Several changes introduced in the management of trauma during the last two decades have considerably decreased the practical exposure to bleeding trauma patients by residents and young surgeons. Hemorrhage still represents the second cause of death from trauma worldwide, and the surgical maneuvers required for its control must be learned and practised in specific courses. These courses address the “second hour” of trauma, beyond ATLS©, and also emphasize the decision-making process, communication among team members, and discussion of clinical scenarios. The significant progress made in simulation technologies and virtual reality systems have yet to replace living tissue models to train surgeons in the rapid control of active bleeding, although that replacement is probably not far away.
Diversos cambios introducidos en la atención al paciente traumatizado en las dos últimas décadas han hecho disminuir considerablemente la exposición práctica al manejo de las lesiones viscerales y hemorrágicas por parte de los MIR y cirujanos jóvenes. Esta hemorragia sigue siendo la segunda causa de muerte por trauma a nivel mundial, y determinadas maniobras quirúrgicas necesarias para su control adquieren a menudo una importancia crítica, debiendo ser aprendidas y ensayadas en cursos específicos. Son cursos dirigidos a la «segunda hora», más allá del ATLS©, y enfatizan también el proceso de toma de decisiones, discusión de casos clínicos y comunicación entre los miembros del equipo multidisciplinar. Los avances significativos experimentados en las tecnologías de simulación y los sistemas de realidad virtual no han logrado aún reemplazar a los modelos tisulares vivos para entrenar al cirujano en el control del sangrado activo de una manera rápida, aunque sin duda lo harán en un futuro no lejano.
Trauma injuries are an enormous public health problem worldwide, resulting in more than 5 million deaths per year and many more millions of disabled persons. According to recent data, trauma injuries caused by traffic collisions cause 1.25 million deaths per year and are the main cause of death in the 15- to 29-year-old age group. In addition, approximately 1.5 million people die as a result of interpersonal violence, and the remainder as a result of falls, war and other causes.1 The epidemiology of trauma varies greatly from one part of the world to another. While it is true that penetrating trauma is still frequent in many countries and traffic crashes are increasing in others, in many other countries this frequency is decreasing, thereby limiting clinical and teaching experience in the management of these patients.
The Need for Training Courses in the Management of Visceral TraumaChanges have been made in trauma care in the last 2–3 decades that have led to considerable improvement in the survival prognosis of severe trauma patients. The most important modifications have been in the conservative management of solid organ injuries, selective surgical management of penetrating trauma, and the importance and growing role of interventional radiology procedures. These changes have considerably reduced the continued exposure of the so-called “trauma surgeons” (mainly in the US) to these patients and have contributed greatly to the “reconversion” of these trauma surgeons into emergency or “acute care surgeons”, with a scope of action that is no longer limited to trauma injuries. These advances, together with the better prevention of trauma in developed countries, excessive atomization or dispersion of patients in too many hospitals in many regions and countries, and limitations to the working hours of surgeons-in-training imposed by the European Work Training Directives2 and the Accreditation Council for Graduate Medical Education,3,4 hinder continued contact with these patients. Exposure is considered essential to gain experience,5 and this experience is considered a key element for acquiring clinical and technical competence6,7; its limitation has led to a decline in surgeons’ confidence in the management of trauma injuries and increased morbidity and mortality.8
