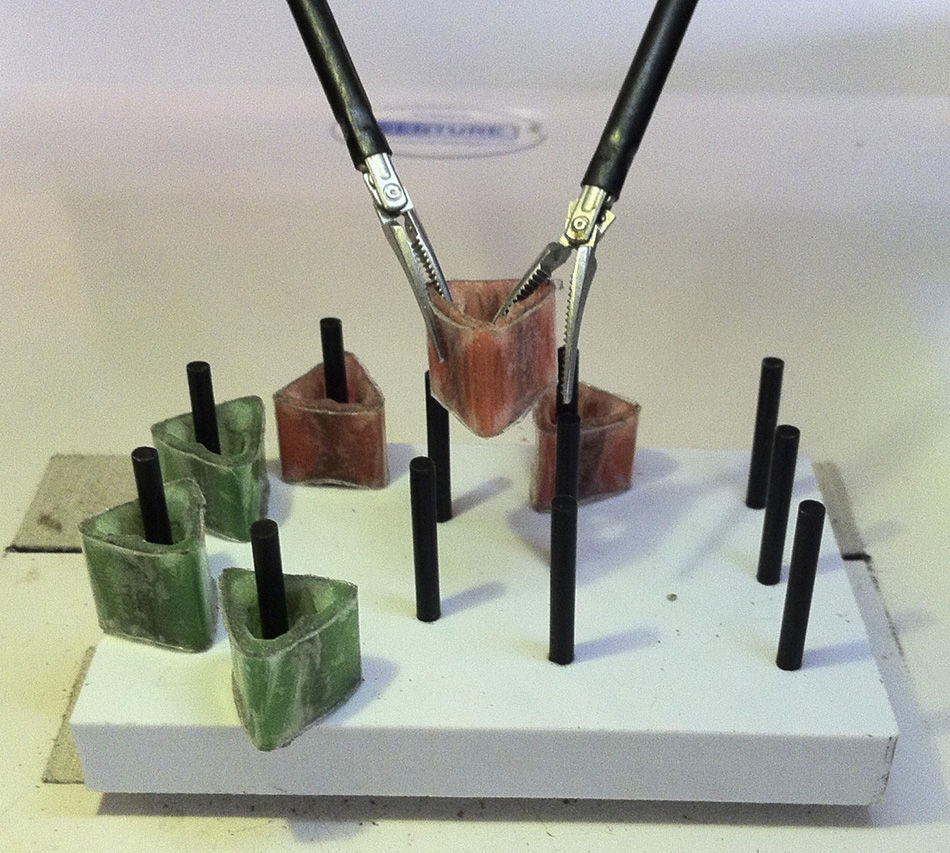
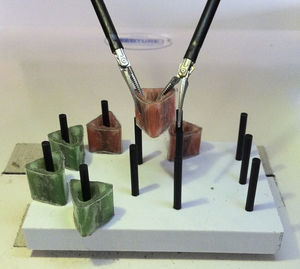
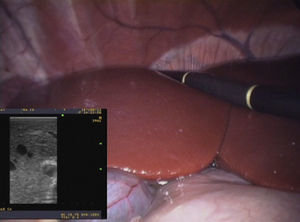
Endotrainers, pelvitrainers or bench models: These training models may be used for a wide variety of exercises, from the simplest ones, such as “taking and releasing objects”, to more complex procedures, such as several anastomoses. These models may be designed with inert objects (pieces of rubber or sponge, short ropes, etc.) or ex vivo tissues such as animal bowel or others. Among the advantages of these models one can mention their low cost, fast implementation, and the ability to effectively train on the most complex steps of a complete procedure, in a repeated way, in a short time (for example, a bowel anastomosis).13–15 Formal training programmes in basic laparoscopy, such as the Fundamentals of Laparoscopic Surgery (FLS) course (Fig. 1) and some training programmes in advanced laparoscopy have proved the transfer of acquired skills to the operating room.16,21
- b)
