Technology is one of the pillars of surgery in the 21st century and is a key factor in achieving better surgical results. The current surgical process involves not only surgical techniques, but also a very high degree of specialisation and the knowledge and use of techniques and devices from other fields. In Spain, there are no studies published at a national level in this regard.
From the Minimally Invasive Surgery and Technological Innovation section of the Spanish Association of Surgeons we have designed a study whose main objective is to evaluate the degree of technological implantation in the specialty of General Surgery in Spain, as well as to analyze the devices available in the different centres of the country. We propose to make a detailed description of the applications of these devices and techniques by areas of interest, pointing out the pathologies and procedures in which this technology is used.
La tecnología constituye uno de los pilares de la cirugía del siglo XXI y resulta un factor clave para la consecución de unos mejores resultados quirúrgicos. El proceso quirúrgico actual lleva implícito no sólo la técnica operatoria, sino un grado de especialización muy elevado y el conocimiento y empleo de técnicas y dispositivos propios de otros campos. En España no existen estudios publicados a nivel nacional a este respecto.
Desde la Sección de Cirugía Mínimamente Invasiva e Innovación Tecnológica (CMI-IT) de la Asociación Española de Cirujanos hemos diseñado un estudio cuyo objetivo principal es evaluar el grado de implantación tecnológica en la especialidad de Cirugía General en España, así como analizar los dispositivos disponibles en los diferentes centros del país. Nos planteamos realizar una descripción pormenorizada de las aplicaciones de dichos dispositivos y técnicas por áreas de interés, señalando las patologías y procedimientos en los que se utiliza dicha tecnología.
Technology and super-specialization are two pillars of 21st-century surgery because they are key factors for achieving better surgical results. Thus, today’s surgical processes entail not only the operative techniques used, but also a very high degree of specialization, as well as the knowledge and use of techniques and devices typical of other fields that had not been part of a surgeon’s activity until now. Digestive endoscopy, ultrasound or intraoperative choledochoscopy, new viewing devices, indocyanine green and robotic-assisted surgery systems are just some of these elements that have been shown to improve surgical results in our specialty1.
Despite having been controversial at times even within the surgical setting2, the application of technologies in surgical practice —some already established and others still emerging— has undoubtedly led to improvements in crucial aspects of the surgeon’s activity. Technology has made it possible to improve established techniques and develop new procedures, most of them in the field of minimally invasive surgery.
However, the current avalanche of technological innovations is being implemented unevenly among different surgical services. In some cases, this is happening even faster than the publication of robust scientific evidence defining its advantages over conventional surgery. This irregular usage also translates into an application of the technology that is asymmetrical and hinders the homogeneous evaluation of results, although this could be due more to economic criteria than to the disposition and training of surgeons for their assimilation and use3.
In Spain, we have little information on the actual application of these technologies, and no nation-wide studies have been published. The aim of the Minimally Invasive Surgery and Technological Innovation Division (Sección de Cirugía Mínimamente Invasiva e Innovación Tecnológica, or CMI-IT) of the Spanish Association of Surgeons (AEC) is to inform, train and disseminate knowledge and methods about different minimally invasive approaches in surgery as well as new developments and innovations as they appear. However, in order to do so, it is necessary to know about the state of implementation of the technology in the general surgery services of our country.
The main objective of this study is to evaluate the degree of implementation of new technologies in the specialty of general and digestive surgery in Spain, as well as to analyze the applications of these devices and techniques by areas of interest, indicating the pathologies and procedures in which the technology is used.
MethodsStudy designA descriptive study was designed with a closed survey, which was sent via email to the heads of the General and Digestive System Surgery Services throughout Spain who were members of the AEC during the months of April to December, 2019.
To prepare the survey, a form was created at https://docs.google.com/forms/u/0/
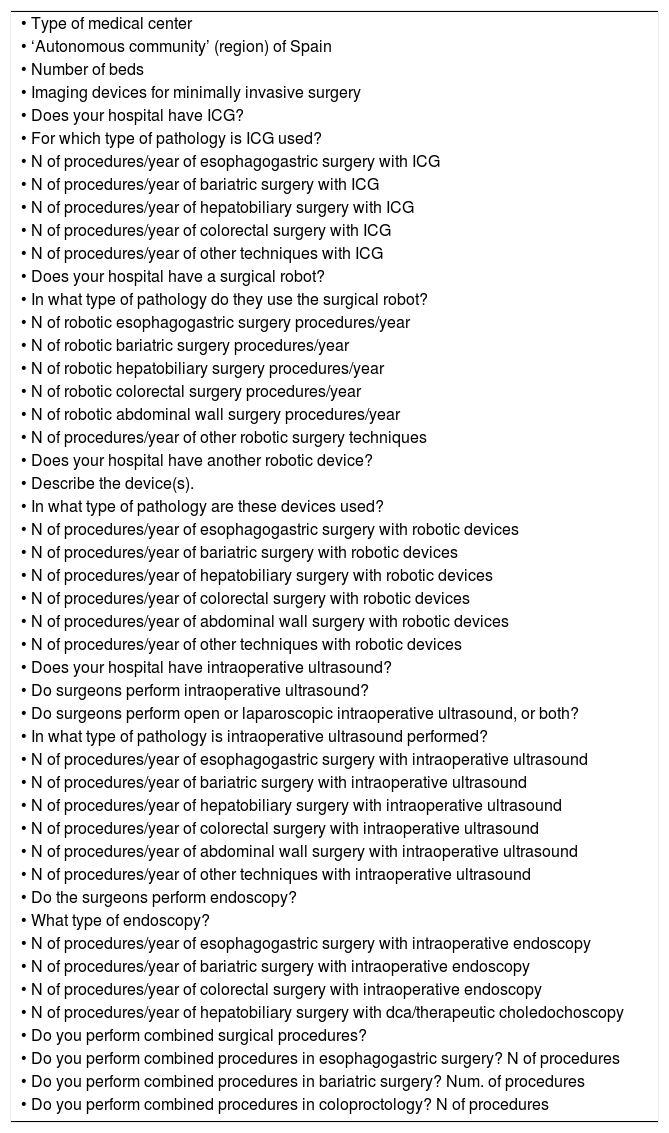
The survey consisted of a 48-item questionnaire (Table 1), divided into eight different sections: type of hospital management, type of imaging devices, use of indocyanine green (ICG), robotic surgery, surgery with robotic devices, intraoperative ultrasound, intraoperative endoscopy and combined surgery. The sections of the survey evaluated the technology available at each hospital, its utilization for different pathologies, and the procedures in which this technology is used.
