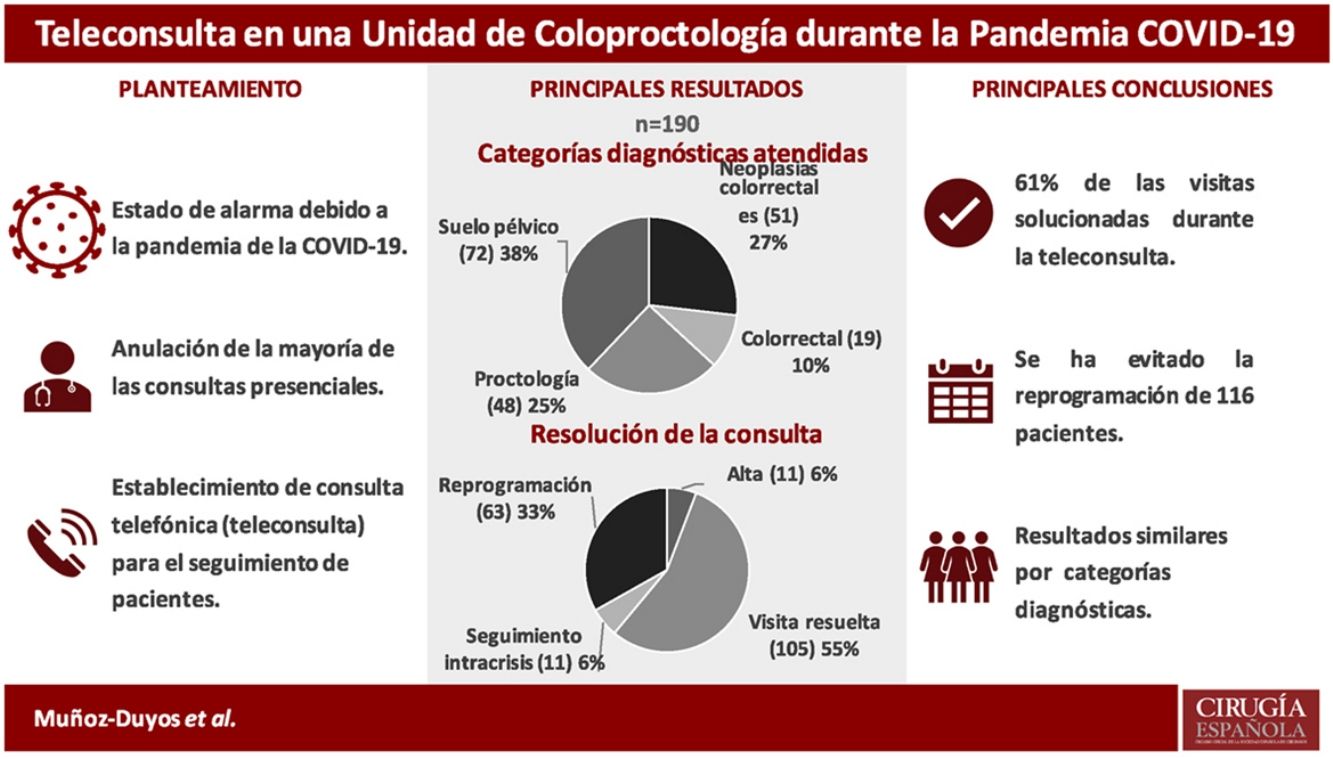
During the state of alarm established in Spain due to the COVID-19 pandemic, most of the face-to-face outpatient consultations were cancelled and a telephone consultation was established to follow up coloproctological patients. The objective of this study was to analyse the efficacy of telemedicine (by telephone) in monitoring patients in a coloproctology unit, in the context of the COVID-19 pandemic.
MethodProspective descriptive study of consecutive patients in a single centre. The result of the teleconsultation was classified as discharge, resolved visit or reprogramming and was analysed by different diagnostic groups.
ResultsFrom March 19th to April 17th, 2020, the teleconsultation of 190 patients was carried out. The response rate was 94.2% (179). The diagnostic categories of the patients attended were: 51 (26.9%) colorectal neoplasia, 48 (25.3%) proctological pathology, 72 (37.9%) pelvic floor dysfunctions and 19 (10%) other benign pathologies. 105 (55.26%) could be recited as if they had come in person. Eleven (5.8%) patients were discharged. No significant differences were found between the different diagnostic categories and the resolution of the teleconsultation. The reasons for reprogramming are analyzed in the study.