Cadaveric models: These may be of animal or human origin, depending on the procedure to be performed. They have an acceptable reliability and the advantage of enabling simulation of the complete surgery; however, their high cost and limited availability, as well as their differences with living tissue and ethical constraints in some countries, have limited their more widespread use.1
- c)
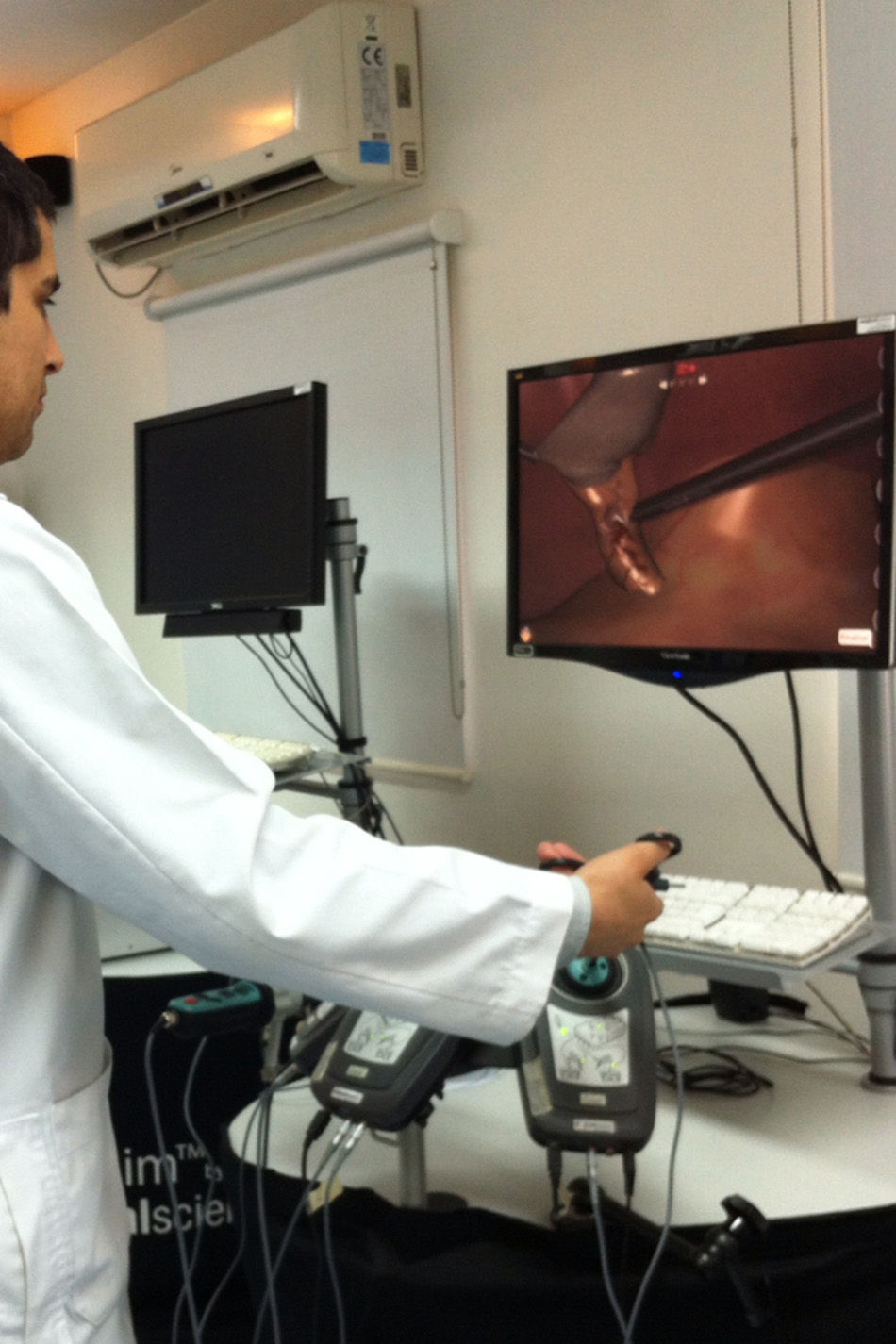
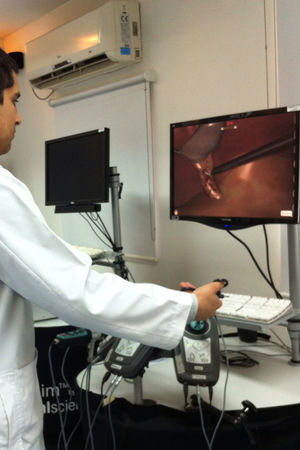
Virtual simulators (Fig. 2): These models enable the performance of complete procedures in one station, unlike “bench models” (where, for example, a cholecystectomy cannot be performed). In addition, they have immediate feedback as stages are achieved, which enables the correction of the most common mistakes during training. In the case of specific training programmes (such as surgery for the treatment of obesity), virtual simulation has allowed a reduction in training times and the need of a tutor being continuously present.22 Virtual reality studies have shown the transfer of most basic laparoscopic skills22 to the operating room, which is not the case of advanced laparoscopic surgery.
