Tuberculosis (TB) of the gallbladder is an uncommon disease that was first described by Gaucher in 1870.1 Gallbladder TB can simulate a carcinoma in patients who present with a gallbladder mass.2 The absence of specific clinical signs make the perioperative diagnosis of TB difficult and even more so given the presence of lithiasis, as most symptoms are attributed to the gallstones.3 There are no pathognomonic characteristics for imaging diagnosis, so this medically curable disease is diagnosed by the histology study of the surgical specimen after cholecystectomy.4,5
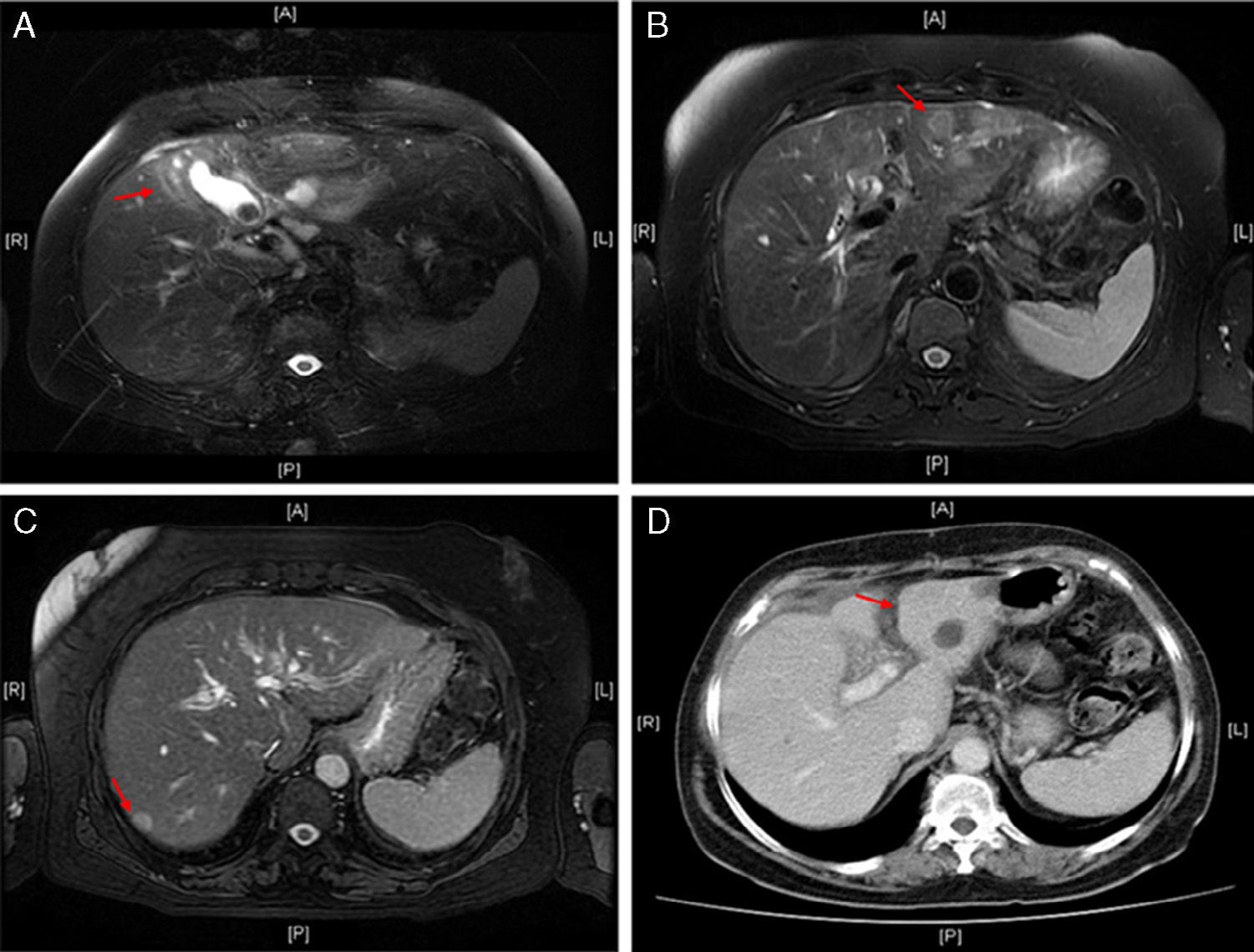
We present the case of a 68-year-old female patient who came to the emergency room with abdominal pain in the right hypochondrium, nausea and vomiting that had started a month before. Her medical history included arterial hypertension, dyslipidemia and type II diabetes mellitus. Physical examination detected jaundice of the skin and mucous membranes and pain in the right hypochondrium. Lab work showed: total bilirubin 6.7mg/dL; direct bilirubin 5.8mg/dL; serum glutamic oxaloacetic transaminase 295U/L; lactate dehydrogenase 715U/L; alkaline phosphatase 242U/L; and gamma-glutamyl transferase 330U/L. Other parameters were normal. Abdominal ultrasound revealed: thickened gallbladder wall with a single gallstone measuring 2.6cm; 2 cystic lesions in segments VI–VII and II; mild dilatation of the intrahepatic bile duct; and, 2 solid hepatic lesions in segments II and VI. The studies were completed with magnetic resonance cholangiopancreatography, which demonstrated irregular thickening of the gallbladder wall with a lithiasis measuring 2.7cm and pathologic contrast uptake, suggestive of gallbladder neoplasm (Fig. 1A), accompanied by dilatation of the intrahepatic bile duct secondary to the impression of the gallbladder neck and 2 solid hepatic lesions in segments II and VI, suggestive of liver metastases (Fig. 1B and C).
(A) Magnetic resonance in T2: irregular thickening of the gallbladder wall with inflammatory changes in the adjacent liver parenchyma; (B) magnetic resonance in T2: nodular lesion in liver segment II; (C) magnetic resonance in T2: nodular lesion in liver segment VI; (D) abdominal CT with contrast: absence of nodular lesion previously described in liver segment II.