ConclusionIn the context of a pandemic, teleconsultation has allowed 61% of follow-up visits to be definitively solved, avoiding the reprogramming of 116 patients. The new social and health paradigm after the pandemic will require a rethinking of our healthcare model, and in many aspects, telemedicine can offer tools for this.
Durante el estado de alarma sanitaria establecido a causa de la pandemia de la COVID-19 se anularon la mayor parte de las consultas externas presenciales y se estableció una consulta telefónica para el seguimiento de pacientes coloproctológicos. El objetivo de este estudio fue analizar la eficacia de la consulta telefónica (teleconsulta) en el seguimiento de los pacientes de una unidad de coloproctología, en el contexto de la pandemia de COVID-19.
MétodoEstudio descriptivo prospectivo de pacientes consecutivos en un solo centro. Se clasificó el resultado de la teleconsulta como alta, visita resuelta o reprogramación y se analizó por diferentes grupos diagnósticos.
ResultadosDel 19 de marzo al 17 de abril de 2020 se realizó la teleconsulta de 190 pacientes. La tasa de respuesta fue del 94,2% (179). Las categorías diagnósticas de los pacientes atendidos fueron: 51 (26,9%) neoplasia colorrectal, 48 (25,3%) enfermedad proctológica, 72 (37,9%) disfunciones del suelo pélvico y 19 (10%) otras enfermedades benignas. Se pudo volver a citar a 105 (55,26%) como si hubieran venido de forma presencial. Se dio el alta a 11 (5,8%) pacientes. No se encontraron diferencias significativas entre las distintas categorías diagnósticas y la resolución de la teleconsulta. Los motivos de reprogramación se analizan en el estudio.
ConclusiónEn el contexto de pandemia, la teleconsulta ha permitido resolver de forma definitiva el 61% de las visitas de seguimiento y ha evitado la reprogramación de 116 pacientes. El nuevo paradigma social y sanitario tras la pandemia requerirá un replanteamiento de nuestro modelo de atención sanitaria y, en muchos aspectos, la telemedicina puede ofrecer herramientas para ello.
Since its inception in the 1950s, telemedicine has expanded exponentially.1 Its use as a tool for patient care has advanced in recent years in various medical2–7 and surgical8–12 specialties. It has been implemented in elderly patients13 and pediatric populations,14,15 as well as to treat patients in remote rural areas.16
A recent review on the use of telemedicine in the surgical field highlights its benefits in reducing absences from work, travel time, costs, and accessibility to health services for people with reduced mobility.17 Recently, the experience in postoperative follow-up by videoconference in a general surgery service in our setting has been published.18
The usefulness of telemedicine in responding to natural disasters has previously been reported.19,20 The COVID-19 pandemic has necessitated the application of telemedicine systems in several countries, and their use has already been reported in different specialties21–29 or fields that, a priori, require in-person treatment, such as rehabilitation.30
In our country, the pandemic caused a ‘state of alarm’ to be declared on March 14, 2020. This situation put great pressure on healthcare systems and has required reorganization to minimize in-person consultations.
The objective of this study is to analyze the effectiveness of telephone consultations (teleconsultation) in the follow-up of patients treated by a coloproctology unit, in the context of the COVID-19 pandemic.
MethodsWe conducted a prospective, descriptive study of consecutive patients who had a previously scheduled follow-up appointment with the coloproctology unit of our public hospital during the COVID-19 pandemic. Patients who did not agree to participate in the study, or who were not capable of comprehending it, were excluded.
The telephone appointment first involved locating all scheduled patients. Those who did not answer were called up to 3 times at different times and, if they could not be contacted, the calls were rescheduled. During that call, we explained to patients that they could not be seen in person, and the consultation was carried out over the phone. The study protocol was completed, with the patient’s oral consent, and an annotation was made in the hospital’s computer system, as is done in person.
This study was approved by the Ethics Committee of the hospital, and patients gave their informed consent both to enter the study and for their data to be used.
