Spontaneous splenic rupture (SSR) associated with the use of anticoagulants is uncommon.1 The term SSR is used for spleen ruptures with no history of trauma, regardless of histopathological findings.2
Statistically, 93% of these ruptures are associated with hematological diseases (pathological rupture), only 7% do not have an etiologic factor or histopathological changes (idiopathic rupture)3 and 9.1% of SSR may be associated with pharmaceutical drugs.1
We present a case of SSR in a patient with no hematological disease being treated with apixaban.
To assess its frequency, a bibliographic review was conducted in PubMed and updated on March 30, 2019, with no limits and using the following search strategy: (apixaban) AND ((spleen) OR (splenectomy) OR (hemoperitoneum) OR (spontaneous rupture)). Only 7 articles were found. All of them were analyzed, as were their references, and only 2 cases of SSR associated with apixaban were found.1,4
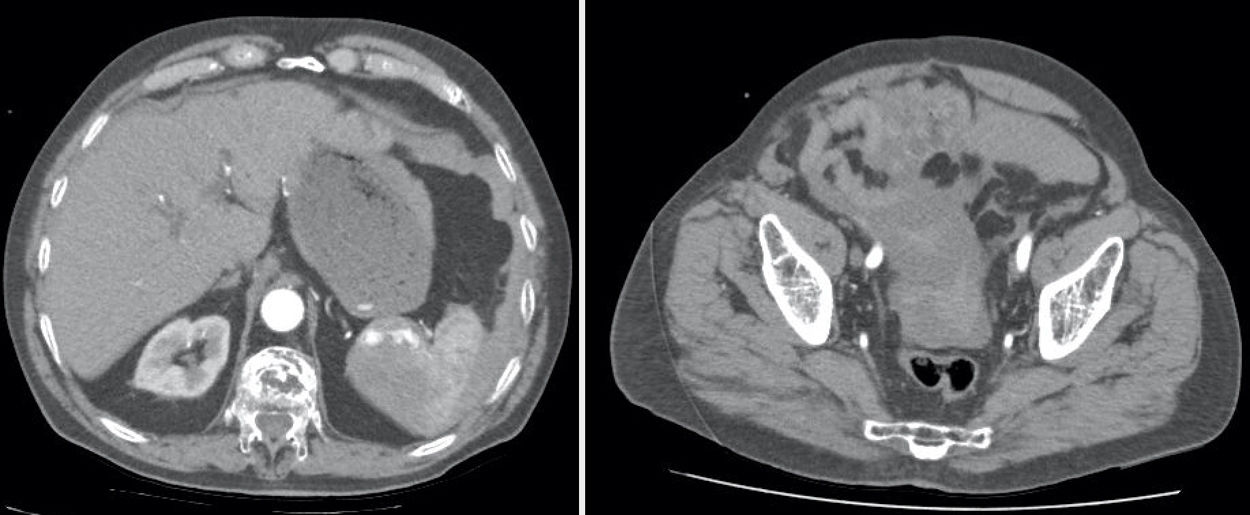
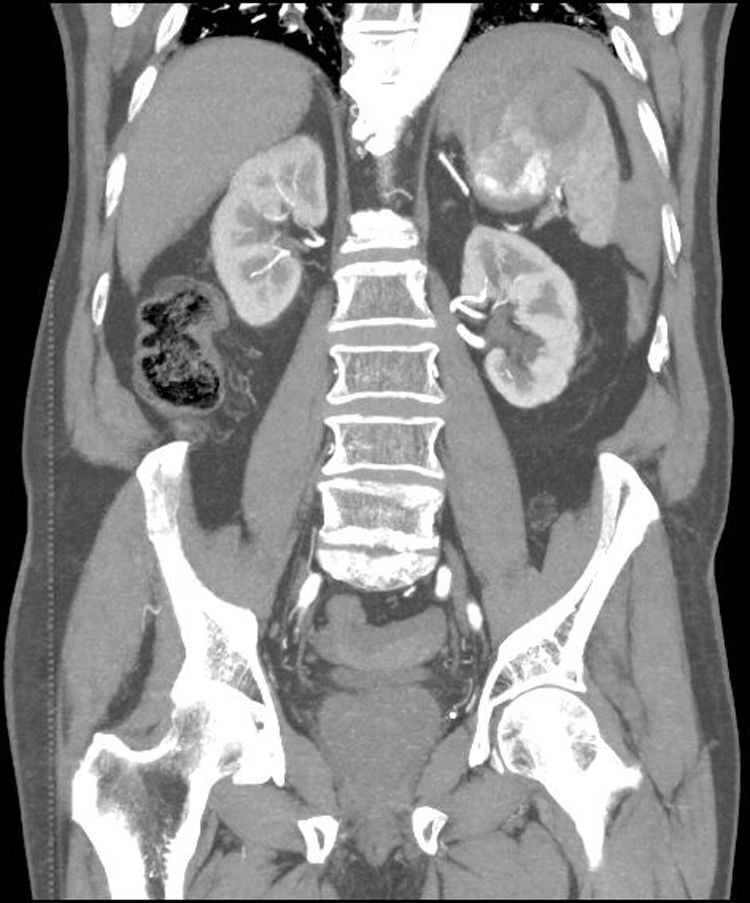
Our patient is an 88-year-old male with a history of atrial fibrillation treated with apixaban, heart failure and gastrectomy due to duodenal ulcer in treatment with omeprazole 20mg and furosemide 20mg. He came to the emergency department with diffuse intense abdominal pain that had suddenly appeared while sleeping. The last dose of apixaban had been taken 6h before. Blood pressure was 100/60mmHg, 62ppm, 98% SatO2 with weak peripheral pulses. Abdomen was globular, tympanic, distended, rigid and painful overall. Lab workup showed 14,000 leukocytes, 11.6 hemoglobin. CT angiography was performed with the suspicion of ruptured aortic aneurysm; splenic rupture was observed with active hilar bleeding and hemoperitoneum.