Questionnaire sent to the participants to evaluate the technological implementation in General and Digestive Surgery services in Spain; survey questions.
| • Type of medical center |
| • ‘Autonomous community’ (region) of Spain |
| • Number of beds |
| • Imaging devices for minimally invasive surgery |
| • Does your hospital have ICG? |
| • For which type of pathology is ICG used? |
| • N of procedures/year of esophagogastric surgery with ICG |
| • N of procedures/year of bariatric surgery with ICG |
| • N of procedures/year of hepatobiliary surgery with ICG |
| • N of procedures/year of colorectal surgery with ICG |
| • N of procedures/year of other techniques with ICG |
| • Does your hospital have a surgical robot? |
| • In what type of pathology do they use the surgical robot? |
| • N of robotic esophagogastric surgery procedures/year |
| • N of robotic bariatric surgery procedures/year |
| • N of robotic hepatobiliary surgery procedures/year |
| • N of robotic colorectal surgery procedures/year |
| • N of robotic abdominal wall surgery procedures/year |
| • N of procedures/year of other robotic surgery techniques |
| • Does your hospital have another robotic device? |
| • Describe the device(s). |
| • In what type of pathology are these devices used? |
| • N of procedures/year of esophagogastric surgery with robotic devices |
| • N of procedures/year of bariatric surgery with robotic devices |
| • N of procedures/year of hepatobiliary surgery with robotic devices |
| • N of procedures/year of colorectal surgery with robotic devices |
| • N of procedures/year of abdominal wall surgery with robotic devices |
| • N of procedures/year of other techniques with robotic devices |
| • Does your hospital have intraoperative ultrasound? |
| • Do surgeons perform intraoperative ultrasound? |
| • Do surgeons perform open or laparoscopic intraoperative ultrasound, or both? |
| • In what type of pathology is intraoperative ultrasound performed? |
| • N of procedures/year of esophagogastric surgery with intraoperative ultrasound |
| • N of procedures/year of bariatric surgery with intraoperative ultrasound |
| • N of procedures/year of hepatobiliary surgery with intraoperative ultrasound |
| • N of procedures/year of colorectal surgery with intraoperative ultrasound |
| • N of procedures/year of abdominal wall surgery with intraoperative ultrasound |
| • N of procedures/year of other techniques with intraoperative ultrasound |
| • Do the surgeons perform endoscopy? |
| • What type of endoscopy? |
| • N of procedures/year of esophagogastric surgery with intraoperative endoscopy |
| • N of procedures/year of bariatric surgery with intraoperative endoscopy |
| • N of procedures/year of colorectal surgery with intraoperative endoscopy |
| • N of procedures/year of hepatobiliary surgery with dca/therapeutic choledochoscopy |
| • Do you perform combined surgical procedures? |
| • Do you perform combined procedures in esophagogastric surgery? N of procedures |
| • Do you perform combined procedures in bariatric surgery? Num. of procedures |
| • Do you perform combined procedures in coloproctology? N of procedures |
ICG: indocyanine green.
The questionnaire was sent to 220 heads of surgery departments at 220 hospitals in Spain.
Differences in responses were evaluated using the two-sided Fisher exact test for categorical variables and the SPSS program version 19.0 (IBM Corp., Armonk, NY, USA).
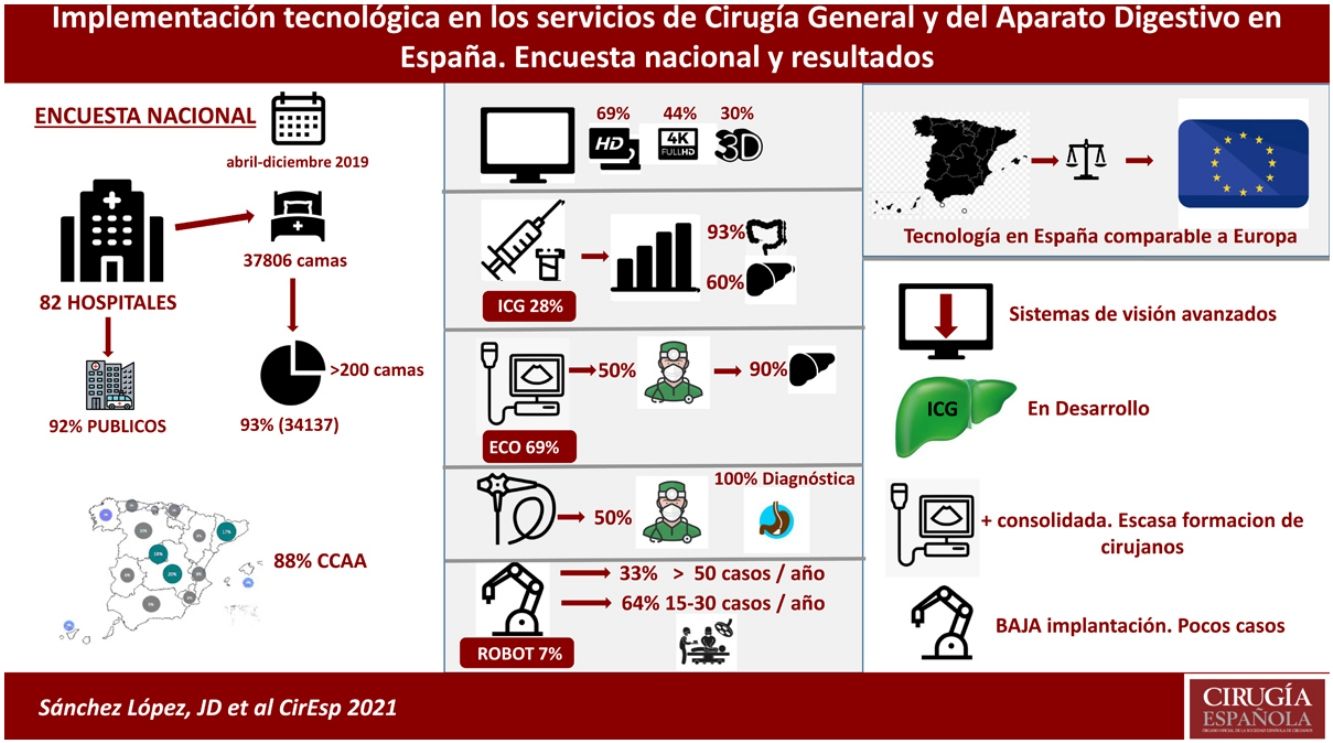
ResultsA total of 82 hospitals (37% of those who were sent the survey) responded to the questionnaire between April and December, 2019. The percentage of completion of the questionnaire among those who responded was 100%.