Most patients with anal fistula were not included in the study because they are monitored in a specific consultation that involves an ultrasound follow-up. Similarly, patients with hemorrhoidal disease are monitored and treated in a specific consultation, with the ability to perform rubber band ligation on an outpatient basis. These patients, who require invasive examinations, were called by the secretary to explain that the consultation would be rescheduled at the end of the crisis. Meanwhile, they were able to contact the unit if their condition worsened.
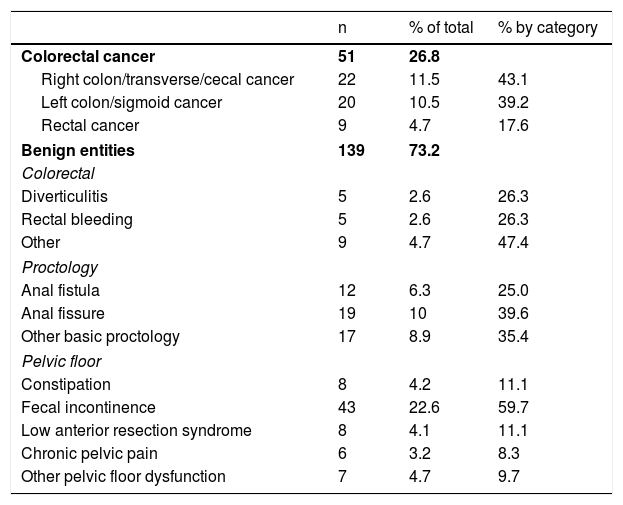
The diagnoses of the patients were classified into different categories (Table 1). Functional diseases included pelvic floor conditions, except rectal prolapse and rectoceles; the remainder were considered structural diseases.
Diagnoses of patients treated during the study.
| n | % of total | % by category | |
|---|---|---|---|
| Colorectal cancer | 51 | 26.8 | |
| Right colon/transverse/cecal cancer | 22 | 11.5 | 43.1 |
| Left colon/sigmoid cancer | 20 | 10.5 | 39.2 |
| Rectal cancer | 9 | 4.7 | 17.6 |
| Benign entities | 139 | 73.2 | |
| Colorectal | |||
| Diverticulitis | 5 | 2.6 | 26.3 |
| Rectal bleeding | 5 | 2.6 | 26.3 |
| Other | 9 | 4.7 | 47.4 |
| Proctology | |||
| Anal fistula | 12 | 6.3 | 25.0 |
| Anal fissure | 19 | 10 | 39.6 |
| Other basic proctology | 17 | 8.9 | 35.4 |
| Pelvic floor | |||
| Constipation | 8 | 4.2 | 11.1 |
| Fecal incontinence | 43 | 22.6 | 59.7 |
| Low anterior resection syndrome | 8 | 4.1 | 11.1 |
| Chronic pelvic pain | 6 | 3.2 | 8.3 |
| Other pelvic floor dysfunction | 7 | 4.7 | 9.7 |
The results of the consultations were defined as: 1) resolved consultation: the attention was equivalent to an in-person appointment; 2) definitive discharge; 3) intra-crisis follow-up: one or more consecutive visits were required within the study period; and 4) rescheduling: if the patient required an in-person office visit at the end of the crisis.
ObjectivesThe aim of the study was to analyze the effectiveness of teleconsultation. This objective was broken down as follows: 1) study how many patients are resolved in the teleconsultation, and calculate the median time until a new appointment; 2) determine how many patients are pending rescheduling and the reasons for rescheduling; 3) study how many patients are discharged; 4) analyze how the follow-up and care of patients pending surgery have been carried out; and 5) investigate whether there are resolution differences between the different diagnostic groups.
Statistical analysisThe quantitative variables are reported with median and range, and the qualitative variables are reported with absolute and relative frequencies. The Mann–Whitney U test was used to compare the quantitative variables of the independent data, and the Pearson correlation coefficient was used to study the independence between qualitative variables. Associations were considered significant if P ≤ .05. The statistical package used was R version 3.6.1 (2019, The R Foundation for Statistical Computing).