Urgent laparotomy revealed hemoperitoneum of approximately 1500cc and supramesocolic block due to adhesions. The spleen was accessed and splenectomy was performed; the abdominal cavity was washed, and a suction drain was placed in the surgical site.
In the intensive care unit, the patient received a transfusion of 2 units of packed red blood cells. He was transferred to the surgery floor on the 2nd postoperative day and discharged from the hospital on the 10th day. He was administered antibiotic prophylaxis with amoxicillin+clavulanic acid and presented no complications.
The histopathological study of the spleen detected a break in continuity of the splenic capsule, a focus of intraparenchymal hemorrhage, negative red Congo and thioflavin stains.
SSR is rare and is usually associated with an infectious, inflammatory, vascular, hematological or oncological condition or disease. A pathologically altered spleen (larger size, inflammation or structural change) presents greater fragility and can break spontaneously, without a trigger, or it can be triggered by a minor physical event.5
SSR during thrombolytic or anticoagulant treatment is even less frequent. It has been reported during treatment with tissue plasminogen activator, streptokinase, warfarin, Syntrom®, heparin,6 but only 2 cases have been reported in association with apixaban.1 In these cases, the pathophysiology is unknown. One theory proposes that a spleen with previous microtrauma may rupture when subjected to different hematological conditions, as seen in anticoagulant, thrombolytic or antifibrinolytic therapies.1
Apixaban is a direct and competitive factor Xa inhibitor indicated for the prevention of cerebrovascular accidents in patients with a history of non-valvular atrial fibrillation, for the prevention of thromboembolism in patients who have recently undergone knee or hip replacement surgery, and for the treatment of acute deep vein thrombosis and pulmonary embolism.1
The clinical presentation of SSR entails abdominal pain, hypotension and, in certain cases, hemorrhagic shock.1 Due to the common symptoms, it can be confused with a cardiac etiology or a suspected perforated peptic ulcer. Without a history of trauma that may indicate a possible splenic rupture, treatment is often delayed, particularly in patients with a history of cardiac or gastrointestinal problems.6
Similar to trauma injuries, treatment is determined by the hemodynamic stability and extension of the splenic injury, as described by the American Association for the Surgery of Trauma (AAST).7 CT scan is the most useful exploration in stable patients, as it shows the morphological signs of splenic rupture, severity of the injury and presence of associated lesions.
Urgent laparotomy should be performed in hemodynamically unstable patients with suspected active bleeding. In hemodynamically stable patients, conservative treatment should be considered with close monitoring and constant reassessment.1
Patients with SSR of malignant etiology should generally undergo immediate total splenectomy. Although under certain circumstances arterial embolization may be used as a temporary stabilizing measure,3 in our case we did not consider this option since it is not available to us (Fig. 1).
SSR associated with new anticoagulants like factor Xa inhibitors is very rare. The use of new oral anticoagulants is becoming more common and, therefore, it is important to consider this. A significant cause of mortality in these cases is the delay in diagnosis (Fig. 2).
Please cite this article as: López Marcano AJ, de la Plaza Llamas R, Latorre Fragua RA, Medina Velasco AA, Ramia Ángel JM. Ruptura esplénica espontánea asociada a apixaban. Cir Esp. 2020;98:164–165.