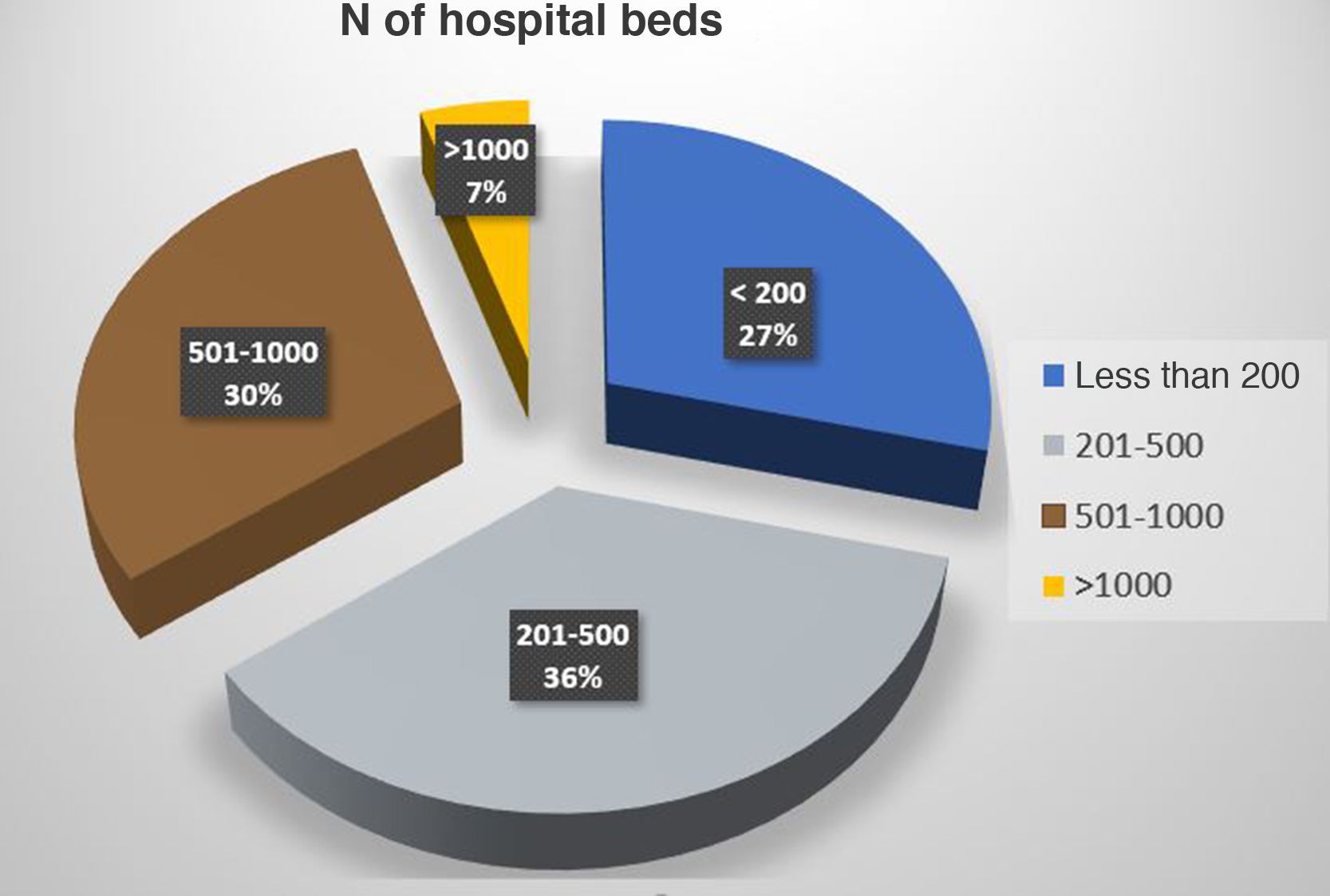
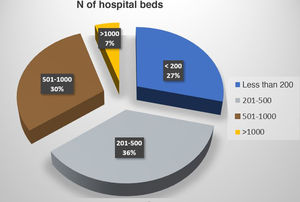
The number of hospital beds represented by the 82 hospitals is 37 806. Some 93% of the total beds (34 137) represent hospitals with more than 200 beds, and 66% represent medical centers with 300 or more hospital beds. The median number of beds in the surveyed hospitals was 403 (Fig. 1)
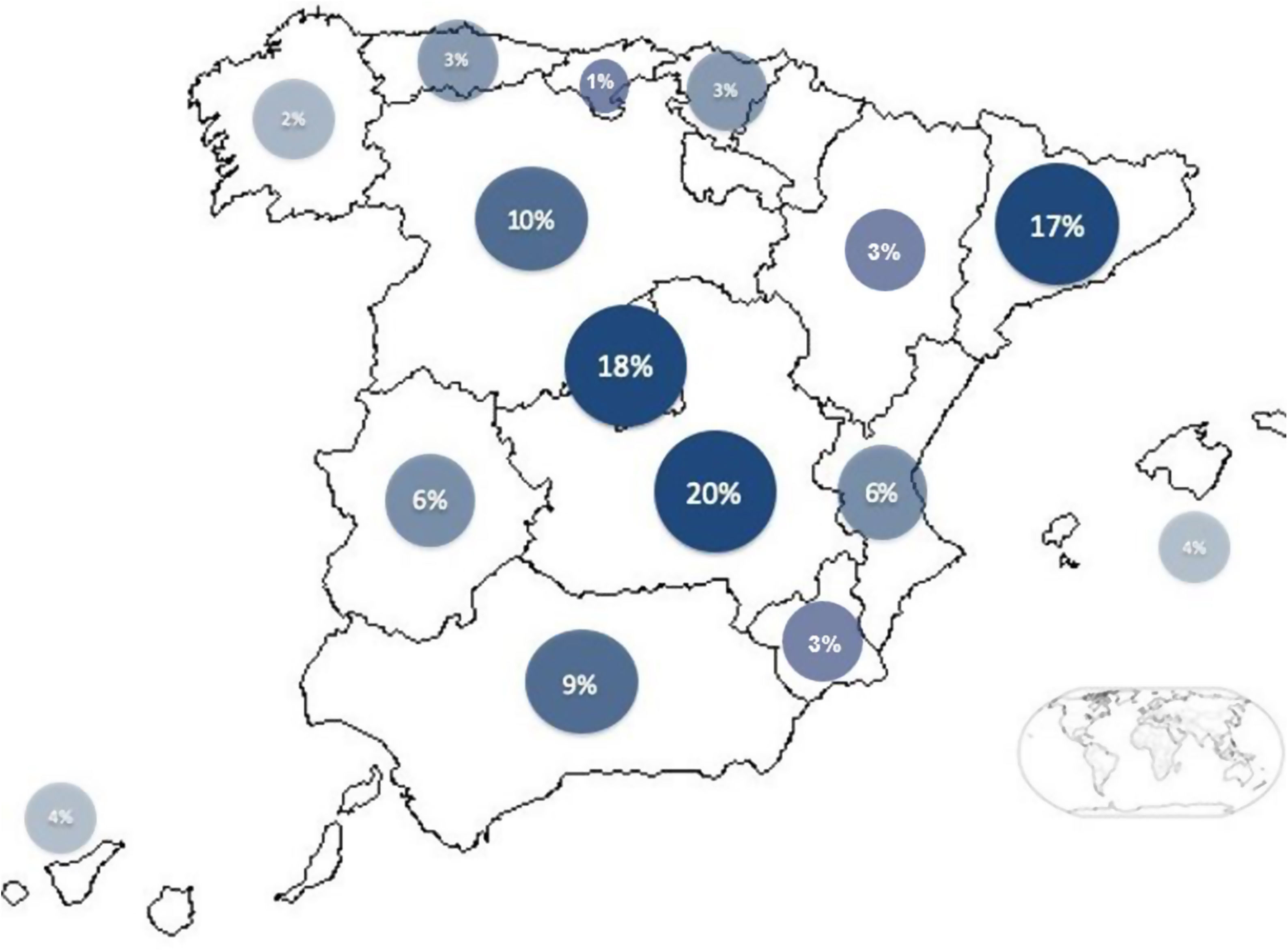
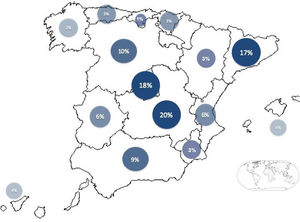
Fig. 2 shows the geographical distribution of participants by Spanish ‘autonomous community’ (region); 88% of the autonomous communities of our country were represented in the survey.
Regarding the management system of the hospitals that completed the survey, 92% are public, 7% are public but privately managed, and 1% are private.