The main limitations of virtual simulators include their [high] costs and their still imperfect tactile feedback transfer for more complex procedures. However, it is still a controversial issue whether this haptic force feedback has an impact on the learning of the technique or not, as shown by some experiences and robotic surgery (robot-assisted surgery, controlled by the surgeon at a certain distance from the patient).23 One is likely to see significant advances in this field in the near future, with the development of high-fidelity technology as it has been in the case of simulation in neurosurgery and endovascular surgery.23
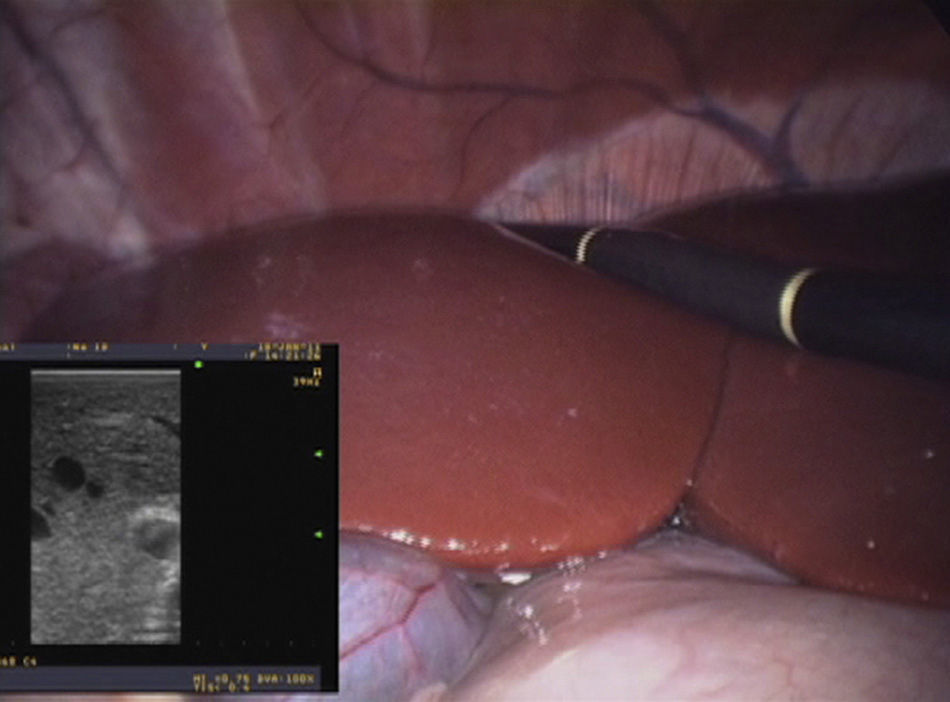
Living ModelsThese models use live animals, in general to emulate complete procedures that are difficult to reproduce in virtual simulators or bench models, such as a laparoscopic sleeve gastrectomy or a porcine intercavoaortic lymph node dissection. The advantages of these models include their high fidelity (unlike currently available virtual simulators) and the ability to emulate a complete procedure.
The main disadvantages include their high financial cost (each procedure requires general anaesthesia, surgical instrument sets, veterinary-trained personnel and operating rooms suitable for animal safety ethical requirements), which is why they are not usually affordable for most simulation laboratories (Fig. 3).
Learning and Training MethodologyThe implementation of a training simulation programme needs to include the critical aspects of a certain surgical procedure. It has to be determined whether it is necessary to provide training in the complete procedure or only for specific stages requiring higher technical skills, which depends on financial variables, the number of patients at the centre, the feasibility of simulating the procedure and the actual impact of the training model.
