Several groups studying the results of the classic sphincteroplasty show improvement of 75% of patients treated in a short-term follow-up, with a worsening of this data in the long-term follow-up down to an improvement of 50% of the patients. Some other groups published more optimistic results, showing an 80% success rate without any deterioration of the technique over time after introducing a separate repair of the internal and external muscles. We think that the introduction of some modifications in the classic technique, named “Anatomic sphincteroplasty with combined reconstruction of external and internal anal sphincter muscles” may obtain very good clinical and anorectal manometric results both in a short and mid-term follow-up. In addition, increasing the pressive length in the anal canal may contribute to maintain more stable results over time.
Los estudios que evalúan la efectividad de la esfinteroplastia clásica muestran una mejoría alrededor del 75% a corto plazo, constatándose un deterioro en el tiempo con resultados satisfactorios a largo plazo alrededor del 50%. Tras introducir la realización de la reparación por separado del esfínter anal interno y externo se publicaron tasas de éxito del 80%, observando que estos resultados se mantenían a largo plazo. Pensamos que la introducción de modificaciones en la técnica quirúrgica desde una mentalidad anatómica y reconstructiva, que hemos denominado: “Esfinteroplastia anatómica mediante reconstrucción combinada de esfínter anal interno y externo”, puede obtener muy buenos resultados clínicos y manométricos en el seguimiento a corto y medio plazo. Asimismo, el aumento de longitud de la barrera presiva generada por la técnica puede colaborar a que estos resultados se mantengan más estables a lo largo del tiempo que con la técnica clásica.
Sphincter repair is one of the most commonly used techniques to treat anal incontinence when there is severe sphincter injury caused by an obstetric history, proctologic surgery or accidental trauma.1–6
The overlapping sphincteroplasty described by Parks and McPartlin7 and modified by Fang et al.8 in 1984 is still the most commonly used surgical procedure by most surgeons.9 The technique, as described, recommended not to separate the internal anal sphincter (IAS) from the external anal sphincter (EAS) and not to excise scar tissue from the severed muscle ends.8 Most authors agree that they are good or very good in the short to medium term, restoring continence for solid and liquid stools in 60%–80% of patients.9–11 However, their efficacy has been found to deteriorate over time, decreasing by up to 50% in the long term.3,11
In 1991, Wexner et al.12 introduced a modification: separate repair of IAS and EAS. Early publications showed slightly better results in the short and medium term (75% recovered faecal continence), and Maslekar et al.13 reported that these results were stable over time. In contrast, Briel et al.14 found no benefit with this technical modification.
Our experience in anatomical studies using cadaveric simulation models for training in surgical techniques in coloproctology allowed us to observe that the possibility of separate dissection and repair of the IAS and EAS restores the injured anatomy better and more selectively. It was also decided to incorporate some details in the dissection of the affected area and in the practice of specific measures with reconstructive intent.
Surgical techniqueWe have called this variation of the classic sphincteroplasty "anatomical sphincteroplasty by combined reconstruction of the internal and external anal sphincter".