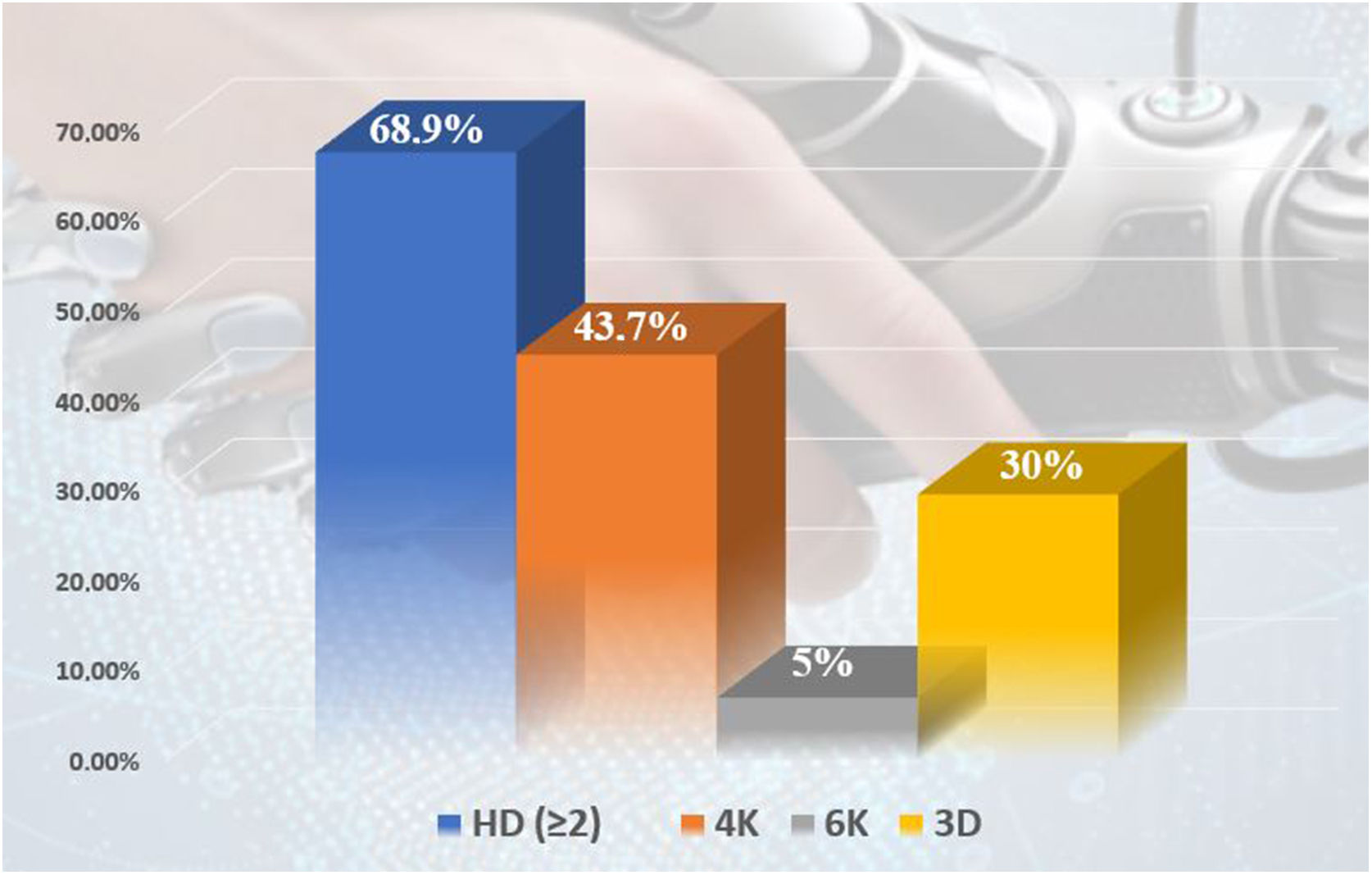
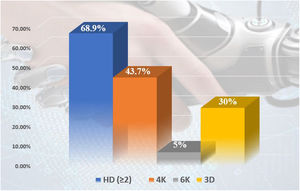
As for the access to imaging devices for minimally invasive surgery (MIS), 68.9% of these medical centers have two or more high-definition (HD) devices, but 56.3% of the hospitals do not have any 4K equipment, and only 4 medical centers (5%) have 6K equipment. As for 3D, only 29.6% of the centers have a device with this image format, while 63.8% of the centers still use even older technology (Fig. 3).
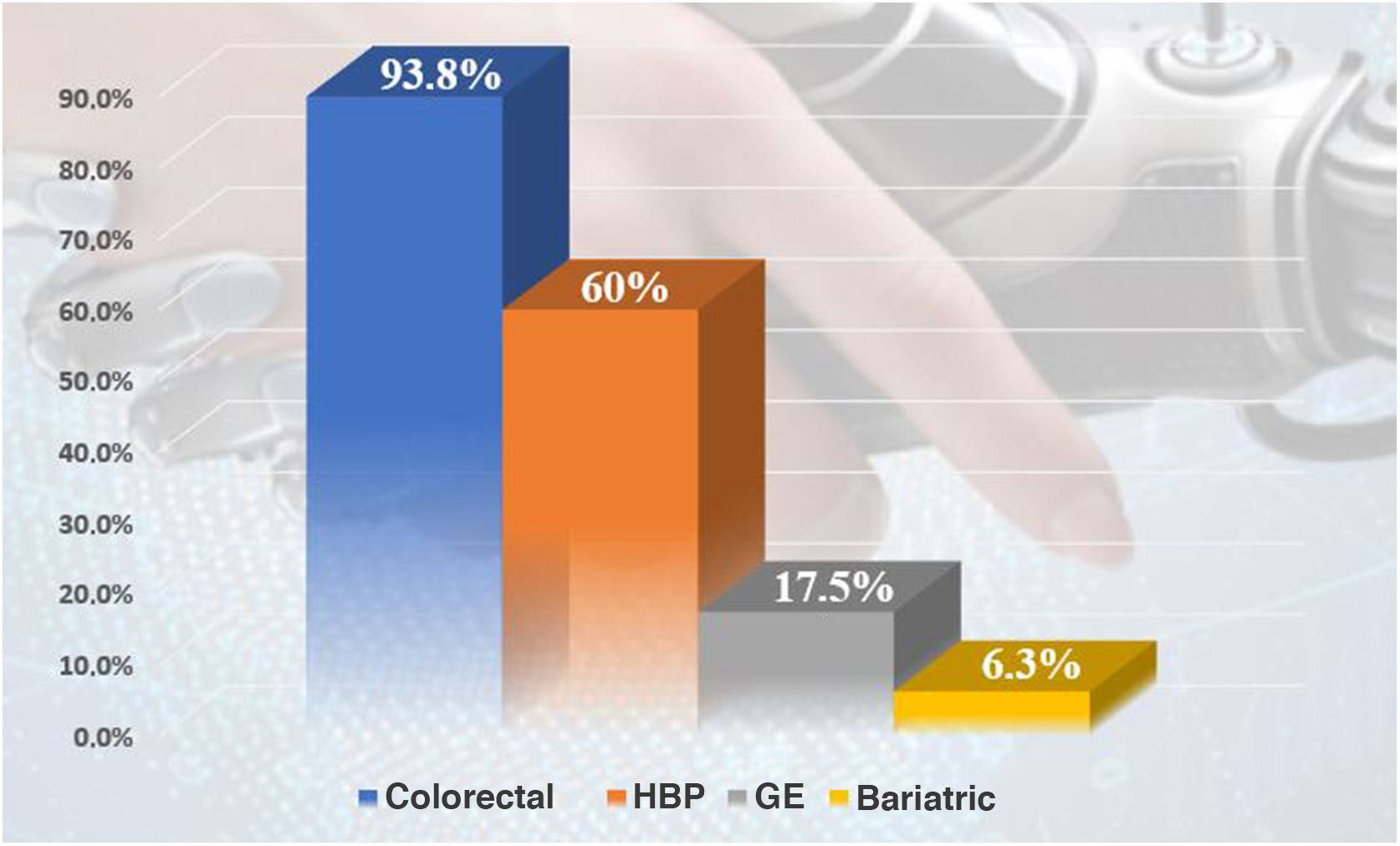
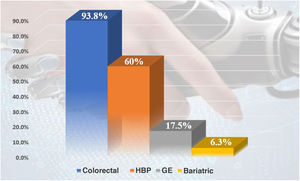
As for ICG, 20 of the 82 surveyed hospitals (28.2%) have this resource and use it regularly; 5.6% have ICG, but do not use it regularly. Among those who have it, 93.8% apply it in colorectal surgery and 60% for hepatobiliary-pancreatic surgery (HBP) (Fig. 4). Regarding esophagogastric surgery, 7 hospitals (35%) use it in more than 10 procedures per year, a percentage that drops to 5% in the case of bariatric surgery. However, in BPH surgery, it is used more than 10 times/year