Two decades ago, some American trauma surgeons were already calling attention to the effect that the non-operative management of abdominal solid organ trauma would have on the surgical experience of surgeons during training.9 Together with many others, Lucas and Ledgerwood also warned about the training gap caused in future emergency surgeons by the decrease in the incidence and the number of therapeutic laparotomies due to trauma, providing as an example a study on hepatic trauma patients treated in the previous 5 decades. They concluded that surgery residents will need to supplement their clinical experience in hemostasis of solid organs with practices in appropriate animal models and cadaver dissections.10,11 With few exceptions, general and digestive system surgeons (GDSS) perform the surgical maneuvers for damage control in unstable patients with trauma-related bleeding in the trunk and, in spite of the aforementioned decrease in this type of patients in our setting, we must be well-versed in these life-saving maneuvers. Bleeding continues to be the second leading cause of death from trauma worldwide, second only to TBI, and is the direct cause of death in a significant percentage of patients who are alive upon arrival to the hospital. However, largely due to the surgical subspecialization seen in recent years, a majority of GDSS are not familiar with the control of bleeding in the thorax, liver or large vessels, even though serious injuries in these areas often lead to death. Therefore, specific training in the management of this type of injuries is necessary with practical courses to develop the required technical skills, emphasizing the management of cervicothoracic penetrating trauma and serious hepatic trauma, control maneuvers for abdominal vascular trauma, and management of pelvic fractures with hemodynamic instability. Among the most frequent errors reported in several studies is the inadequate evaluation of the abdomen and the delay in the decision for therapeutic intervention, both in laparotomy as well as emergency and resuscitative thoracotomy.12 However, not only has the delay in the diagnosis of fatal intra-abdominal hemorrhage been recognized as one of the main causes of avoidable mortality, but also the delay in the implementation of correct hemostasis procedures.13,14 The causes of these errors include insufficient experience and training in trauma of many of our surgeons, the organizational heterogeneity among hospitals for the care of these patients in our setting,15,16 and the occasional presence of very complex problems requiring treatment by trained teams and well-established protocols. This heterogeneity means that the components and leadership of trauma teams who receive these patients vary greatly according to the organization of each hospital, and there are even many hospitals where surgeons are not involved in the management process from the start.
Main Training Courses in the Management of Visceral TraumaAs of June 2016, 10 years had passed since the introduction of the “Definitive Surgery for Trauma Care” (DSTC) training course in our country, which is offered by the Trauma and Emergency Surgery Division of the AEC. The teaching experience of this course over the past 12 years has confirmed the interest of our young surgeons in being adequately trained in this field, from the perspectives of both the students and the instructors of the course. Likewise, we have been able to know and learn from the experience of instructors in other surgical specialties, such as thoracic and vascular surgery, and instructors from other countries with higher incidences of severe visceral trauma, mainly motivated by high rates of interpersonal violence and the availability of firearms in the general population. The DSTC© course came about as a response to a concern expressed by several internationally known trauma surgeons who, in the early 90s, recognized the need for a trauma course for the “second hour”, beyond the ATLS© course, and aimed at surgeons with no preferential dedication to these patients. The course has a practical focus, centered on the decision-making process, with extensive discussion about clinical cases, and a fundamental part aimed at practicing technical skills in simulation, using anesthetized live animals and/or cadavers. The course manual is updated periodically17 and used in several interactive informative talks, together with a DVD. The course was integrated into the International Association for Trauma and Surgical Intensive Care, which is a member of the International Society of Surgery-Societé Internationale de Chirurgie, based in Zurich.18 In the technical skills part, life-threatening scenarios are simulated in anesthetized animals, using hemorrhagic injuries that must be quickly and adequately controlled by the students, thereby generating high-stress situations where important mistakes must not be made.