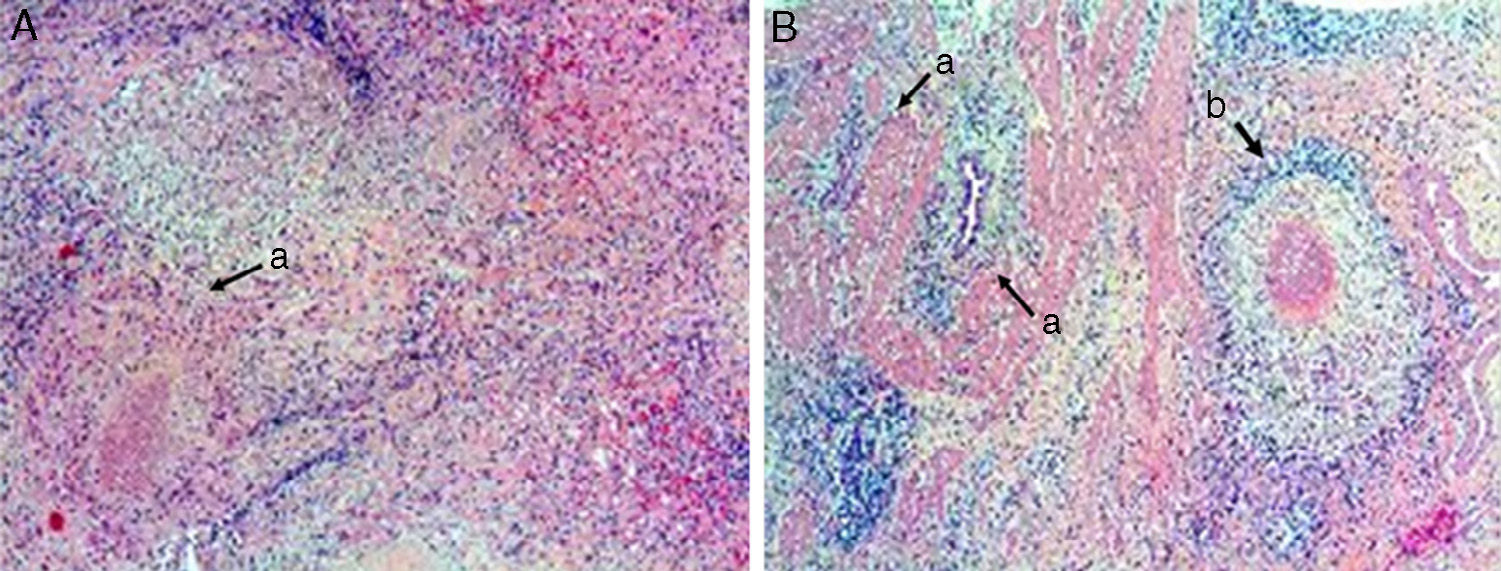
Surgical assessment was performed by right subcostal laparotomy in order to obtain a confirmation biopsy after having no radiological “window” for percutaneous puncture. The gallbladder was observed to be thickened and closely adhered to the main bile duct and duodenum, with a lithiasis of approximately 2cm. Biopsies were taken of the hepatic lesions, whose intraoperative histology identified a tuberculoid granulomatous reaction and absence of malignancy. Given these findings, simple cholecystectomy was completed. The intraoperative histology of the gallbladder confirmed the presence of tuberculosis with no signs of malignant disease. The definitive pathology study reported the existence of hepatic lesions with tuberculoid granulomatous reaction, caseous necrosis (Fig. 2A) and chronic cholecystitis with cholelithiasis and tuberculoid granulomas with caseous necrosis in the gallbladder wall (Fig. 2B). In the postoperative period, tuberculin and QuantiFERON®-TB-Gold tests were negative, and positive results were obtained by polymerase chain reaction. Patient progress was satisfactory and she was discharged on the 8th day post-op. She later completed tuberculosis treatment with isoniazid, rifampicin and pyrazinamide for 6 months, and a follow-up CT showed the resolution of the hepatic granulomas (Fig. 1D).
(A) Liver parenchyma with granulomas compromised of epithelioid cells and lymphocytes, with caseous necrosis and abscess (a) (haematoxylin–eosin 5×); (B) gallbladder wall with fibroconnective tissue showing invaginations of the surface epithelium, creating Rokitansky-Aschoff sinuses (a); granuloma comprised of epithelioid cells, with giant Langhans-type multinucleated cells, lymphocytes and centers with caseous necrosis (b) (haematoxylin–eosin ×5).
Since the first description of tuberculosis of the gallbladder, less than 120 cases have been reported in the literature.6 In comparison with other cases of abdominal tuberculosis, gallblader TB most frequently presents in older patients. Cholelithiasis, obstruction of the cystic duct and benign lesions like gallstones, diffuse papillomatosis and opisthorchiasis are factors that promote the development of gallbladder TB.7,8 The