Kneebone19,20 states that surgical learning should be based on the 4 surgical competence pillars: theory, skill, experience, and decision-making. Other factors added are communication skills and teamwork, which characterise an integral surgeon.20 Technical skills have traditionally been the main focus of training simulation, but this aspect is only one of the surgical practice components. A training simulation that only includes technical skills will result in experienced non-expert24 surgeons, who have extensive expertise in common situations, but who are incapable of making good decisions20,24 in the face of unexpected changes in the environment, such as intraoperative complications. The foregoing is one of the differences with expert adaptable24 surgeons, who have more experience and who have received training in the rest of the surgical competence pillars as well. Surgical simulation has to tackle all these aspects to achieve complete and successful training, through versatile surgical scenarios, such as those available in virtual simulators and even with strategies such as using actors together with the simulation models, who while interacting with the apprentice reach a more reliable clinical scenario.25 This type of experience has been successfully used by other specialties, such as anaesthesia, through the implementation of crisis simulation scenarios in the operating room.26 This is how each and every training simulation programme should consider 3 key elements: the simulator, which has to be reliable and accessible; tutors accredited in learning and assessment methodologies, and students to be trained (medical students, surgical residents, or practising surgeons who wish to develop their knowledge).20
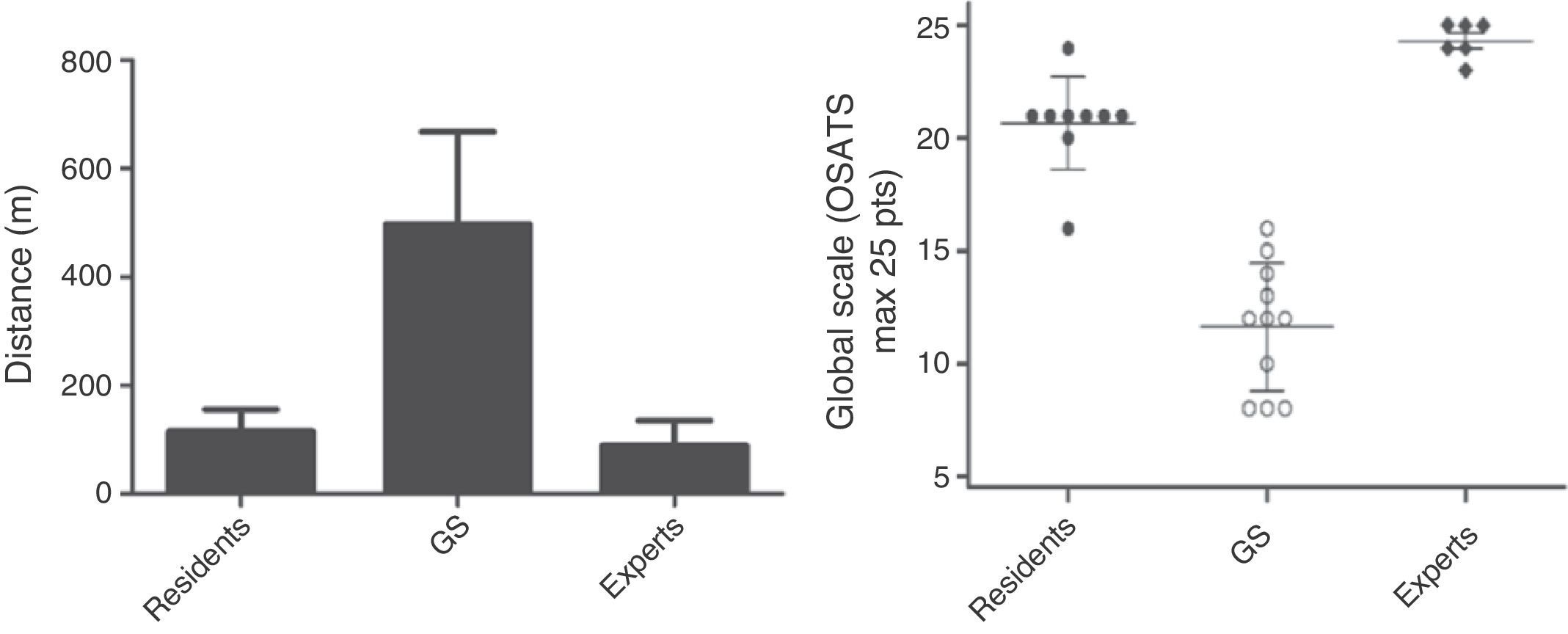
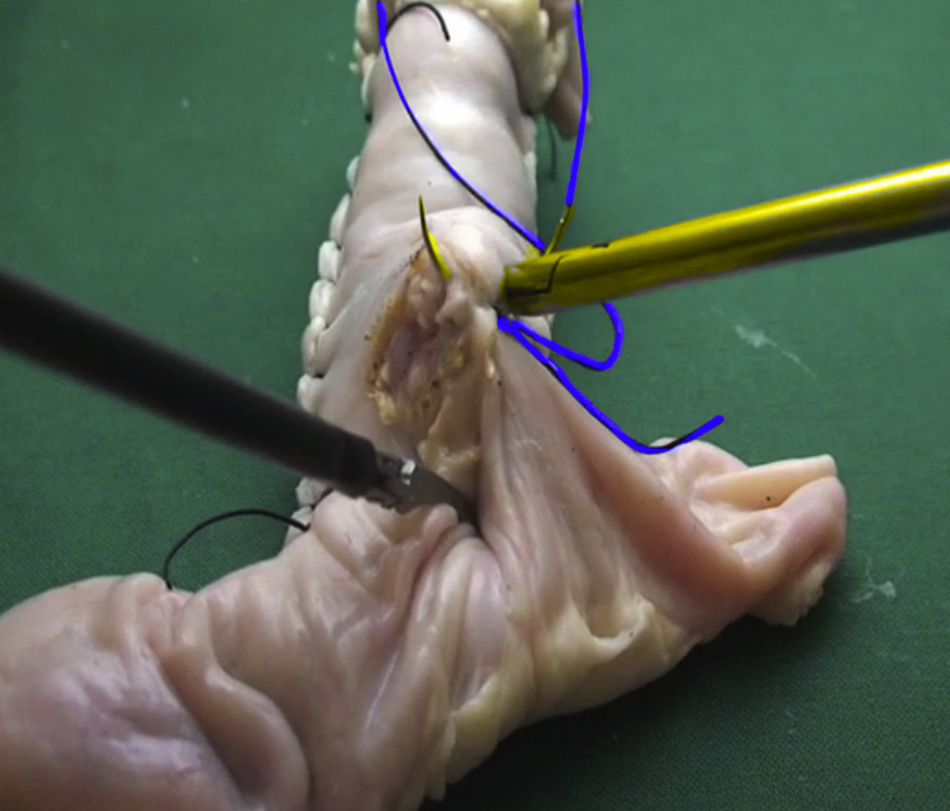
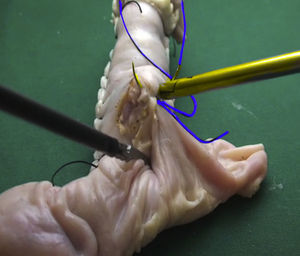
In our centre, a 16-session training model was developed for residents of surgical specialities, which required learning a laparoscopic bowel anastomosis. This inanimate bench model yielded significantly better results for trained students (general surgery first-year residents) compared to graduated surgeons from traditional programmes without simulation.13 Once training had finished, participants and the control