The majority of specific training courses in surgery are more focused on technical aspects, such as sutures and instrument handling, than communication (with the anesthetist, discussion with the rest of the team about possible approaches, etc.) and team skills (help in handling instruments and assistance in surgery).19–22 This is understandable for simple training in skills like sutures, but not for complex surgical skills that involve team management. We know that many errors in the operating rooms are due to failures in these non-technical skills,22 and the DSTC© also deals with these non-technical aspects, although the limitations imposed by the time and structure of the course mean that they are not always properly developed. In an interesting recent analysis of the instructions and feedback provided by the DSTC© instructors in Nijmegen, Holland, it was observed that the instructions given to the students were much more frequent than the feedback provided subsequently by the instructors, which was also very non-specific, and that non-technical aspects of communication or teamwork were rarely emphasized.19 Reasons for this have been argued, such as the limited time, cognitive overload of the instructors when having to give instructions and immediate feedback while teaching the techniques, and the surgical level of occasional courses with advanced students. Breaks have been suggested as a strategy to increase this essential feedback during practice in the operating room. The philosophy of the DSTC© soon infiltrated the field of military surgery in the US, United Kingdom, Australia, France, Germany, Scandinavian countries, etc., and the Definitive Surgical Trauma Skills (DSTS©) became an essential course before military deployment to areas of conflict.5,23 Within the DSTC©, a military module was created as a requirement for the armed forces of the Australian Army.24 The German army has also implemented the so-called War Surgery Course since 1998; currently, it is a 5-day course of 20 theoretical modules, with 4 practical sessions in anesthetized live animals and the recent addition of a course involving exposure to vascular structures in cadavers.25 The French army has also developed its course based on these courses.26
In recent years an essential complement to the DSTC© has emerged, which directly involves the specialty of Anesthesia and Resuscitation, known as the Definitive Anesthesia Trauma Care (DATC©), which is taught together with the DSTC© in several countries of the European Union and also at two of the DSTC© offices in our country (Hospital Gregorio Marañón in Madrid, and Hospital Parc Taulí in Sabadell). As a result, anesthesiologists, as a fundamental component of the team that treats these patients, have become instructors for this course together with specialists in thoracic surgery and vascular surgery, specialties that have had several instructors since the course began to be taught in our country. In the Netherlands, the course is called DSATC©, and the experience has been very positive, helping to foster the spirit of teamwork that should always prevail in the care of these patients.27 The Advanced Trauma Operative Management (ATOM©) course was developed by the University of Connecticut in Hartford, and was adopted by the Surgical Skills Committee of the American College of Surgeons in 2001. It is a one-day course focused on the management of penetrating trauma, with a practical simulation component that is very similar to that of the DSTC©, with a student/instructor ratio of 1:1.28,29 The Trauma Exposure Course (TEC©) was designed at Parkland Memorial Hospital in Dallas, Texas, where the pilot course was taught in 2006.30 It was a course of about 8h using fresh, non-preserved corpses, focused on rapid exposure to vascular structures of vital importance in trauma to the neck, chest, abdomen and extremities. It was designed as a complementary course to ATOM©. This TEC© gave rise to the Advanced Surgical Skills for Exposure in Trauma (ASSET©) course developed by the American College of Surgeons – Surgical Skills Committee in 2010, after a first course developed in Bethesda, Maryland, in 2008, with objectives and structure that were very similar to TEC©. It is also a one-day course in unpreserved cadavers based on cases and scenarios and aimed at senior residents, trauma fellows and trained surgeons.8,31,32
Training With Cadavers or Live Anesthetized Animals?Historically, fresh, unpreserved cadavers have been used for the purpose of learning anatomy and surgical simulation. The use of cadavers provides knowledge of anatomical relationships to achieve vascular control, while the anesthetized live animal model allows training in the rapid control of hemorrhagic lesions to avoid death. The two models are complementary and should be seen as a symbiotic combination that maximizes the benefits of training.25 The use of biological experimental models with complete animals entails a series of ethical, moral and legal implications that must be considered and are often complex,33 and there is a growing awareness of the concern of animal rights activists. Animal simulation requires specialized facilities and personnel, especially if the use of large animals is intended. These facilities and procedures are subject to strict international regulations, and the animals are protected by the Animal Welfare Act of 1999, which states that animals have an intrinsic value, regardless of the value given by their habitual use by humans. The protocols followed for experimentation must be approved by an Ethics Committee and be in accordance with the Declaration of Helsinki on the International Standards of Good Clinical Practice. Therefore, the courses continue to evolve with the aim of replacing these living tissue models, although without sacrificing their educational value.34 In recent years there have been significant advances in simulation technologies and virtual reality systems, and in the near future animal simulations will probably be replaced by simulators with tissue properties similar to those of humans, where real instruments can be used.35
Furthermore, the restoration of adequate circulation in cadavers is another line of novel research to achieve this replacement. Arterial perfusion in cadavers for this purpose was already described in 2001 in an attempt to create a model for the evaluation of vascular devices and for simulation of vascular surgical procedures.36 The limitations of this initial model were that the venous system was not perfused and the perfusion fluid did not simulate blood. Later, a model was created fundamentally for trauma instruction, using cannulation of the large vessels and adaptation to an extracorporeal pump. The filling of the venous system was static through a femoral vein catheter, and authentic arteriovenous circulation was created by performing A–V shunts between the large vessels.37 Recently, the model has been perfected by means of pressurization techniques that have been shown to be very effective, and by adding a perfusion solution that closely resembles blood.38 It is important to incorporate these models after rigorous scientific studies and not as an emotional reaction to the pressures of antivivisectionist groups,25 although current living tissue models still cannot be replaced to train surgeons in rapid control of active bleeding.