in 50% of the medical centers, and in colorectal surgery 80% of the centers use it in more than 10 surgeries per year (7 centers use it in more than 100 procedures/year).
69% of the surgery services (57 hospitals) have intraoperative ultrasound, and in 50% of the cases it is the surgeon who performs it. In 60%, it is used both in laparoscopic surgery and in open surgery, while in 36% of the centers it is only used in open surgery. In 90% of cases, it is used for BPH surgery, 6.3% for colorectal surgery, 4.2% for esophagogastric surgery and 12.7% for other pathologies, mainly breast surgery. In 70% of the hospitals where it is used in BPH surgery, more than 15 procedures/year are performed with intraoperative ultrasound.
Six hospitals that answered the questionnaire have a surgical robot (7.3%), and 2 have one in their center, but do not use it. Meanwhile, 100% of the services that use the robot do so in colorectal surgery, and 25.8% use it for bariatric surgery (more than 15 cases/year). Among the hospitals where the surgical robot is available and used, 66% perform more than 15 colorectal surgery procedures/year, and 33% perform more than 50 procedures/year. In none of the centers that responded to the survey is it used for abdominal wall surgery.
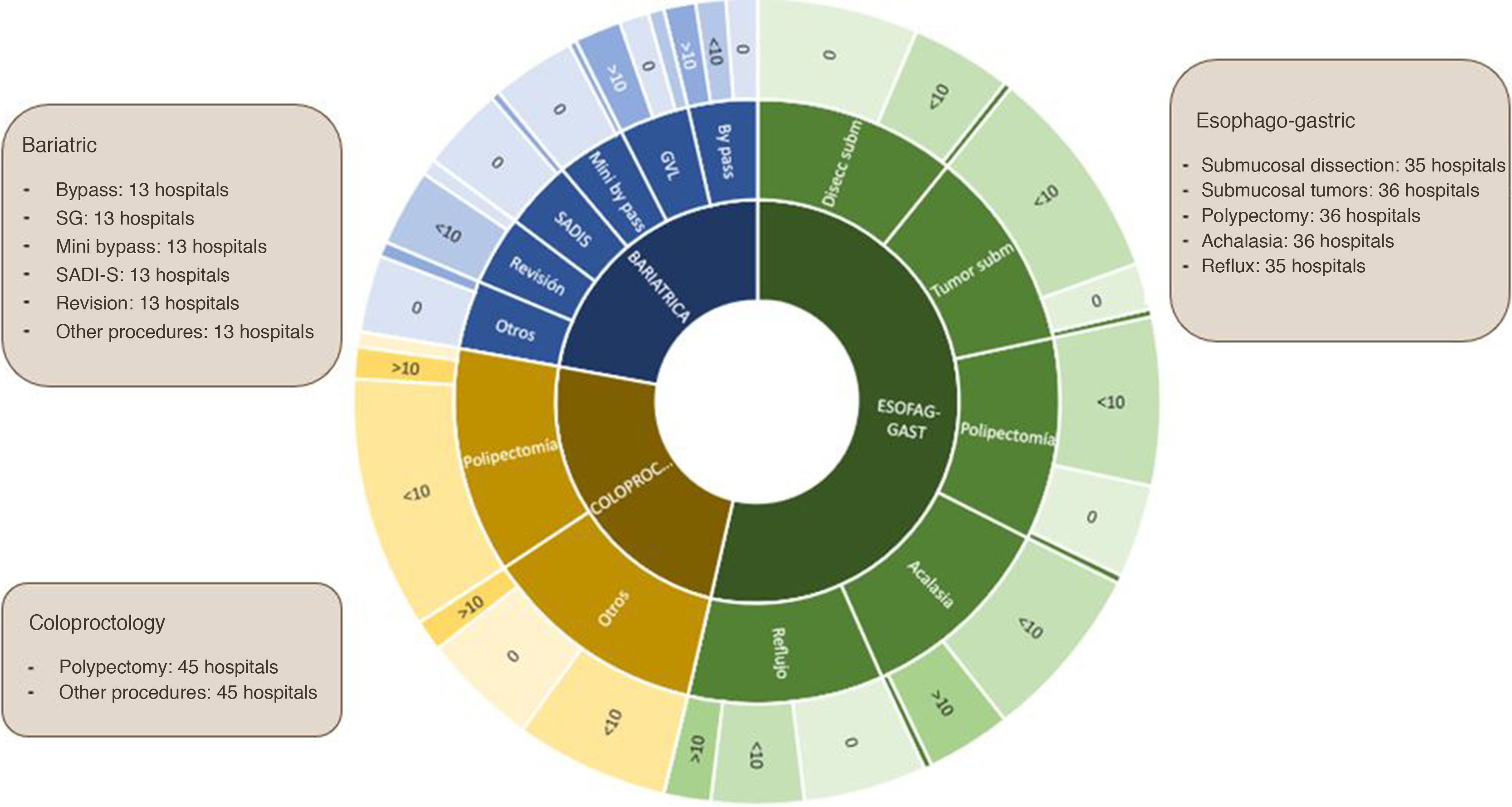
In most hospitals (69%), surgeons do not perform endoscopy, although in 66% of centers endoscopy is used for combined procedures. In the hospitals where it is used by surgeons, it is used for diagnosis by all, including 82% during the intraoperative period and in 70% also outside the operating room. In 35% of hospitals, it is used for intraoperative therapy, in 30.7% for diagnostic choledochoscopy and only in two centers for therapeutic choledochoscopy. In hospitals where intraoperative endoscopy is used for colorectal surgery, in 40% it is used in more than 15 procedures/year. The most commonly performed combination treatments are the resection of polyps in colorectal surgery or esophagogastric surgery, as well as assistance in or revision of bariatric surgery (Fig. 5).