group were assessed in a porcine living model performing a laparoscopic bowel anastomosis and they were compared with expert surgeons. Trained residents showed significantly better operative times and a better performance in technical skills compared to general surgeons without simulation programmes. Residents did not have any significant differences compared to experts13 (Fig. 4). Promising studies may yield the same results in an operating room in the near future.
Values obtained with Imperial College Surgical Assessment Device (ICSAD) expressed as total distance run in metres and Objective Structured Assessment of Technical Skills (OSATS) scale global scores obtained by general surgery first-year trained residents (residents), general surgeons without simulation programmes (GS), and expert surgeons (experts), while performing a bowel anastomosis in a living porcine model.
When designing and implementing a training programme, there are some key educational tools that should be considered:
- a)
Training by stages
This consists of the deconstruction of a procedure considering its basic components or stages; for example, if training is on a mechanical bowel anastomosis, one may divide the procedure into 4 stages: apposition suture, enterotomies, stapling, and anterior wall closure with continuous suture. The purpose is to make the student focus on each aspect of the procedure in a sequential way. Upon mastering a stage, new tasks will be added to the already consolidated knowledge, until eventually completing the required procedure.27–29
- b)
Theoretical sessions
Their application has been recommended in surgical simulation programmes with a view to optimising the training time,30,31 making the integration of simulation hours within a busy work schedule more feasible. Furthermore, it is the right instance for the introduction of new tasks or the explanation of the used assessment methods. Expository presentations, manuals, or instructional videos (Fig. 5) may be used, where the way how and the reason why a specific task should be performed are explained. Another modality includes video portfolios, which contain educational material and videos showing students and the mistakes they have committed and the corrections made by the instructors.