Objective Evidence of the Benefit of Specific Training Courses in Visceral TraumaThe short-term improvement of certain surgical skills through practical general and visceral surgery courses, and the motivation that this generates, has been proven and is accepted. The vast majority of participants report a substantial improvement, both short- and long-term, in the degree of confidence for performing the techniques practiced.39 The actual duration of the beneficial impact of these acquired skills is important, and some studies find a longer duration when these skills are taught and practiced with a certain periodicity (weekly), rather than in a short intensive course with similar simulation training times.40 Due to the necessary and intensive practical teaching of these courses, the number of students is always small and this makes it difficult to conduct long-term studies (prospective and randomized) to validate their effectiveness. There are numerous studies about their design and structure, others where the participants evaluate them, and finally others where the student makes a subjective self-evaluation of the confidence acquired afterwards.25 The first 50 participants in the ATOM© course demonstrated substantial advances in knowledge and self-confidence in trauma management,28 and in a follow-up study of 104 participants 6 months later, the majority indicated that they were better able to identify and repair penetrating injuries.41 Unfortunately, it would be ideal to be able to objectively evaluate the clinical repercussions of the skills and knowledge obtained in these specific courses of visceral trauma management, but this is somewhat difficult to determine.42
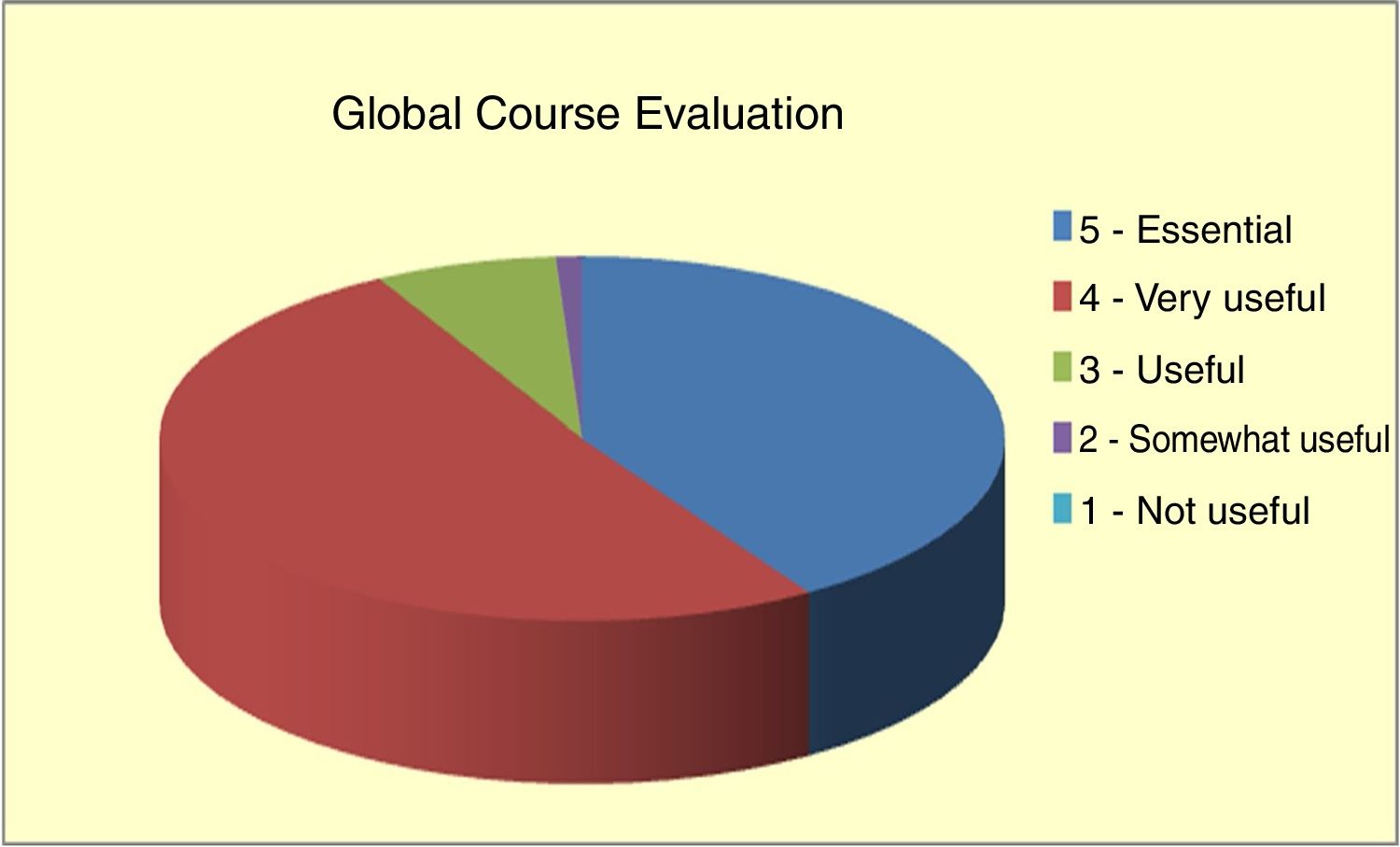
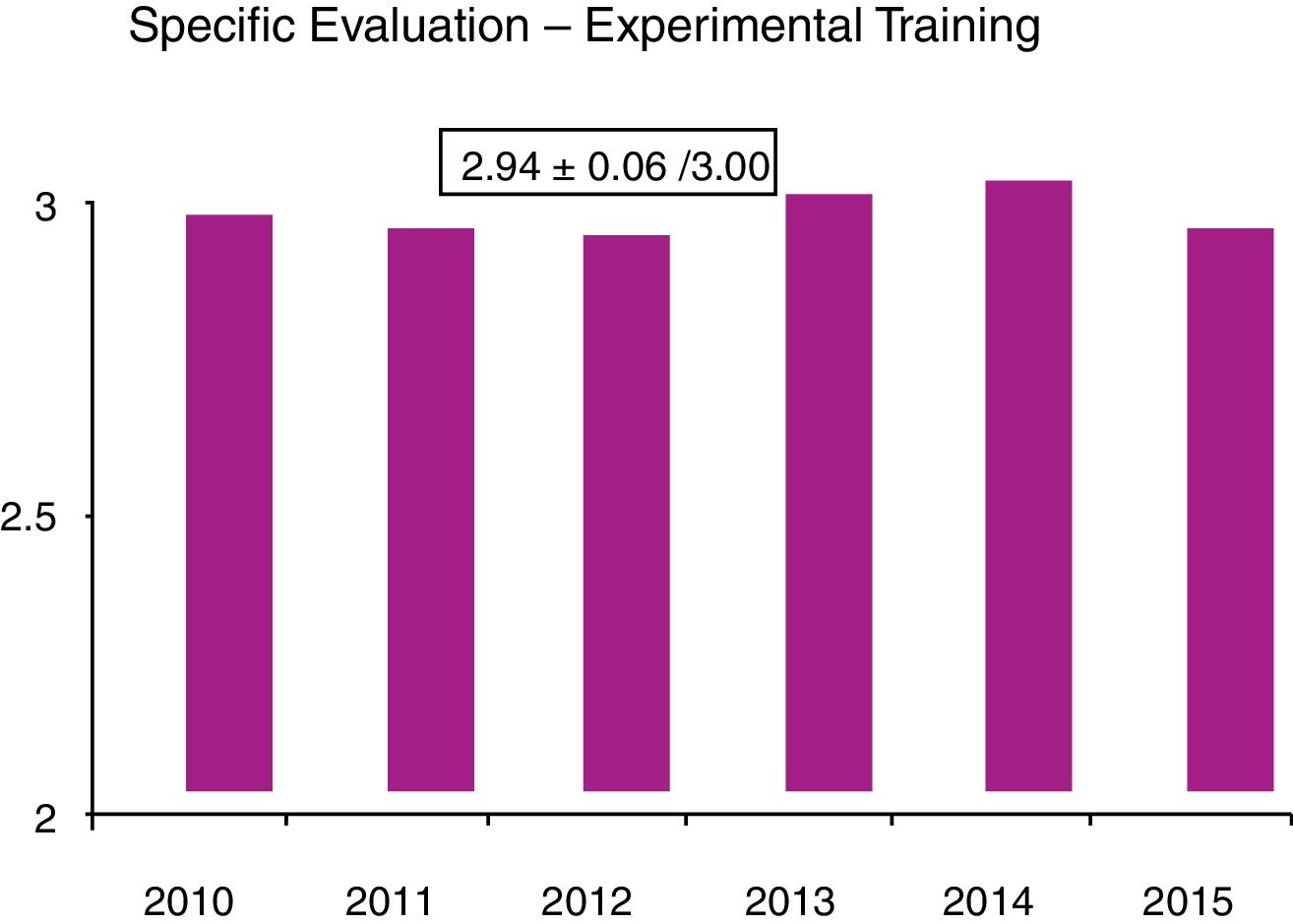
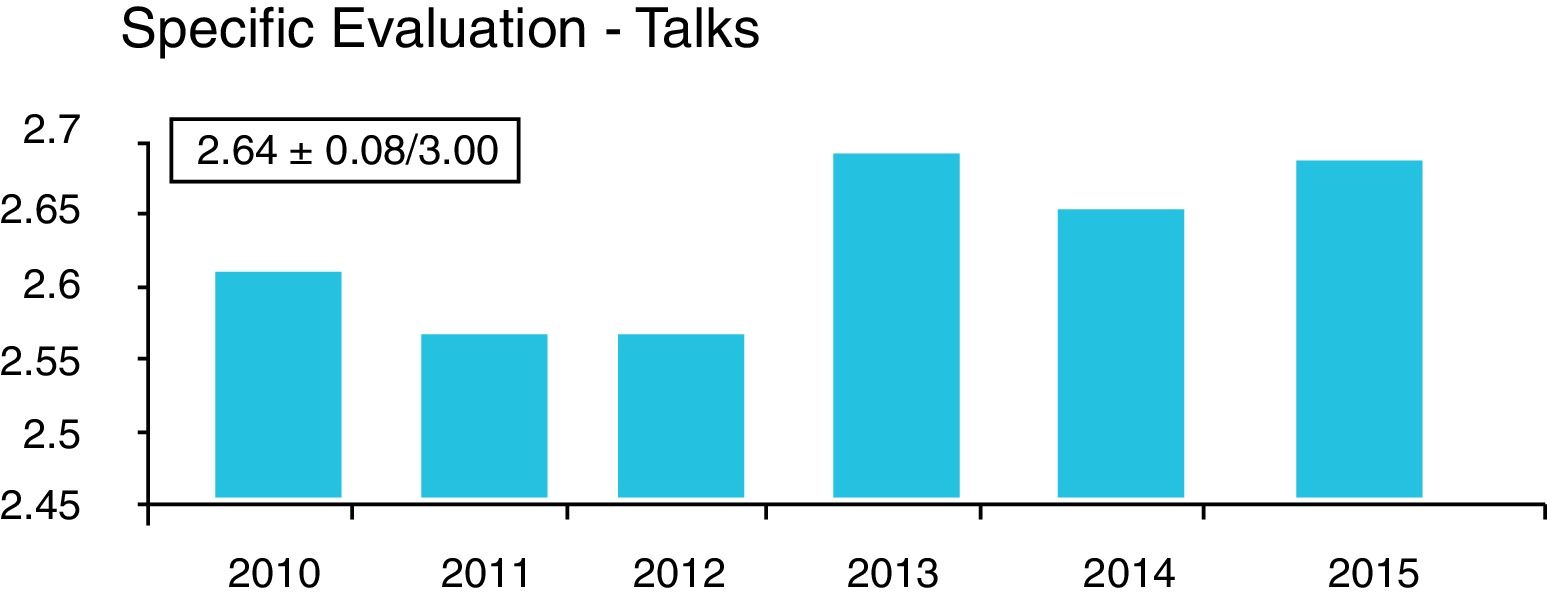
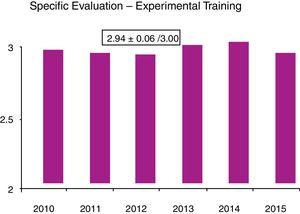
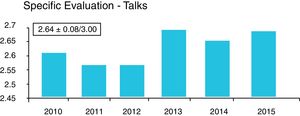
In the DSTC© course, the degree of acceptance by the student is quantified through the analysis of anonymous global and specific surveys that students complete at the end of the course. In our country, an analysis of these surveys in 2016, after 10 years of course implementation, yielded a very satisfactory global assessment (Fig. 1) and specific evaluation (Figs. 2 and 3). Especially relevant were training with animal models, the discussion of clinical cases, and the presence of experienced instructors from countries with a high prevalence of trauma. From July 2006 to April 