The main modifications introduced in the technique are as follows:
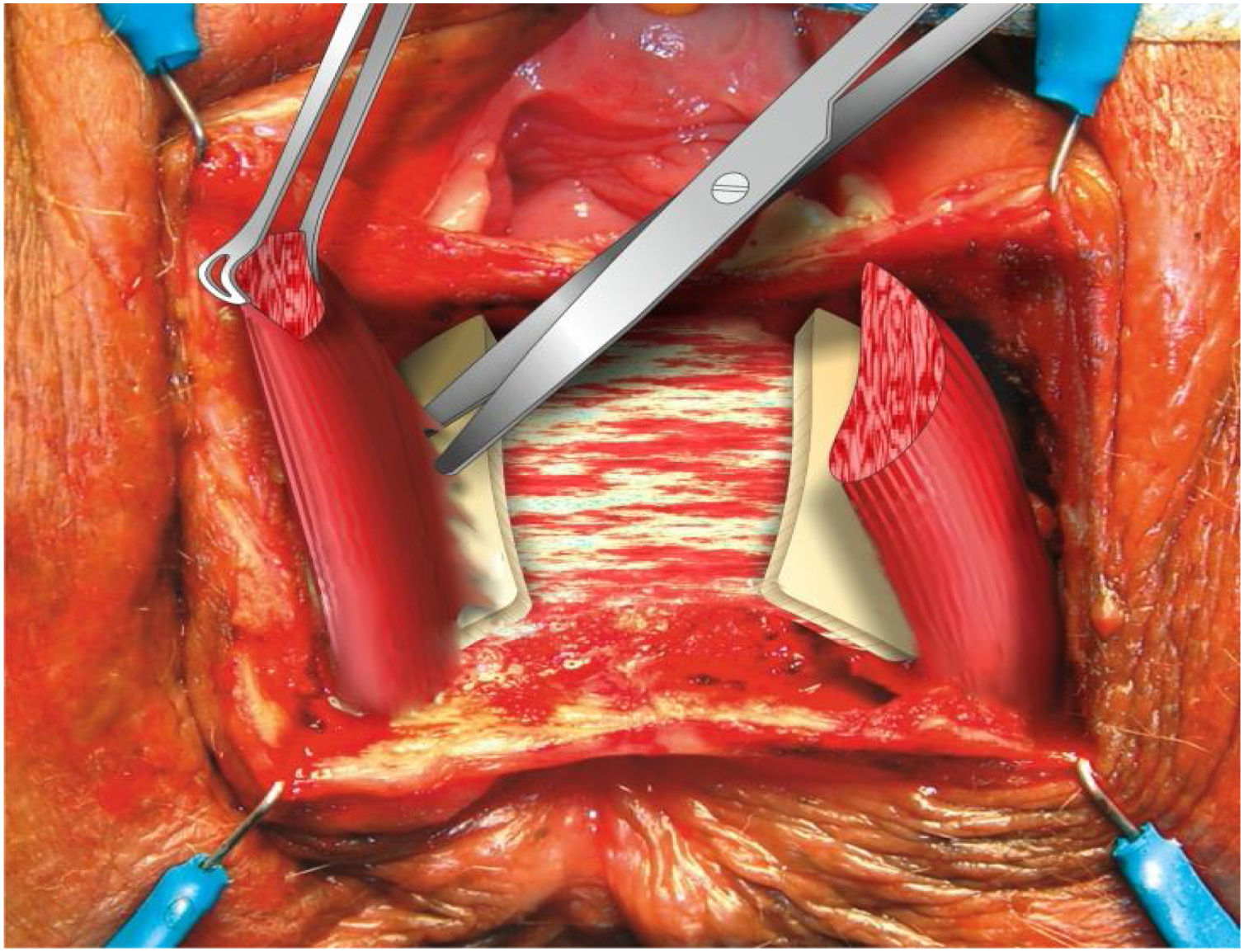
- 1
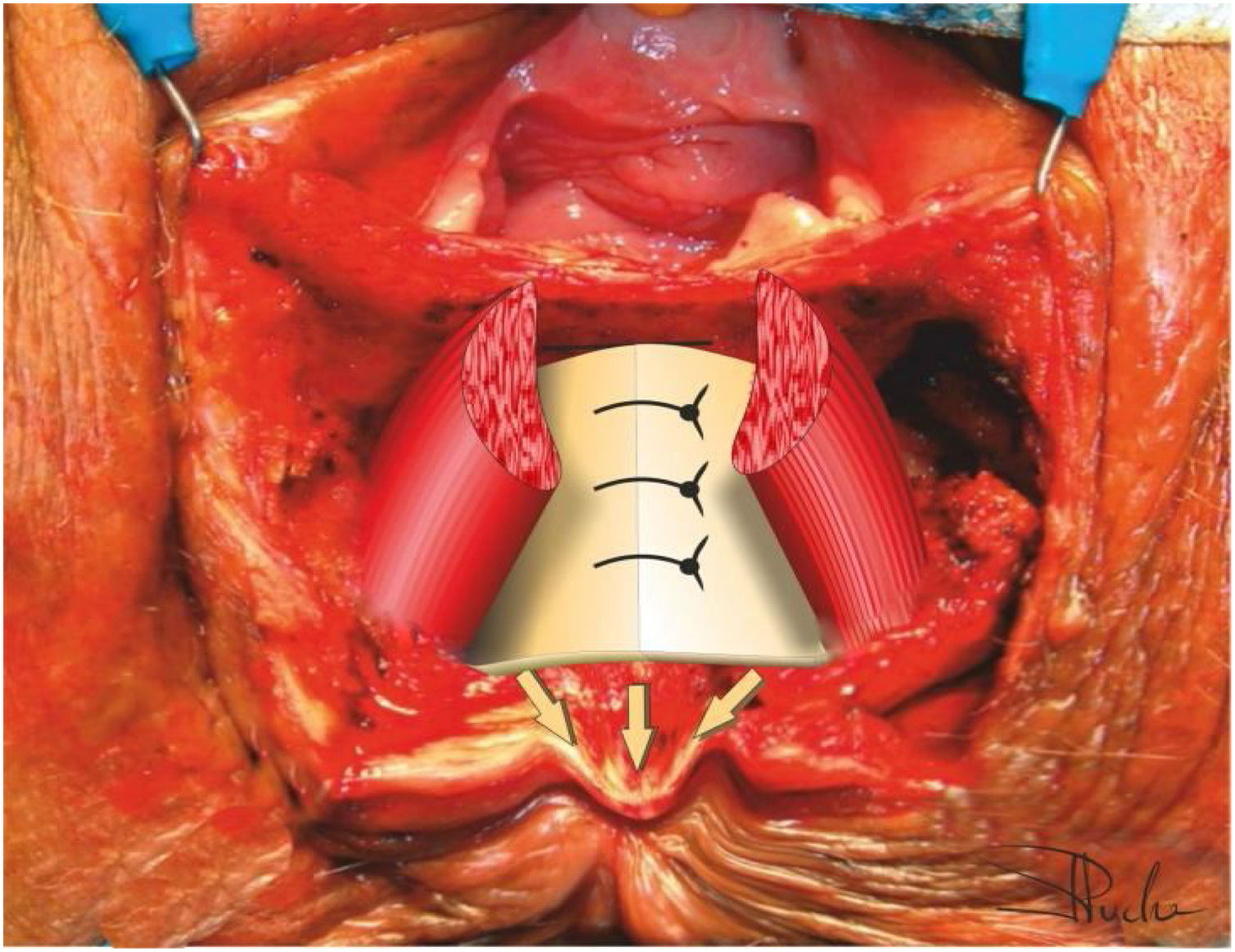
Perform a deep dissection of the anovaginal space until both loops of the puborectalis muscle are clearly visualised. Dissection of the intersphincteric space separating the IAS from the EAS. This will allow us to perform a plication or sphincterorrhaphy of the IAS (when its complete lesion is evident) longitudinally in the midline of at least 4 cm in length. In this way, we increase the maximum basal or resting pressure not only circumferentially, but we also extend this increase in depth, restoring both anatomically and functionally the maximum possible pressure length of the anal canal.
- 2
Plication of the most distal portion of the IAS also includes an anal plasty with the subcutaneous cellular tissue at the level of the anal margin itself, which makes it possible to restore the anal skin folds by inverting and externally protruding the anal margin. This not only increases the length of the plasty, but also generates a greater barrier effect at the height of the anal margin, achieving a better complete closure or sealing of the anal orifice at rest.