ResultsFrom March 19 to April 17, 2020, 190 patients (106 women) with a mean age of 61.5 years (15–88) had telephone consultations. The distribution of patients by type of consultation was: 123 (64.7%) general coloproctology consultation, and 67 (35.3%) specific pelvic floor consultations. All were called in the context of phases V and IV of the pandemic as defined by the AEC.31
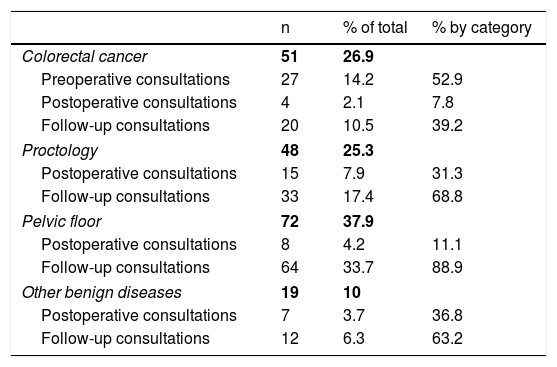
The diagnostic categories and the list of most frequent diagnoses can be seen in Tables 1 and 2. Out of the total number of patients consulted, 34 (17.9%) were called during the immediate postoperative period after either elective or urgent surgery, and 129 (67.9%) were in long-term follow-up. The remaining 27 patients (14.2%) had an active neoplasm pending testing and treatment, representing 52.9% of cancer patients.
Diagnostic categories and types of follow-up of the included patients.
| n | % of total | % by category | |
|---|---|---|---|
| Colorectal cancer | 51 | 26.9 | |
| Preoperative consultations | 27 | 14.2 | 52.9 |
| Postoperative consultations | 4 | 2.1 | 7.8 |
| Follow-up consultations | 20 | 10.5 | 39.2 |
| Proctology | 48 | 25.3 | |
| Postoperative consultations | 15 | 7.9 | 31.3 |
| Follow-up consultations | 33 | 17.4 | 68.8 |
| Pelvic floor | 72 | 37.9 | |
| Postoperative consultations | 8 | 4.2 | 11.1 |
| Follow-up consultations | 64 | 33.7 | 88.9 |
| Other benign diseases | 19 | 10 | |
| Postoperative consultations | 7 | 3.7 | 36.8 |
| Follow-up consultations | 12 | 6.3 | 63.2 |
After 3 separate attempts, 11 patients had not answered the call, which represented a response rate of 94.2% (179). All patients in the immediate postoperative period answered the teleconsultation phone call. The group that answered less frequently was the pelvic floor group: 7/11 (63.6% of calls went unanswered).
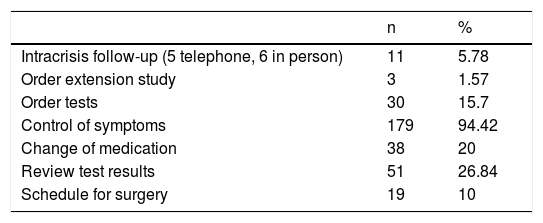
Table 3 summarizes the actions developed during the teleconsultation, the most frequent of which was the follow-up of symptoms, followed by the review of test results.
Out of the 190 patients included, 116 (61%) obtained care that avoided rescheduling, 105 patients (55.25%) were classified as having had a resolved visit, and 11 patients (5.8%) were discharged.
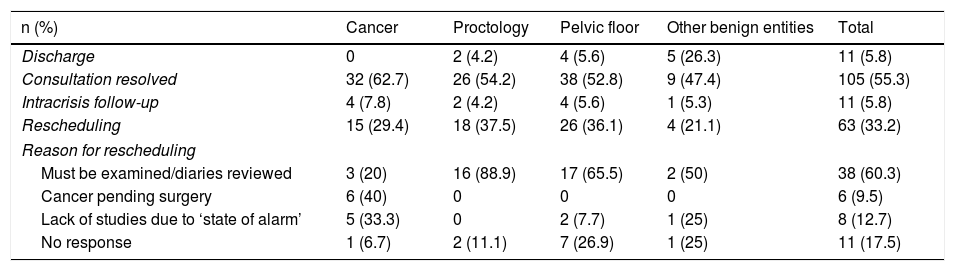
Table 4 shows the distribution frequency by diseases and the resolution of the teleconsultations. Patients with proctological and pelvic floor disease had to be rescheduled more often than cancer patients, without implying significant differences. The description of the discharged patients is shown in Table 5.
