Trocar site hernias are a complication of minimally invasive surgery that are often underestimated. These lesions cause patient discomfort and require surgery for their correction, which increases healthcare costs.
The data available in the literature on the incidence of trocar site hernias in laparoscopic surgery are very variable, ranging from 0.3% to 31.9%.1–5 This complication seems to be more frequent in umbilical trocars compared to other locations outside the midline, and there is speculation that this may be due to the weakness of the abdominal wall in this area, as well as longer incisions and the frequent need to extend the incision for the extraction of the surgical specimen. In recent years, the development of single-incision laparoscopic procedures, which are generally umbilical and require slightly larger incisions than conventional procedures, has raised concerns about long-term safety in terms of wound complications. In this instance, we have found hernia rates reported in the literature ranging from 1% to 8.4% using this approach.6–8
In our group, we have analyzed the incidence of umbilical trocar site hernias in patients undergoing elective cholecystectomy using minimally invasive surgery techniques. A cohort of 108 patients was treated with a multiport approach using a supraumbilical balloon port, and another cohort with 109 patients was treated through a single transumbilical incision. The groups were comparable for different risk factors, such as infection rate, body mass index or incidence of diabetes mellitus. Follow-up was more than 3 years for most patients, during which we observed a high incidence of incisional hernia in both groups (29.6% and 5.5%, respectively), most of which were detected within the first 2 years of follow-up.
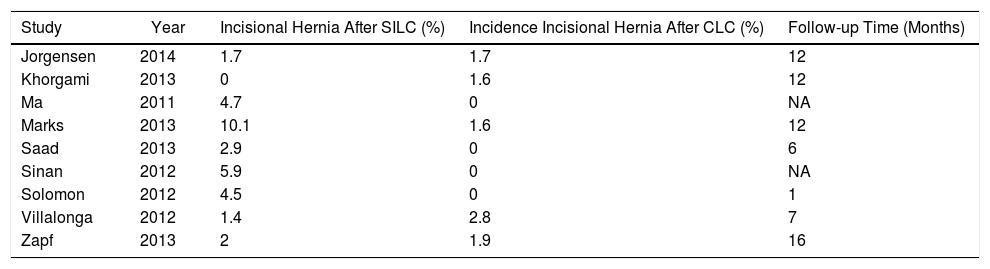
Some authors, such as Marks et al., have compared the incisional hernia rate between multi-port laparoscopic cholecystectomy and single-incision cholecystectomy, finding no differences 3 months after the intervention but observing differences after one year of follow-up, with an incidence of 8.4% in single-incision and 1.2% in conventional laparoscopy.6 Several recently published meta-analyses describe an increased risk of hernia in the single-incision group, although there is great variability in the follow-up between the studies analyzed as well as significant heterogeneity in the technique and material used for the abdominal wall closure7,8 (Table 1). In our series, the incidences of incisional hernias in patients who had undergone single-incision procedures is similar to reports by other authors, so it seems that the difference between the two techniques may be mainly due to the high incidence of incisional hernias in patients with the conventional approach.
Incidence of Incisional Hernia After Single-incision Laparoscopic Cholecystectomy Versus Conventional Laparoscopic Cholecystectomy.
| Study | Year | Incisional Hernia After SILC (%) | Incidence Incisional Hernia After CLC (%) | Follow-up Time (Months) |
|---|---|---|---|---|
| Jorgensen | 2014 | 1.7 | 1.7 | 12 |
| Khorgami | 2013 | 0 | 1.6 | 12 |
| Ma | 2011 | 4.7 | 0 | NA |
| Marks | 2013 | 10.1 | 1.6 | 12 |
| Saad | 2013 | 2.9 | 0 | 6 |
| Sinan | 2012 | 5.9 | 0 | NA |
| Solomon | 2012 | 4.5 | 0 | 1 |
| Villalonga | 2012 | 1.4 | 2.8 | 7 |
| Zapf | 2013 | 2 | 1.9 | 16 |
CLC: conventional laparoscopic cholecystectomy; SILC: single-incision laparoscopic cholecystectomy; NA: not available.
These figures in the multi-port surgery group, although high, are in line with those of other prospective series in cholecystectomized patients after a conventional laparoscopic approach. For instance, the publication by Comajuncosas et al.3 reports the global incidence of umbilical trocar hernia at 25.9% after a mean follow-up of 3 years, while the study by Armañanzas et al.4 reports 31.9% in patients with risk factors for incisional hernia. Incidences that are far from 0.3% to 5.4% are frequently described in the literature,2 leading to maintained interest in this complication and the search for prevention strategies, such as the use of prophylactic prostheses in selected patients.4,9
Several factors have been associated with the appearance of trocar site hernias: some related to the patient, others with the disease being treated, and yet others with technical aspects of the procedure.1–5 In patients undergoing laparoscopic cholecystectomy, these factors include: diabetes, obesity, incision length and surgical site infection.3,5 In our patients, wound infection was associated with a higher risk of incisional hernia, and a slight increase in risk was also observed at higher BMI. In this sense, and although it may be considered something obvious and common to any abdominal wall incision, we should insist on the importance of taking precautions to reduce surgical site infections as part of the strategy for trocar site hernia prevention.
Factors associated with the surgical technique can also influence the appearance of incisional hernias. In our series, the same closure technique was used in all patients (simple interrupted suture, 3–4 stitches at a distance of 0.5cm, using long-lasting absorbable synthetic material), which leads us to believe that others details, such as the type of trocar or the location (supraumbilical versus transumbilical incision), may have contributed to the appearance of these differences.
Trocar site hernias are an important complication whose evaluation requires long-term follow-up. However, the duration of this follow-up does not seem to be the only factor that explains the difference between the low incidences found in most studies and the extremely high incidences observed in others. The study of other risk factors, beyond those associated with the patient, including technical details and the surgical material used, should shed light on this matter and facilitate the implementation of strategies for the prevention of this complication.
Please cite this article as: Rodríguez de Guzmán CA, Morandeira Rivas AJ, Herrero Bogajo ML, Moreno Sanz C. Hernia del orificio del trocar, ¿un problema más frecuente de lo que creemos? Cir Esp. 2019;97:410–411.