- 3
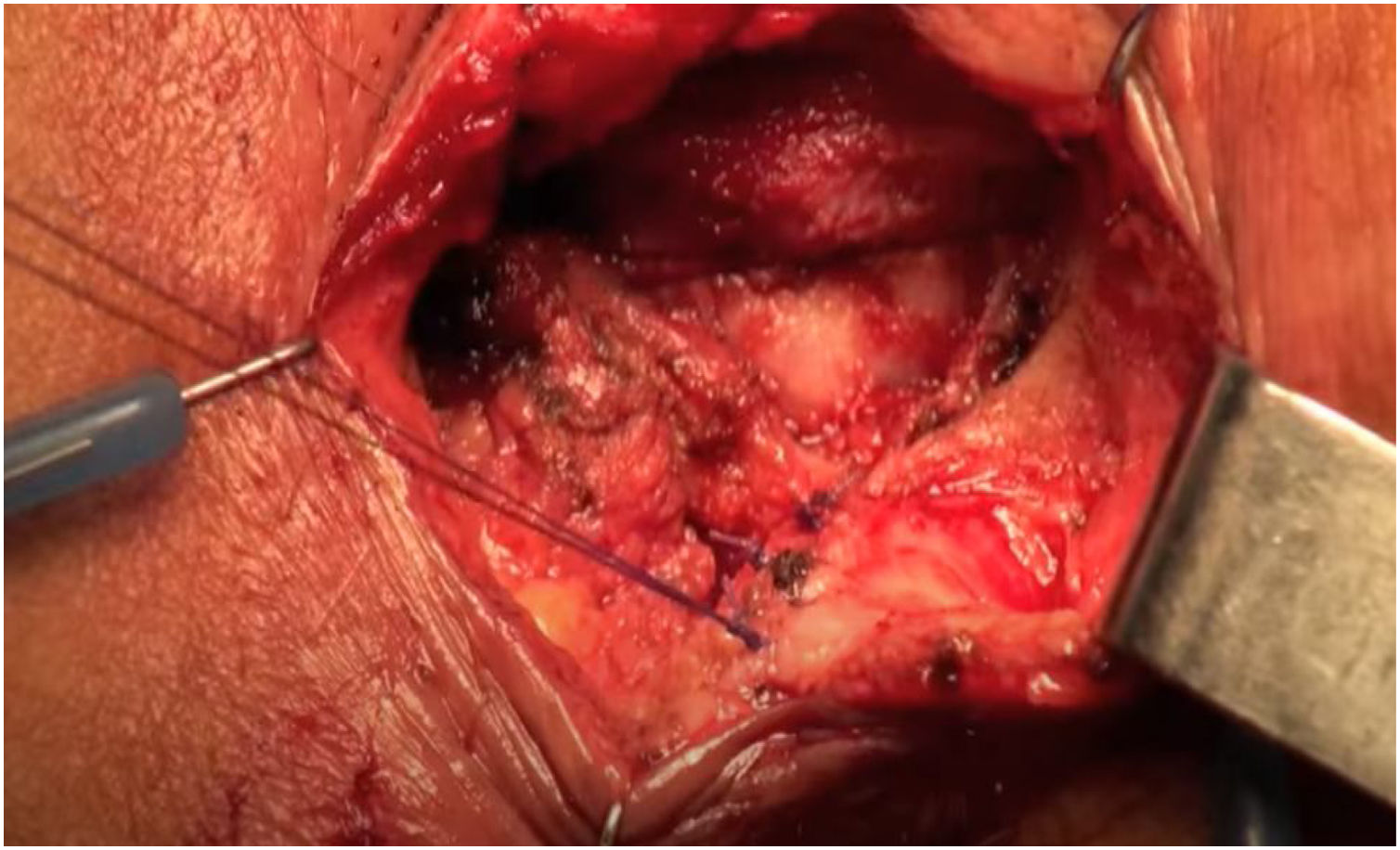
After initial identification and dissection of the EAS muscle endings, the scar and non-contractile fibrotic tissue can be removed from the muscle endings. These do not need to be released much laterally, thus avoiding nerve injury to pudendal end branches, as the plication of the IAS in the midline allows the overlapping sphincteroplasty of the EAS strands to be performed easily and without any tension.
The video of the fundamental steps of the surgical technique can be viewed at the link shown in Fig. 1.