Five medical centers (6%) have used other robotic devices (robotic arms for camera support, robotic instruments, robotic endocutters), mainly for esophagogastric and bariatric surgery, although in some centers they have been tested in all fields. Although they are used in few hospitals, more than 10 procedures are carried out using these devices.
DiscussionThis study shows that the implementation of new technologies in surgery is low. According to the respondents, there is an asymmetric implementation of vision systems (44.7% of the hospitals with 4K technology), less than one-third of hospitals have ICG, and only 7.3% have a robotic device. Intraoperative ultrasound is carried out in half of the centers and in only 31% are endoscopies performed by surgeons.
This is the first study to evaluate the real situation of innovation and the presence of new technologies in the surgical services in Spain.
The number of hospital beds represented by the hospitals that completed the survey was 37 806 out of the 112 000 of the National Catalog of Hospitals 20194, so the sample obtained represents 33.7% of the total hospital beds of the entire national territory. In addition, 92% of the respondents represented public hospitals, the majority of which had more than 300 beds, so the results obtained can fairly faithfully reflect the implementation in our country, as medium and large hospitals usually have more technology available.
The utilization of vision systems is asymmetric. HD is more widely implemented, but only 43.7% of surgery services have 4K devices and 30% 3D devices, while the majority (63.8%) use even older technology. Although the innovations in imaging quality initially encountered some skepticism, many studies have since shown their advantages over 2D technology, where better image quality leads to a more precise execution of surgical procedures and visualization of key elements provides better results5–7. Furthermore, this entails a significant reduction in unnecessary movements and errors, helping to reduce surgical time and increase the safety of interventions8. Although the costs/economic consequences of vision systems have not been evaluated, the constant increase in laparoscopic surgery means that a more efficient use of operating rooms and a reduction in postoperative morbidity and mortality leads to a significant reduction in costs and greater patient satisfaction, which could offset any excess cost that these represent9,10.
Indocyanine green fluorescence (ICG) is being used in the different subspecialties of gastrointestinal surgery. According to the results of this survey, although 28% of hospitals have ICG, only 5.6% use it regularly in surgical practice, mainly in colorectal surgery (more than 10 cases/year in 80%), HBP surgery (more than 10 cases/year in 50%) and esophagogastric surgery (more than 10 cases/year in 35%). The results of different meta-analyses on the use of ICG in these settings are promising, and although it seems a feasible technique, doubts remain about basic aspects of its interpretation, such as dose, times and objective measurement systems11–13. Perhaps this initial stage of its results, associated with the need for light sources, optics and camera systems specially adapted to fluorescence, mean that its implementation in our country is still limited.
Intraoperative ultrasound is a highly sensitive and specific diagnostic tool that provides real-time diagnosis and requires manageable equipment at an affordable price. The performance of intraoperative ultrasound by the surgeon has noticeably increased in recent years, being more prominent in thyroid and parathyroid surgery, breast surgery, and in open and laparoscopic hepatobiliary surgery14–16. This resource is available for 69% of the services surveyed, and an outstanding fact is that in half of the cases it is the surgeon who performs the intraoperative ultrasound, especially in hepatobiliary surgery.
The renewed interest in MIS of the abdominal wall (extraperitoneal approaches, separation of components and anesthetic blocks) is probably a future focus of interest for surgeons who intend to apply intraoperative ultrasound as a complement to their surgical practice17.
Although intraoperative endoscopy (IOE) is very useful when incorporated into surgical teams18, the low usage of endoscopy in surgeons’ daily practice in our setting is remarkable, despite the great impact that surgeons have had on the development of flexible endoscopy19. In 69% of Spanish hospitals, surgeons do not perform endoscopy. This is in contrast with other countries such as Canada, where the surgeon is responsible for flexible endoscopy on a regular basis20, or the United States, where, especially in rural communities, 74% of surgeons perform more than 50 flexible endoscopies/year, and 42% of surgeons perform more than 200 endoscopies/year21.
In our country, 66% of the services surveyed use IOE for combined procedures. However, only 31% of surgical teams perform their own endoscopies and in all cases for diagnosis (82% intraoperative and 18% outside the operating room for pre- or postoperative follow-up). Despite performing fewer procedures than gastroenterologists, endoscopy in the hands of the surgeon is safe and effective22 and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) and the American Board of Surgery (ABS) have developed a specific curriculum to improve flexible endoscopy training for surgical residents. In Spain, and despite the BOE stating that surgical residents “…must acquire knowledge and skills in fibrogastroscopy, endoscopic retrograde cholangiopancreatography (ERCP), fibrocolonoscopy and rectoscopy”, there is no program similar to the US system that guarantees acquiring these skills23.
