The use of robot-assisted minimally invasive surgery in ventral/incisional hernia repair has increased exponentially in recent years. This increase is probably related to the advantages of robotic surgery, among which are better visualization, the implementation of articulated instruments and better ergonomics for the surgeon. The TARUP (Robotic Transabdominal Retromuscular Umbilical Prosthetic Hernia Repair) technique combines the benefits of minimally invasive surgery, in terms of less wound-related morbidity, also allowing the placement of a mesh in a retromuscular position facilitated by the use of the robotic platform.
La reparación de la hernia ventral/incisional mediante cirugía mínimamente invasiva asistida por robot ha aumentado exponencialmente en los últimos años. Este aumento probablemente esté relacionado con las ventajas que aporta, destacando una mejor visualización, la implementación de instrumentos articulados y la mejor ergonomía para el cirujano. La técnica TARUP (Robotic Transabdominal Retromuscular Umbilical Prosthetic Hernia Repair) combina los beneficios de la cirugía mínimamente invasiva asistida por robot con una menor morbilidad relacionada con la herida y la colocación de una malla en posición retromuscular.
Most ventral incisional hernia (VIH) repairs are performed with open surgery, and the use of minimally invasive approaches is low.1,2 It is difficult to determine a specific cause for this poor implementation of minimally invasive surgery. Contributing factors may include: degree of technical difficulty, learning curve, lack of standardized training, or costs associated with different procedures.1 The advantages offered by robotic surgical platforms include better visualization and better movement capabilities, which allow the surgeon to complete technically difficult procedures. In addition, their use can contribute towards reducing the learning curve and the rate of postoperative complications, while also reducing the costs of the procedure in the long term.3
This article describes the TARUP (Robotic Transabdominal Retromuscular Umbilical Prosthetic Hernia Repair) technique published by Muysoms et al. in 2018.4 This procedure entails VIH repair assisted by the Da Vinci Xi robotic platform, which provides the benefits of this minimally invasive approach while also avoiding mesh placement in an intraperitoneal position.
Surgical techniqueThis technique is indicated in patients diagnosed with primary or incisional umbilical hernia and with a recommended mean size of 4 cm in transverse diameter.4
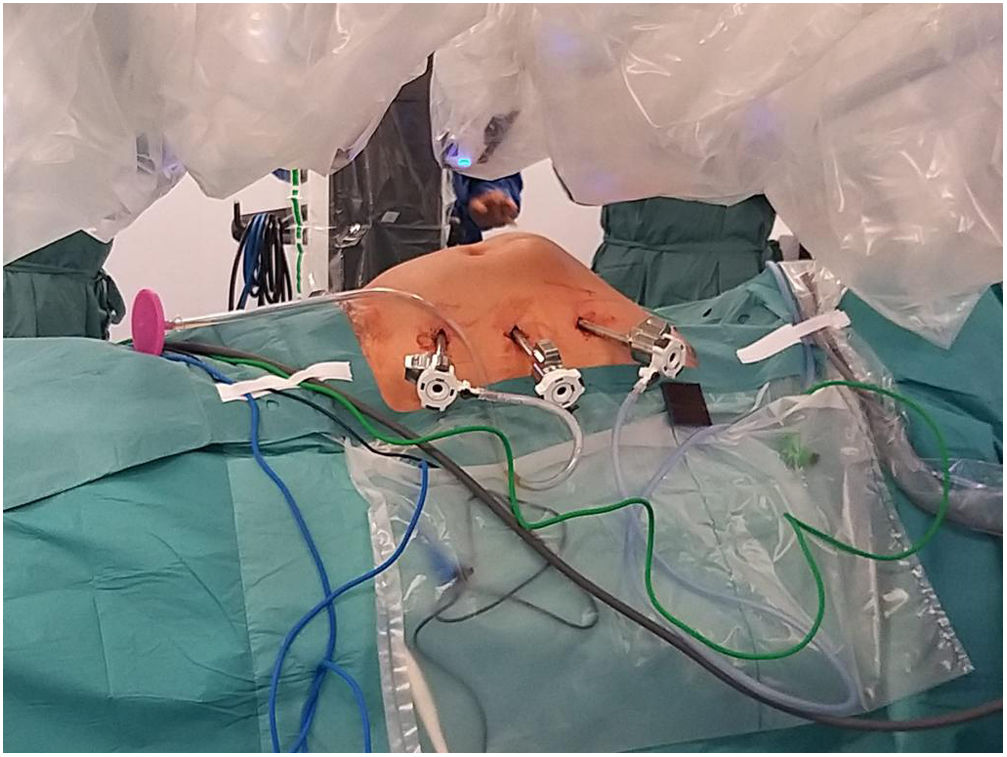
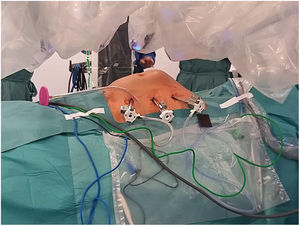
The patients were operated on using the Da Vinci Xi® system (Intuitive Surgical, Inc., Sunnyvale, CA, USA). Patients were placed in a supine position with both upper limbs close to the body; the robotic arm, or boom was located to the right of the patient, and the trocars were arranged on the left side. The nursing staff stood on the left side of the patient along with the assistant surgeon.