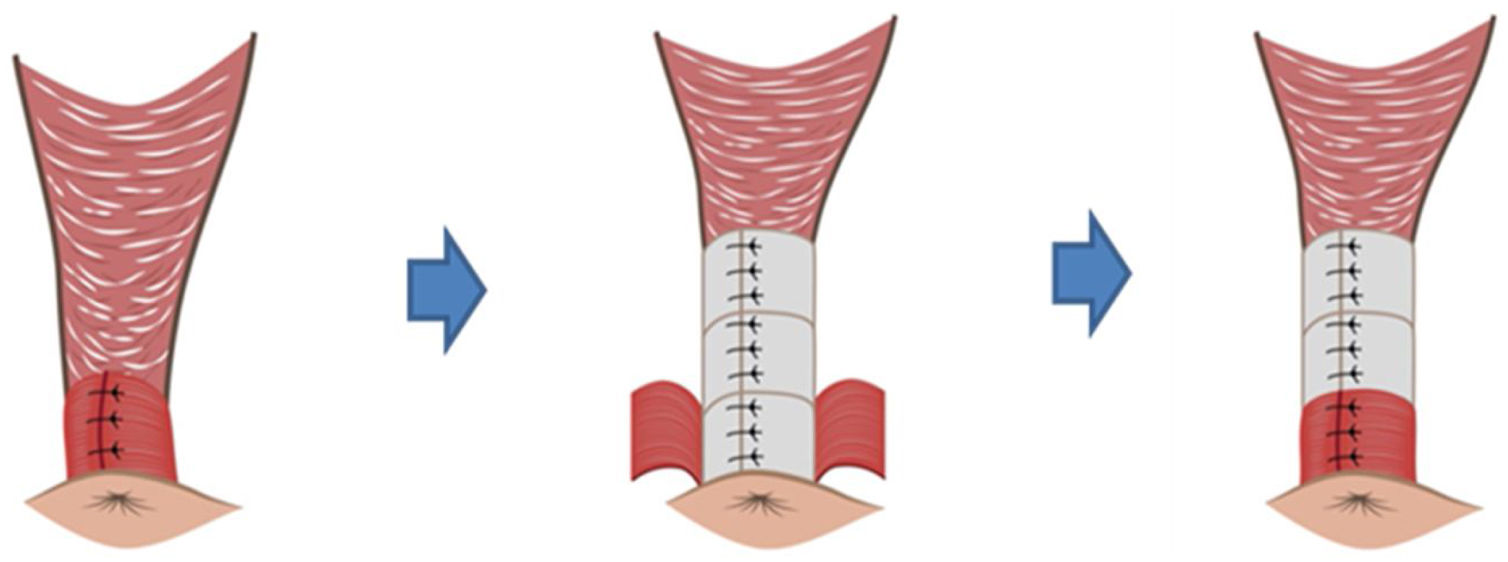
The technique schematised by steps:
- 1
Curvilinear incision in the area of the defect, 2−3 cm away from the anal margin.