2016, 43 courses were held with a total of 792 students and an instructor–student ratio of 1:3. In terms of age, 59% of students were in the 30–39 age group, 52% were attending physicians, and 29% 5th year MIR students. The overall assessment of the course was 4.3±6.2 of 5. Thus, the course was mostly completed by young staff and 5th year MIR residents, and the main negative factor was the cost. Currently, these training courses in visceral trauma are not part of the curriculum of our surgeons-in-training, who participate of their own volition and at a high personal expense, contrary to what happens with other GDSS courses, which are much more affordable. This may be one of the reasons for the current short waiting list for the courses, which is forcing the annual course offerings to be reduced. We believe that in the very near future we will have to reduce the number of hospitals that offer courses and limit them to those locations where they are jointly provided with the DATC© and/or where a minimum number of serious trauma patients are treated per year, which will undoubtedly improve the personal contribution of local instructors.
In conclusion, one of the pillars on which surgical teaching is based in general, and in the management of visceral trauma in particular, is the emphasis on the decision-making process and the teaching of technical, communication and teamwork skills. In visceral trauma, this teaching has an increasingly limited space in the daily clinical practice of our residents and young surgeons, and this means that the courses outlined in this paper should be an integral part of future curriculums. In our opinion, it would be desirable for all MIR residents in GDSS, Thoracic Surgery and Anesthesia-Resuscitation (and perhaps also the MIR residents of Vascular Surgery) to complete the DSTC©-DATC© courses during the last two years of their training period. Due to the high cost of the courses, financial support from the scientific societies would be necessary, given the growing difficulties for finding another type of financing for training.
Conflict of InterestsThe authors have no conflict of interests to declare.
We would like to thank the directors of the DSTC© course and the instructors, both national and international, who, with their experience and enthusiasm, contribute to its success.
Please cite this article as: Turégano Fuentes F, Pérez Díaz D. Docencia en el manejo del traumatismo visceral. Cir Esp. 2018;96:606–611.