Resolution of teleconsultation by diagnostic categories and reasons for rescheduling.
| n (%) | Cancer | Proctology | Pelvic floor | Other benign entities | Total |
|---|---|---|---|---|---|
| Discharge | 0 | 2 (4.2) | 4 (5.6) | 5 (26.3) | 11 (5.8) |
| Consultation resolved | 32 (62.7) | 26 (54.2) | 38 (52.8) | 9 (47.4) | 105 (55.3) |
| Intracrisis follow-up | 4 (7.8) | 2 (4.2) | 4 (5.6) | 1 (5.3) | 11 (5.8) |
| Rescheduling | 15 (29.4) | 18 (37.5) | 26 (36.1) | 4 (21.1) | 63 (33.2) |
| Reason for rescheduling | |||||
| Must be examined/diaries reviewed | 3 (20) | 16 (88.9) | 17 (65.5) | 2 (50) | 38 (60.3) |
| Cancer pending surgery | 6 (40) | 0 | 0 | 0 | 6 (9.5) |
| Lack of studies due to ‘state of alarm’ | 5 (33.3) | 0 | 2 (7.7) | 1 (25) | 8 (12.7) |
| No response | 1 (6.7) | 2 (11.1) | 7 (26.9) | 1 (25) | 11 (17.5) |
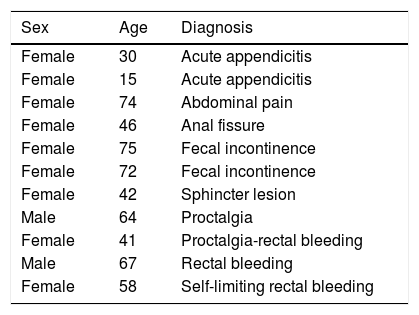
Characteristics of the patients discharged.
| Sex | Age | Diagnosis |
|---|---|---|
| Female | 30 | Acute appendicitis |
| Female | 15 | Acute appendicitis |
| Female | 74 | Abdominal pain |
| Female | 46 | Anal fissure |
| Female | 75 | Fecal incontinence |
| Female | 72 | Fecal incontinence |
| Female | 42 | Sphincter lesion |
| Male | 64 | Proctalgia |
| Female | 41 | Proctalgia-rectal bleeding |
| Male | 67 | Rectal bleeding |
| Female | 58 | Self-limiting rectal bleeding |
The mean time before the next follow-up visit for patients with a resolved consultation was 4 (3–12) months. Twenty-three (25.8%) of the patients required rescheduling 3 months after the teleconsultation, another 23 were scheduled for 4 months later, 36 (40.5%) for 5 or 6 months later, and 7 (7.8%) were scheduled for more than 6 months later. In addition, 19 (10%) patients were not scheduled for another outpatient consultation because they were directly scheduled for surgery: the procedure was explained to them, and they were instructed to sign the consent form in the pre-anesthesia appointment (17 with cancer and 2 patients with incontinence, who were candidates for implantation of a sacral neuromodulation pulse generator).
It was necessary to reschedule 63 (33.2%) patients. The distribution frequency of the reasons for reprogramming is described in Table 4. The main cause was the need to examine the patient or assess defecation diaries (60.3%), which essentially affected the proctology and pelvic floor patients. In the group of cancer patients, it was the lack of studies due to cancellations during the pandemic.
During the teleconsultation, 11 (11.8%) patients were identified as requiring intra-crisis follow-up, 5 of whom had to be called 3 times a week to monitor symptoms of large neoplasms and to assess the need for preferential surgery or colonic stent placement. Through this intra-crisis follow-up and a change in dietary habits, none of the patients required urgent surgery. In addition, 6 postoperative patients had to be monitored in person for various reasons.
The mean telephone consultation time was 6 min (2–15), which was somewhat longer in the coloproctology group due to the concentration of cancer patients, whose appointments lasted 8 min (2–15), versus the pelvic floor consultations, with a duration of 5 min (3–12).