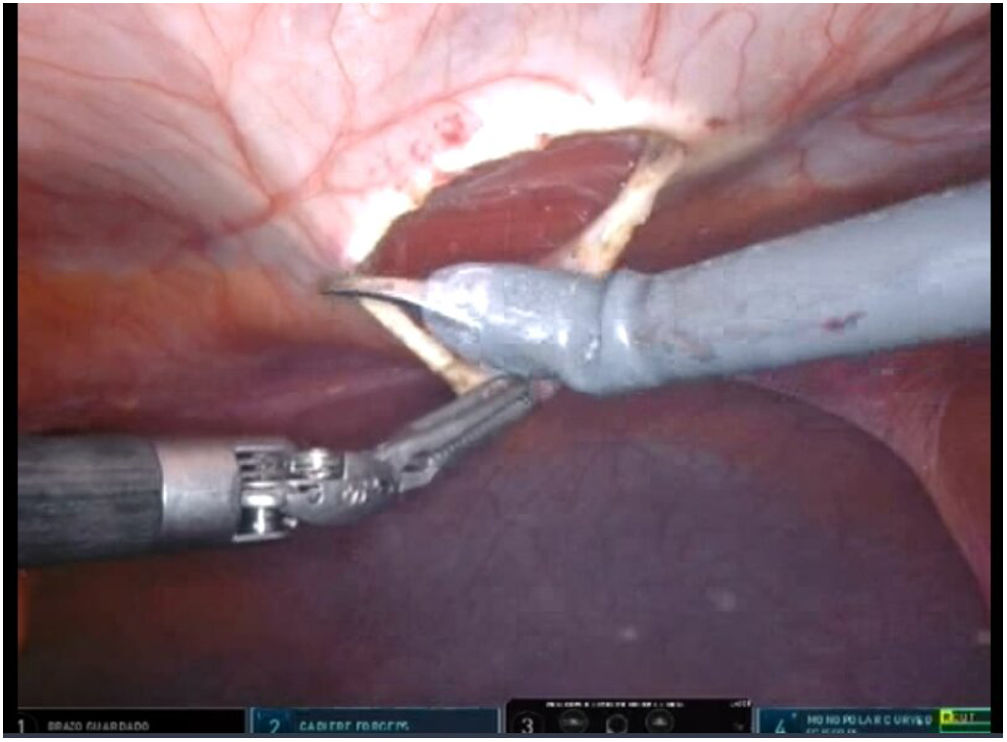
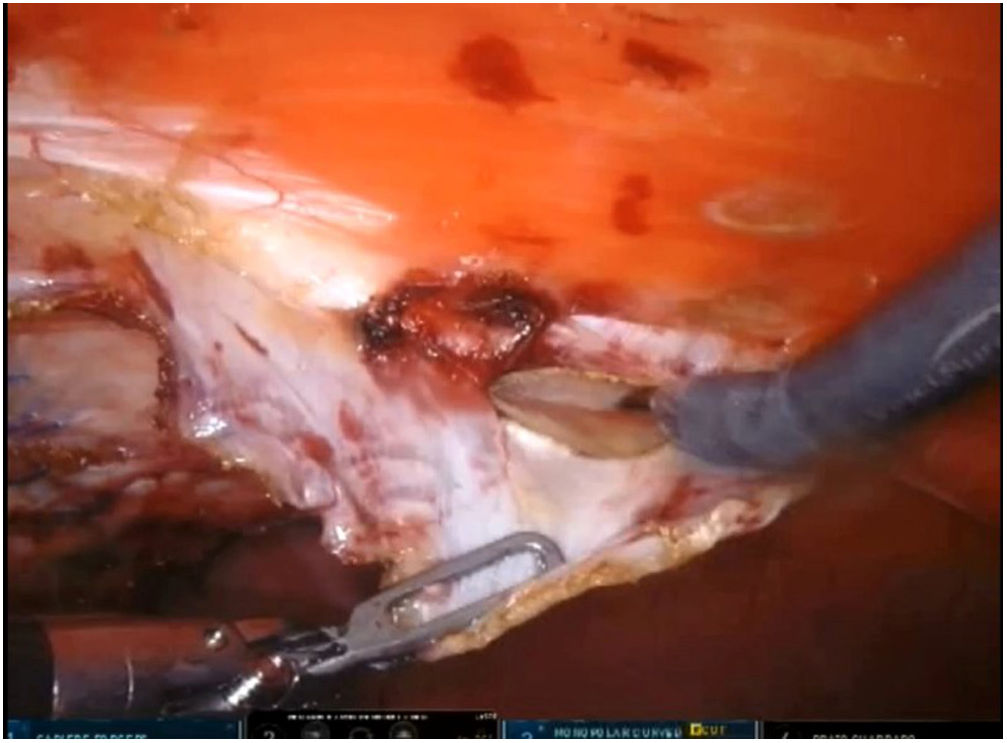
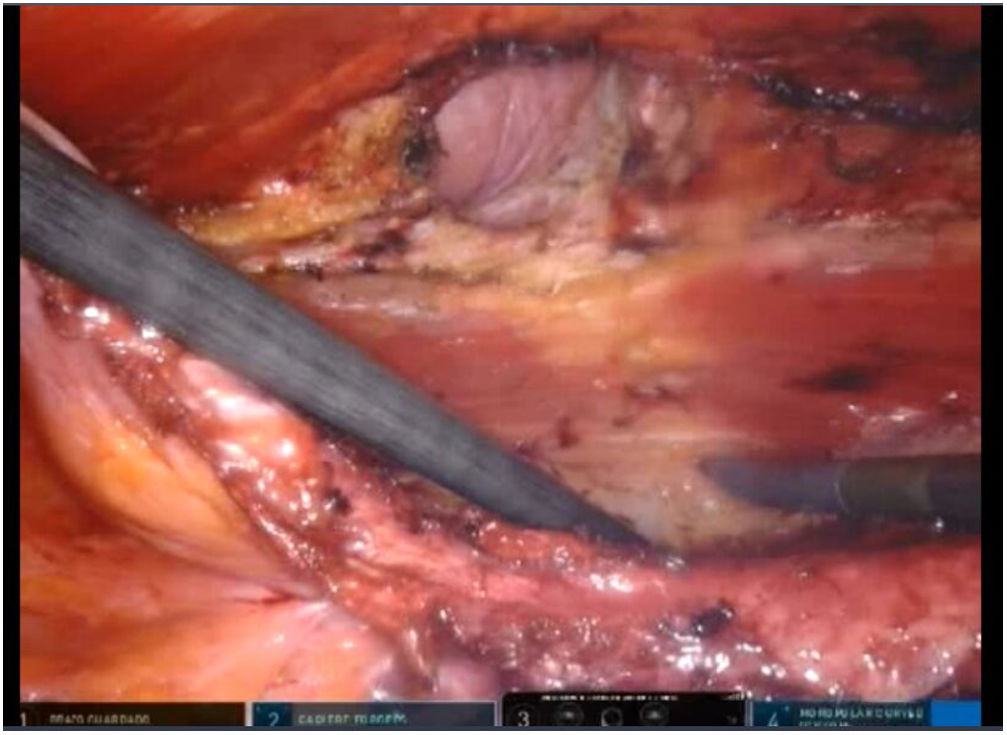
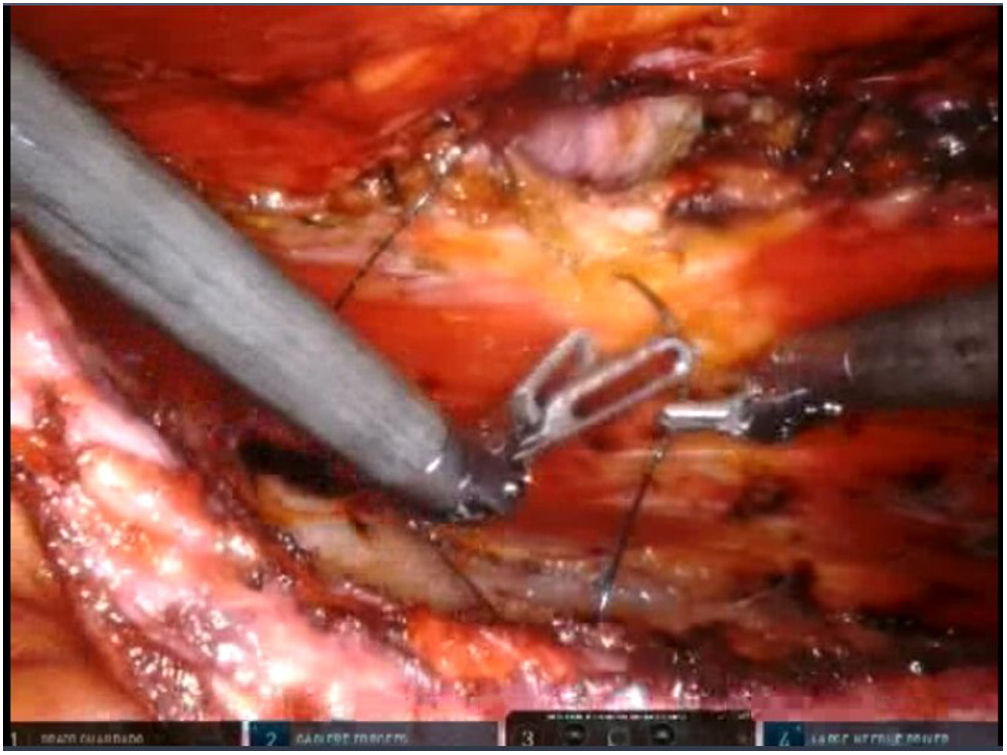
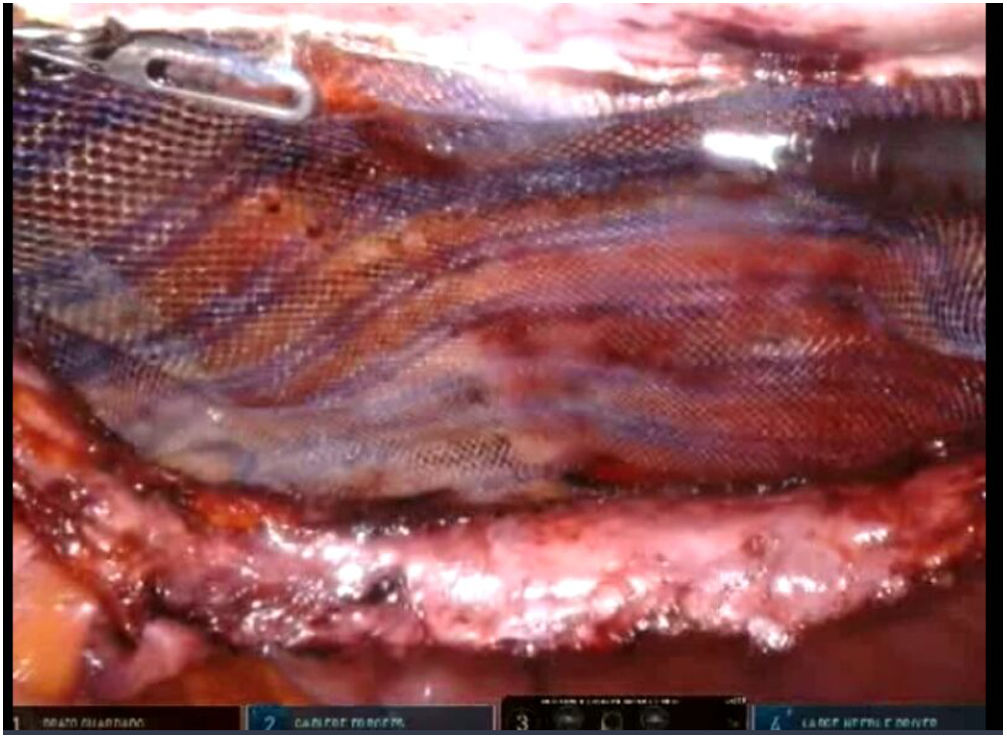
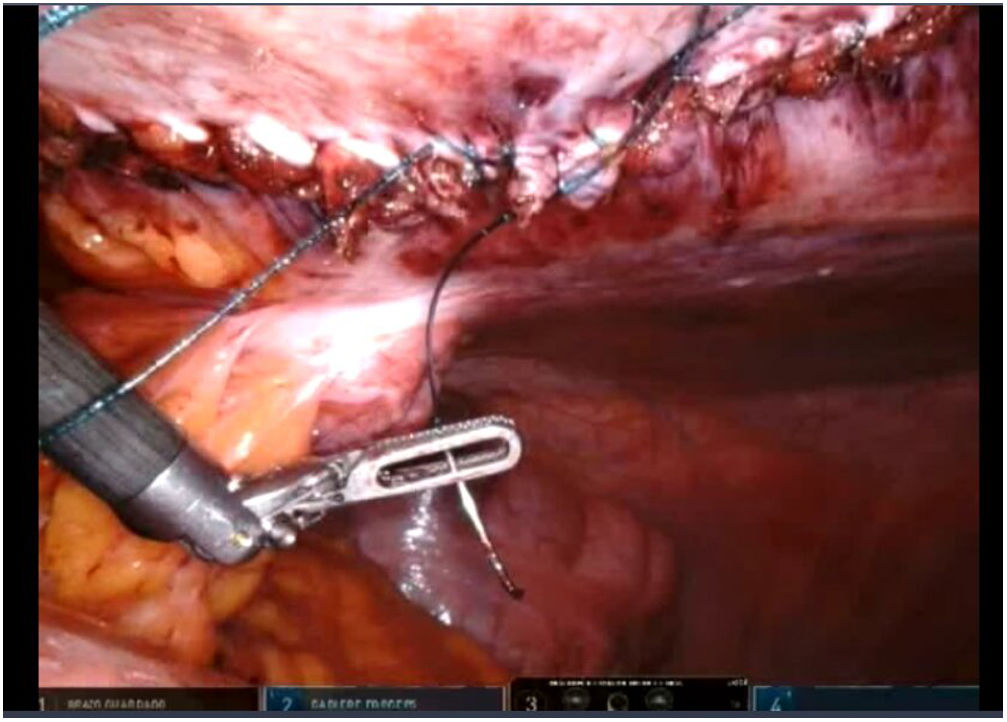
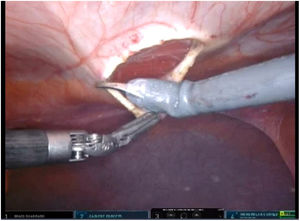
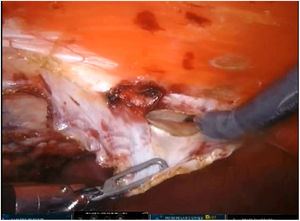
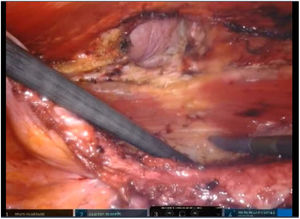
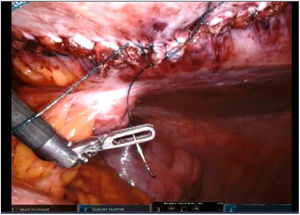
To create pneumoperitoneum, a Veress needle was used at Palmer’s point, reaching a maximum intra-abdominal pressure of 12 mmHg. The first 8 mm trocar was placed in the left subcostal region (2 cm from the costal margin) at the midclavicular line. Subsequently, the other two 8 mm trocars were placed under direct vision on the same vertical line (with approximately 8 cm between them) (Fig. 1). The robotic arms were attached to the trocars (docking). The 30-degree optical camera was located in the central trocar. The instrumentation used included of the ProGrasp™ forceps, scissors with monopolar power connection, and needle holders (all instruments from Intuitive Surgical Inc., Sunnyvale, CA, USA). An incision was made in the posterior lamina of the left rectus sheath to access the retromuscular space (about 5 cm from the midline). This