In a certain asymmetrical way, the surgical robot is being implemented faster than the appearance of scientific evidence about its advantages over conventional surgery, even despite its current major drawback —its cost24,25. Compared to conventional laparoscopy, robotic surgery provides an immersive 3D view, greater instrument maneuverability, better ergonomics, lack of tremor, and other advantages26. Despite this, there is still no robust scientific evidence that supports its superior patient results compared to conventional laparoscopy27,28. Even so, its implementation has experienced exponential growth in the last decade. In mid-2018, there were 4600 units of the Da Vinci robotic platform installed in 66 countries around the world; currently, the global figure is close to 6000 devices. In our country, there were 46 units in 2018, making Spain one of the top five European countries with the largest number of Da Vinci robots installed, together with Germany, Italy, the United Kingdom and France. By October 2020, there were already 68 Da Vinci robots installed in Spain (18 in Catalonia, 14 in Madrid, 9 in Andalusia, 6 in the Basque Country, 5 in Castilla y León, 4 in Valencia, 4 in the Canary Islands, 3 in Galicia, 2 in Cantabria, one in Asturias, one in Navarra and one in the Balearic Islands). Out of the 82 hospitals that responded to our survey, 8 have a surgical robot (9.7%), 2 of which are not used by the surgery service.
According to the data results of this survey, around one-third of the surgical services that use the surgical robot perform more than 50 procedures per year. Coloproctology and bariatric surgery perform a greater volume of robotic surgeries, since 100% of the services that have the robot use it in colorectal surgery and 25.8% for bariatric surgery with more than 15 cases/year. In Germany, a specific national survey about the use of robotics showed a significant increase in procedures in recent years, although the authors consider robotic surgery to still be in its initial phase29. This situation could be identical to the evolution in Spain, although it is impressive to find ourselves in a more initial phase of this upward curve. However, we do not have a survey that specifically targets robotic surgery centers in our country to be able to extrapolate parallel results.
In studies about different general and digestive surgical techniques, we have repeatedly observed how the increased surgical time and the direct costs (platform, material and maintenance) are the two main factors that currently slow down the speed of expansion of robotic surgery in our hospitals. Despite this, the evident advantages that this technology offers in the development of procedures and their results promote the continuous advancement of the system itself and the extension of the number and variety of applications in our specialty30–35.
In this context, the development of new alternative devices to the current Da Vinci system is noteworthy, including robotic instruments that can provide some of the advantages of the Da Vinci, without the limiting factor of its high pricetag36. Currently, only 5 of the hospitals that completed the survey report having and using robotic instruments for MIS. It remains to be seen whether this type of device will be used prominently in the surgery services of our country in the future.
In conclusion, the results of this study allow us to affirm that the implementation of technology in surgical services in our country reflects a situation similar to that of other European countries in terms of the availability and utilization of technological resources.
HD vision systems are solidly established, but the presence of other more advanced options is modest. The use of ICG in surgical procedures is still very limited; there are few hospitals with a high volume of cases, and its use is especially focused on colorectal surgery.
As for the surgical robot, its implementation is low, and few hospitals have accumulated a high number of cases. The current scientific evidence does not show clear advantages from a clinical standpoint, and the financial cost is presented as the main obstacle to its expansion. The announced launch of new robotic platforms with a possibly lower purchase price and/or maintenance costs may be a determining factor in the implementation of surgical robots in our healthcare system.
The use of intraoperative ultrasound and endoscopy as adjunctive tools to surgical practice is not widespread. Although included in the training program of our specialty, it seems necessary to promote specific training programs to ensure adequate knowledge of these techniques among surgeons for their systematic use.
The present study indicates a starting point in the evaluation of the technological preparedness and application of these devices in the different surgical services of our country and demonstrates a significant margin for improvement.
Most of the techniques and technologies presented have been shown to provide benefits for surgical patients. The challenge of scientific societies is to promote training, research and implementation of these technologies in our healthcare system.
Conflict of interestsThe authors have no conflict of interests to declare.
The authors would like to thank the members of the Minimally Invasive Surgery and Technological Innovation Division (Sección de Cirugía Mínimamente Invasiva e Innovación Tecnológica) as well as the Board of Directors of the Spanish Association of Surgeons (Asociación Española de Cirujanos, AEC) for their support in this initiative. Thanks also go to all the surgeons who participated in this survey.
Members of the Minimally Invasive Surgery and Technological Innovation Division (Sección de Cirugía Mínimamente Invasiva e Innovación Tecnológica) of the Spanish Association of Surgeons (Asociación Española de Cirujanos, AEC) who collaborated with this study: Carmen Cagigas Fernández, Iván J. Arteaga González, Dulce Momblan García, Manuel Lozano Gómez, Juan Bellido Luque, and J. Ignacio Rodríguez García.
Members of the Minimally Invasive Surgery and Technological Innovation Division (Sección de Cirugía Mínimamente Invasiva e Innovación Tecnológica) of the Spanish Association of Surgeons (Asociación Española de Cirujanos, AEC) who collaborated with this study: Carmen Cagigas Fernández, Iván J. Arteaga González, Dulce Momblan García, Manuel Lozano Gómez, Juan Bellido Luque, and J. Ignacio Rodríguez García.
Please cite this article as: Sánchez López JD, Acosta Mérida MA, Toledano Trincado M, Segura Sampedro JJ, Trébol López J, Aranzana Gómez A, et al. Implementación tecnológica en los servicios de Cirugía General y del Aparato Digestivo en España. Encuesta nacional y resultados. Cir Esp. 2021;99:707–715.