- 2
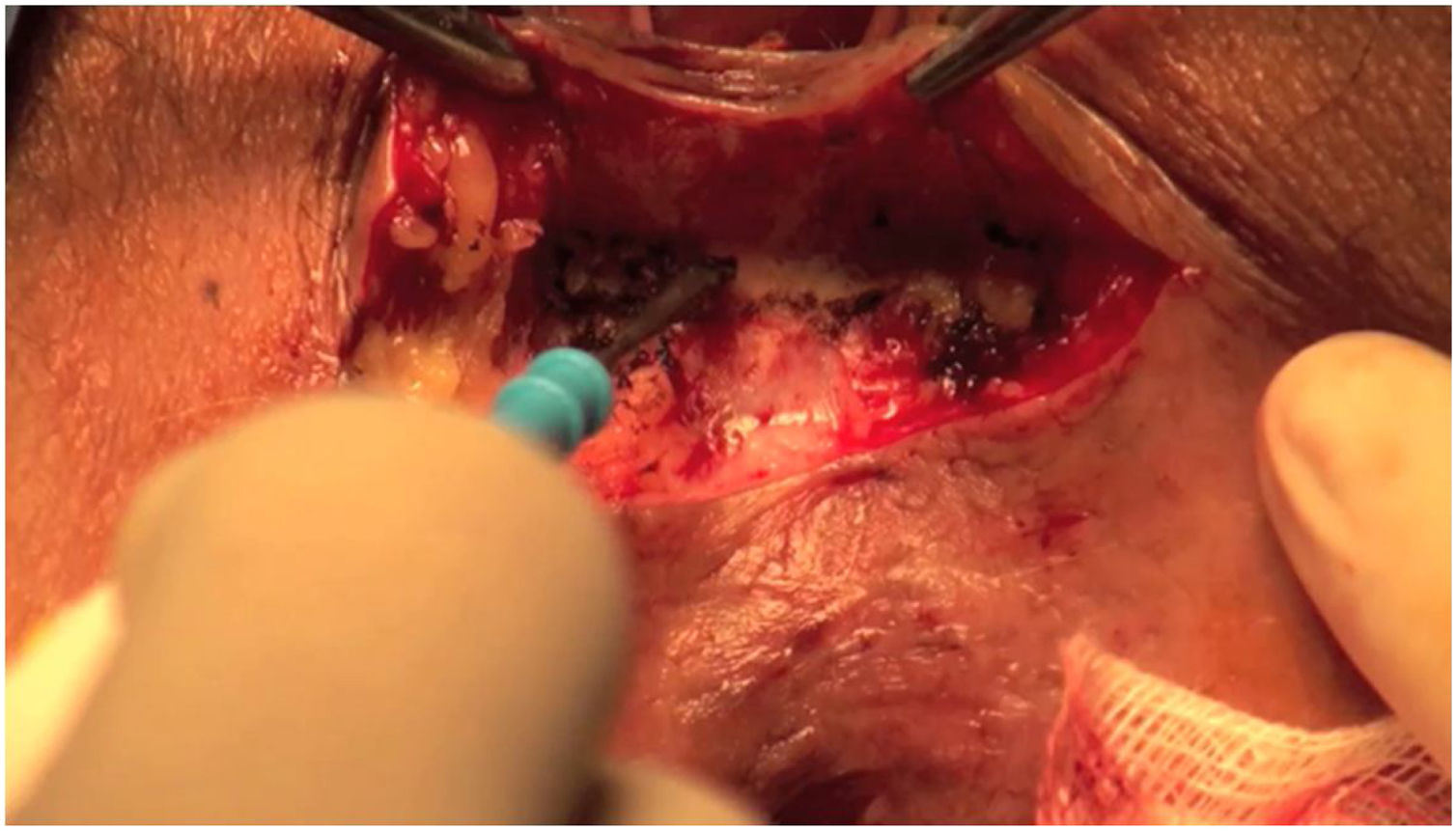
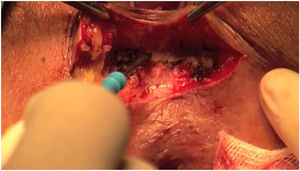
Wide dissection of the anovaginal space (Fig. 2).
- 3
Lateral dissection until the ends of the sphincter complex are located.
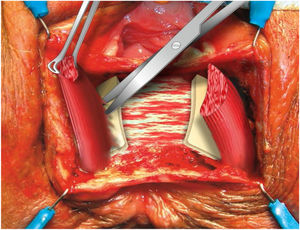
- 4
Identification of the IAS. Excision of the scar tissue of the IAS. Dissection of the intersphincteric space (Fig. 3).
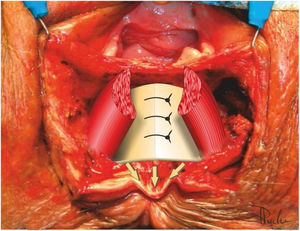
- 5
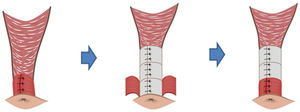
Selective plication or sphincterorrhaphy of the IAS with 3/0 resorbable braided suture, creating a 4 cm long loop (Fig. 4).