- c)
Feedback
This is one of the most important tools in medical education. The method of feedback will vary depending on the environment where it is given, for example, in surgery it is offered in the operating room under the tutoring model, while the apprentice performs the procedure. If the apprentice is not capable of completing the surgery in an adequate manner, the expert surgeon takes charge of it. One disadvantage is the variability of the information offered. In the case of simulation, the apprentice has to be previously interrogated and ideally assessed on the competences that are to be acquired, so as to subsequently start guided and standardised training. The main difference between the operating room and the simulation laboratory is that in the latter students are allowed to make mistakes. The expert tutor shall observe and correct the mistakes during the training session, enabling the student to resolve them in an accurate way. This method is called effective feedback29 and has been successfully used in laparoscopic training centres.28
The FLS course was presented in 2004 at the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) Conference, as a programme designed to teach the basic skills required in laparoscopic surgery. Since 2009, this programme has been considered a prerequisite for passing the Surgical Board [sic: Board of Surgery] examinations in the United States.21 The programme has a theoretical component and a practical component, which consists of standardised exercises in a bench model, such as moving objects from one position to another or intermittently pulling a rope with both hands. Hafford et al.32 proved that only 30% of active surgeons who had not received training in simulation were able to pass the FLS course, thus showing a clear deficiency in their laparoscopic technical skills compared to trained surgeons.
This programme has been validated for and proved its correlation with basic technical skills in the operating room, but not with advanced surgical procedures,21 which leads one to believe that although it is a good introductory course, there is a need to develop training programmes that provide the skills required to perform more complex procedures.
Advanced LaparoscopyWith the increasing popularity of laparoscopic surgery and the appearance of training programmes such as the FLS course, Laparoscopy 101,21 the use of virtual simulation, etc., surgeons have been looking for ways to continue their training beyond basic procedures. For example, in gastrointestinal surgery, the skill required to perform a laparoscopic gastric bypass is much higher than for a cholecystectomy, requiring advanced knowledge in intracorporeal suture and the use of mechanical suture devices. Suture and bowel anastomosis13–15 training models have been included in advanced training programme curricula, as well as new models of more complex procedures, which are still being developed (gastrojejunal anastomosis and biliodigestive anastomosis) (Fig. 5).
AssessmentHaving an objective assessment tool that marks the performance and advances made by students enables the improvement of the learning experience and programme failures. Variables such as operative time, procedure completion, and distance run by the surgeon's hands while operating are quite objective and generally have little variability among assessors. However, these variables represent only a first step in the assessment of a student's performance and do not imply a detailed description of the quality with which the exercise is being performed.
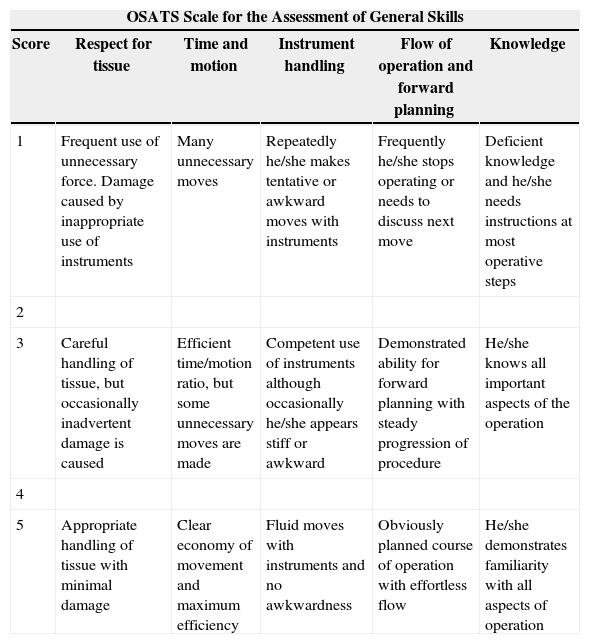
Due to this, practical skill assessment scales have been developed, such as Direct Observation of Procedural Skills (DOPS)33 and Objective Structured Assessment of Technical Skills (OSATS)15,34 scales, which are considered essential for the assessment of manual dexterity. The OSATS marking scheme is an example of a Likert-type scale, which comprises both general and specific aspects of students’ performance during a certain procedure, thus enabling the assessment of the surgical technique.3Table 1 shows an example of an OSATS scale for assessing general skills.