No age differences were found between the patients who were resolved or discharged from the teleconsultation and those who required rescheduling: 63 (15–88) vs 59 (17–87) years (P = .749). Sex was also not a prognostic factor for rescheduling either.
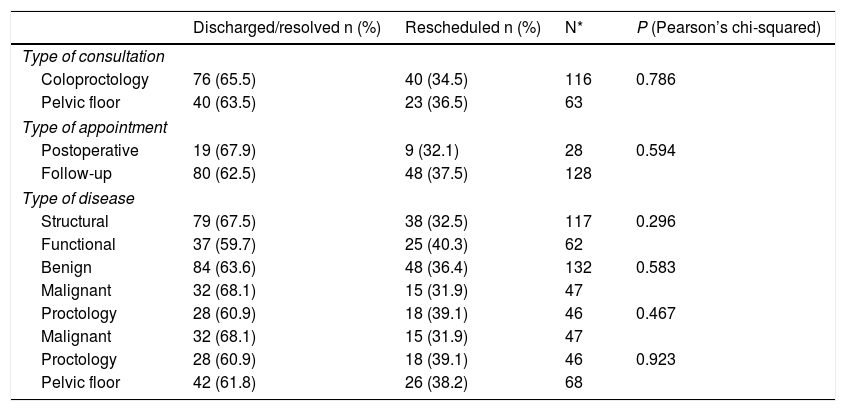
No statistically significant differences were found between the different diagnostic categories or the type of consultation or visit for which the patients were scheduled and the resolution of the teleconsultation (Table 6).
Influence in the diagnostic categories or type of consultation in the resolution of the teleconsultation.
| Discharged/resolved n (%) | Rescheduled n (%) | N* | P (Pearson’s chi-squared) | |
|---|---|---|---|---|
| Type of consultation | ||||
| Coloproctology | 76 (65.5) | 40 (34.5) | 116 | 0.786 |
| Pelvic floor | 40 (63.5) | 23 (36.5) | 63 | |
| Type of appointment | ||||
| Postoperative | 19 (67.9) | 9 (32.1) | 28 | 0.594 |
| Follow-up | 80 (62.5) | 48 (37.5) | 128 | |
| Type of disease | ||||
| Structural | 79 (67.5) | 38 (32.5) | 117 | 0.296 |
| Functional | 37 (59.7) | 25 (40.3) | 62 | |
| Benign | 84 (63.6) | 48 (36.4) | 132 | 0.583 |
| Malignant | 32 (68.1) | 15 (31.9) | 47 | |
| Proctology | 28 (60.9) | 18 (39.1) | 46 | 0.467 |
| Malignant | 32 (68.1) | 15 (31.9) | 47 | |
| Proctology | 28 (60.9) | 18 (39.1) | 46 | 0.923 |
| Pelvic floor | 42 (61.8) | 26 (38.2) | 68 | |
N = 179: for the analysis, patients have been eliminated from the intracrisis follow-up group.
This study shows that, in the context of a pandemic, teleconsultation without video has made it possible to definitively resolve 61% of the follow-up visits that were scheduled in the coloproctology consultations, while avoiding rescheduling for the consultation in 116 patients.
Several studies on the use of telemedicine during the COVID-19 pandemic have already been published. Its effectiveness has been highlighted in aspects as diverse as patient safety26 and healthcare worker safety,29 the identification of early COVID-19 symptoms,32 treatment of patients who show new symptoms and need to be referred to different specialties,25,33–36 or the improved identification of contacts of a patient for epidemiological and pandemic control purposes.37 However, we have not found studies that indicate its usefulness in an outpatient coloproctology consultation already scheduled prior to the pandemic.
In many other departments, the alternative to teleconsultation (as in our unit) has involved the review of patient diagnoses and clinical histories, selecting those patients who absolutely required a phone call or in-person office visit. In addition, the administrative call was necessary to inform patients not to come to the consultation and that the visit would be rescheduled when possible. We believe that systematic teleconsultations and calling all patients without prior selection, when possible, allows surgeons to provide patient care in a pandemic situation in non-priority cases, and especially cancer patients. Likewise, this model facilitates the management of outpatient consultations for 2 reasons: 1) the best time to call the patient and resolved the visit is when the surgeon is reviewing the patient file; and 2) this avoids double calls, and that time can be used to call other patients for first non-oncological visits or coloproctological examinations to inform them that their appointment will be rescheduled.