most common clinical presentation described is chronic cholecystitis or gallbladder mass accompanied by nonspecific symptoms like abdominal pain, weight loss, fever, anorexia and/or vomiting.2,9,10 Complementary studies are usually nonspecific and detect anaemia and increased erythrocyte sedimentation rate, which, together with the low rate of clinical suspicion, mean that the diagnosis is frequently histological, postoperative or postmortem.6 Computed tomography has more recently defined findings that could lead to the diagnosis of gallbladder TB, such as hypodense irregular thickening of the gallbladder wall with perivascular edematous changes, lesions to the micronodular basal cell or polypoid lesions to the gallbladder wall, masses with focal areas of necrosis or calcifications, and especially lesions associated with infiltration of the hepatic parenchyma with multiple patchy calcifications or lymph nodes with peripheral enhancement.6
The nonspecific symptoms and complementary test results of micronodular tuberculosis of the gallbladder frequently simulate gallbladder cancer.2,6 Findings like the presence of liver metastases or hepatic infiltration have usually guided the diagnosis towards gallbladder carcinoma.9 In this case, however, the hepatic lesions described were tuberculous granulomas that, together with the nonspecificity of the other radiological findings, provided the preoperative diagnosis of gallbladder carcinoma with hepatic metastases. Therefore, it is a diagnosis that should be included in the differential diagnosis of gallbladder carcinoma even in the presence of hepatic lesions that suggest liver metastases in the complementary studies. Given the higher incidence of both diseases in older patients, it is necessary to be informed of this uncommon disease, which is curable with medical treatment but is currently diagnosed during surgical procedures.
Conflict of InterestThere are no relationships, conditions or circumstances that could contribute to a potential conflict of interests.
Please cite this article as: Mon Martín F, Guil Ortíz B, Delgado Plasencia LJ, Expósito Afonso I, Bravo Gutiérrez AF. Tuberculosis de la vesícula biliar; un dilema diagnóstico con el carcinoma de vesícula metastásico. Cir Esp. 2015;93:e143–e145.