Modified Version of Objective Structured Assessment of Technical Skills (OSATS) Scale for the Assessment of General Skills.
| OSATS Scale for the Assessment of General Skills | |||||
|---|---|---|---|---|---|
| Score | Respect for tissue | Time and motion | Instrument handling | Flow of operation and forward planning | Knowledge |
| 1 | Frequent use of unnecessary force. Damage caused by inappropriate use of instruments | Many unnecessary moves | Repeatedly he/she makes tentative or awkward moves with instruments | Frequently he/she stops operating or needs to discuss next move | Deficient knowledge and he/she needs instructions at most operative steps |
| 2 | |||||
| 3 | Careful handling of tissue, but occasionally inadvertent damage is caused | Efficient time/motion ratio, but some unnecessary moves are made | Competent use of instruments although occasionally he/she appears stiff or awkward | Demonstrated ability for forward planning with steady progression of procedure | He/she knows all important aspects of the operation |
| 4 | |||||
| 5 | Appropriate handling of tissue with minimal damage | Clear economy of movement and maximum efficiency | Fluid moves with instruments and no awkwardness | Obviously planned course of operation with effortless flow | He/she demonstrates familiarity with all aspects of operation |
Measurement of the student's multiple technical attributes provides a better idea of his/her surgical dexterity and at which stage of the learning process he/she is in. Moreover, it enables us to establish cut-off points and thus decide if the student has the required skill level to pass a training course.35 Measurement of the achievement of learning curves is also useful to establish the effectiveness of a training programme, thus enabling tutors to identify the factors that favour or hinder the learning process.
Transfer of SkillsThe main purpose of any simulation programme is to transfer the acquired skills to a real scenario. Kirkpatrick36 defined 4 levels required to evaluate the effectiveness of a training programme (reaction, learning, transfer, and organisational value), establishing that at level 3 the important thing is to determine whether acquired skills and knowledge result in a better performance in real scenarios or not. In the case of surgical training, effectiveness may be defined as the degree to which simulation may prepare surgeons to perform surgical procedures in patients.36
Recent studies have shown that knowledge acquired by means of training simulation is transferred to the operating room,16,37–39 most of them in basic laparoscopic procedures and some approaching advanced laparoscopy. However, evidence supporting the effectiveness of simulation-based surgical training, compared to the traditional model, has been inconsistent. One of the main reasons for the wide variability of results is the absence of strict methodologies, aimed at obtaining reliability and validity of the assessment tools.4,29
Simulation Institutional ValueAccording to level 4 defined by Kirkpatrick, “organisational value”, an important aspect when evaluating the effectiveness of a training programme, consists of measuring its financial impact on the lowest levels of the organisation.36 In the case of simulation, it is necessary to establish the cost-effectiveness of a surgical simulation programme for the institution. It is known that both traditional training and simulation are costly for an institution4,40; however, the reduction of learning curves in a simulation laboratory could reduce operating room costs,4 especially by reducing the operative times, thus increasing the efficiency of the operating room. Having technically better surgeons who operate faster will result in lower costs for the institution, less surgical complications, a higher volume of patients for the organisation, etc. This has been proved in studies showing that simulation programmes are more profitable than exclusive conventional training, mainly in training programmes using bench models and virtual simulators with more than 10 residents.16 More studies are required in order to understand all the cost and safety implications for the patients of each institution, but everything seems to indicate that well-designed, validated, and properly implemented programmes may enhance the performance of a surgical training programme as a whole.
Conclusions and Future ProspectsSurgical education is experiencing a paradigm shift. Most residency programmes are concentrating their efforts on how to increase surgical practice within more restricted timetables, maintaining patient safety standards and incorporating minimally invasive surgery in traditional training programmes.
Simulation emerges as a promising solution to this difficult task, allowing reduction of learning curves in a safe and controlled environment, through the transfer of skills acquired in the training programmes to the operating room.
Surgical simulation scopes should not be limited to residency programmes; on the contrary, surgical simulation should be incorporated in medical undergraduate programmes in more basic procedures and by practising surgeons who aim for continuous training and learning.
Conflict of InterestThe authors declare that they do not have any conflicts of interest.
Please cite this article as: León Ferrufino F, Varas Cohen J, Buckel Schaffner E, Crovari Eulufi F, Pimentel Müller F, Martínez Castillo J, et al. Simulación en cirugía laparoscópica. Cir Esp. 2015;93:4–11.