incision was extended longitudinally, both cranially and caudally, using the direction of the rectus muscle fibers as a reference (Fig. 2). The retromuscular space dissection was advanced towards the midline until the junction of the anterior and posterior laminae of the left rectus sheath was identified. An incision was made about 0.5 cm below said junction, providing access to the space behind the linea alba (crossover). The dissection was extended, surrounding the hernia, whose content was reduced while attempting to preserve the peritoneum intact (Fig. 3). The posterior lamina of the contralateral rectus sheath was then incised to access the right retromuscular space, completing its dissection. This dissection of both retromuscular spaces had a radius of at least 6 cm around the hernia (Fig. 4). The hernia defect was closed using a continuous suture with barbed, slowly-absorbed material (V-Loc™ [2/0], Medtronic, Madrid, Spain) after lowering the pneumoperitoneum pressure to 8 mmHg (Fig. 5). Subsequently, the medium-weight, wide-pore polypropylene mesh was inserted with a size adjusted to the retromuscular space created. The mesh was affixed with 4 cardinal sutures of PDS 2/0 (Fig. 6). Finally, the posterior lamina of the left rectus sheath was closed using a continuous suture of slowly-absorbed, barbed material (V-Loc™ [3/0], Medtronic, Madrid, Spain) (Fig. 7). No surgical drains were placed.