The situation of home confinement has made the response rate very high. 100% of postoperative patients responded to the teleconsultation, as in most telemedicine studies on postoperative follow-up.8,9,38 The important collaboration and predisposition of patients to have a telephone consultation has undoubtedly been favored by the circumstances, which limits the extrapolation of these results to a normal situation. Another limitation of our study, in terms of extrapolation, is that, due to the organization of our unit, most of the patients with anal fistula or hemorrhoids were not included.
The efficacy rate of our model was lower than the 74% reported in the recent study on the use of videoconferencing in a general surgery consultation,18 which used a meticulous process of selecting patients for teleconsultation. Possibly, the definition of the inclusion criteria for a new healthcare model, given the paradigm shift posed by this pandemic, will allow us to improve its effectiveness.
We did not find differences in the rescheduling rate according to the diagnosis of the patients included. The main limitation in the group of cancer patients was the cancellation of tests during the pandemic; however, it is very possible that these patients could benefit from a new telephone consultation once the complementary examinations were carried out. In the group of patients with proctological and pelvic floor problems, the main limitation was the need to examine them or review defecation diaries, and this will be a persistent limitation in the post-pandemic context that we must bear in mind.
Teleconsultation has made it possible to identify patients who required intra-crisis follow-up and, in addition to visiting postoperative patients who required wound cleaning, it has prevented colon neoplasms with risk of occlusion from needing to be operated on urgently.
Gunter et al. reported a high percentage of affirmative responses when patients were asked whether telemedicine was useful for them in different studies.1 The TUQ questionnaire,39 published in 2016, evaluates the perspective of patients regarding the use of telemedicine, and its validated Spanish version was published this year.40 One weakness of this study is undoubtedly the lack of a protocolized patient satisfaction evaluation.
The use of video platforms in teleconsultation, which is advocated in several studies,41,42 was not possible in our setting. The advantages attributed to this system range from the possibility of seeing the patient’s appearance and increasing empathy, to performing visual physical examination of surgical wounds, for example. However, the need for knowledge and availability of specific material for video-consultation may limit accessibility. Other studies have commented on the selection bias that access to digital platforms may entail.1 A recent study has shown that the older population was more resistant to the use of telemedicine platforms using smartphones.43 Furthermore, we should recognize that the time per visit would be considerably increased by adding images. In an ideal model, it would be possible to determine which patients require eye contact and which other follow-ups may be done over the phone.
With teleconsultation, we have avoided the need to reschedule 116 patients. This consultation time can be used for other patients when external consultation activities are reinitiated post-pandemic, as has been reported in other studies.11 A significant proportion of multi-specialty outpatient visits may be effectively manageable from a distance, and many patients will benefit from telemedicine without compromising their health or quality of care. Furthermore, telemedicine has been shown to reduce healthcare costs by reducing hospital admissions and readmissions.8,12,44,45 However, we must not forget that it will continue to be essential to safeguard the privacy of patients during teleconsultation.
Although there are still certain legal, regulatory and funding challenges to introduce telemedicine into the new healthcare paradigm, the COVID-19 outbreak may be the catalyst for institutions, legislators and regulatory agencies to enact new measures that facilitate its widespread implementation. Perhaps the COVID-19 crisis will transform the healthcare model more than any other crisis in modern history.
Telephone consultations have made it possible to resolve a high percentage of follow-up visits in a coloproctology unit in the context of the COVID-19 pandemic, and no differences were identified between diagnostic categories. The response rate has been very high, and we were able to identify which patients could be followed up sequentially, thereby avoid visits to the emergency department. The new paradigm after the pandemic will require rethinking our healthcare model, and telemedicine will be a tool to consider.
Please cite this article as: Muñoz-Duyos A, Abarca-Alvarado N, Lagares-Tena L, Sobrerroca L, Costa D, Boada M, et al. Teleconsulta en una unidad de coloproctología durante la pandemia de COVID-19. Resultados preliminares. Cir Esp. 2021;99:361–367.