From September 2018 to August 2020, 10 patients were treated with the TARUP technique (4 patients with primary umbilical hernia and 6 with incisional hernia). Mean age was 67.1 years (SD 9.9), and 4 of the patients were women. The mean BMI was 28.8 kg/m2. Regarding comorbidities, 2 patients had COPD and 6 diabetes mellitus.
The mean transverse diameter of the hernia defects was 3.4 cm (SD 1.48). Only one patient had a 2-day hospital stay, and the remainder were discharged the day after surgery. Five patients presented type 1 seroma, according to the Morales-Conde classification,5 and one patient presented omphalitis that was resolved with local treatment. Mean follow-up was 7.3 months (SD 4.6). One patient presented recurrence 7 months after the procedure, which was treated using an open approach.
DiscussionOpen-access sublay mesh repairs have been considered by many to be the gold standard treatment of VIH. This technique is associated with low rates of recurrence and surgical wound complications compared to other open techniques.6 In recent years, the use of laparoscopy in VIH repair has been performed mainly at the expense of the placement of an intraperitoneal mesh (eg, IPOM and IPOM plus). These techniques have been associated with a lower rate of surgical wound infection and similar recurrence rates when compared with open surgery.7 However, long-term disadvantages have been reported, such as the formation of adhesions, pseudo-recurrences (eg, bulging), seroma, and chronic pain secondary to intraperitoneal mesh fixation.8–11 In this context, in 2013 a laparoscopic technique for VIH repair was described using a lateral retromuscular approach with placement of a mesh in this position. This technique combined the benefits of laparoscopic surgery and avoided the placement of an intraperitoneal mesh. The authors of this technique conclude that it is safe and effective but technically very demanding12 since it requires dissection and sutures in the ‘roof’ of the abdominal cavity; it probably did not become popular for this reason. As mentioned above, this same technique was recently described under the name TARUP but using the Da Vinci Xi robotic platform4; this series included 41 patients, the vast majority of which were treated in a day surgery regimen, with good short-term results. The authors of this robotic series conclude that it is a reproducible, safe technique with a shorter operative time compared to the conventional laparoscopic approach.4 As far as we know, this study is the second series published in the literature.
Among the advantages of TARUP, we should highlight the fact that it avoids intraperitoneal mesh placement, potentially reduces wound-related complications, and is associated with less postoperative pain. In addition, the robotic approach allows for greater precision in suturing and comfort compared to conventional laparoscopy, with improved ergonomics for the surgeon. It is likely that, in coming years, with a greater availability of robotic platforms and more surgeons trained and experienced in their use, more VIH repairs will be performed using a minimally invasive robot-assisted approach. Furthermore, the TARUP technique appears to be reproducible and safe, with promising results that can make it attractive to start the learning curve in robotic surgery of the abdominal wall.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Rodrigues V, López-Cano M. Técnica TARUP. Ventajas de la cirugía mínimamente invasiva de la pared abdominal asistida por robot. Cir Esp. 2021;99:302–305.