- 6
Performance of an anal plasty by inversion and protrusion of the anal margin itself (Fig. 5).
- 7
Overlapping of the EAS with 3/0 long-term resorbable monofilament suture.
- 8
Approximation of the subcutaneous cellular tissue.
- 9
Simple partial skin closure or butterfly flap closure in cases of severe anovaginal cloaca.
All patients in whom this technique was used had an EAS and IAS defect not exceeding 180, irrespective of their aetiology. Furthermore, all cases had a Cleveland Clinic scale15 score of more than 9 points, following the implementation of hygienic-dietary measures, medication and biofeedback.
To date, we have performed the technique in 30 patients, evaluating the short- and medium-term results, with a median follow-up of 11.5 and 37.5 months, respectively. Five patients had postoperative complications, all of which were resolved conservatively, except for one patient who required a new sphincteroplasty. Among the results observed, there was an improvement in the Cleveland Clinic Score, which went from a median of 15.5 to 3 points in the early evaluation and to 2 points in the evaluation performed more than 3 years after surgery (p < .001 between preoperative and postoperative values). There was a statistically significant improvement in all items of the faecal incontinence quality of life survey and more than 93% of patients were satisfied or very satisfied after surgery. There was also evidence of a significant increase in PMB and PMCV from a median of 25 and 55 mmHg to 40 and 100 mmHg (p < .001), respectively, at short-term follow-up. The same variables were evaluated comparing both postoperative follow-up periods, with no deterioration of the results. These data are awaiting publication in a more developed form.
DiscussionPerforming a wider and deeper dissection of the anovaginal space allows for a longer repair using IAS plasty. This reconstruction reaches deeper than the area of the EAS overlap.
Graphically, it would be like buttoning a shirt all the way up, not just the lower or middle portion, but all the way to the top. This seems to us to be a key factor in the improvement of clinical results, as we extend the pressive area longitudinally and in depth with respect to the classic technique of overlapping en bloc sphincteroplasty, in which we would only recover the pressive anal canal in the area of the overlap (Fig. 6).
Furthermore, plication or sphincterorrhaphy of the IAS will allow us to more easily perform an EAS overlap without tension, which can also be associated with fewer failures of the technique. Therefore, we differ from the opinion of Briel et al.14 who state that more complex dissection of the IAS and EAS and wide dissection of the anovaginal space has no clinical repercussions; in fact, in our study we observed a greater increase in acceptable outcomes and postoperative PMB than described in the literature.
Another modification included in our technique is to continue the IAS plasty very distally, until it reaches the subcutaneous cellular tissue of the anal margin itself. This plasty generates a bulge in the anal margin, like a "haemorrhoid", which may be reminiscent of the physiological role played by the haemorrhoidal plexuses in continence.16 We have also observed that performing this suture so distally allows us to reconstruct the lost folds of the anal margin. Our impression is that adding this technical detail to the separate repair of the IAS and EAS of the technique proposed by Wexner et al.12 may be key to increasing the barrier effect, sealing the new anal orifice more competently, which would translate into a greater possibility of recovery of continence to gas and a decrease in soiling, which in previous series of our group,17,18 when we did not include this manoeuvre, did not usually happen.
There is no study in the literature that evaluates whether preservation of the scar tissue of the sphincteric cords, in cases in which the IAS is repaired independently, is necessary or beneficial. This scar tissue could hypothetically allow lengthening of the sphincteric cords to avoid tension suturing, while suturing at this level would have less risk of tearing the tissues than suturing at the muscular level. However, by incorporating the IAS plasty independently beforehand, it brings the EAS strands clearly closer together so that they can overlap without difficulty or tension. Thus, sphincteroplasty should not only aim to restore the anatomical aspect, but also its functionality, which is why we believe that a sutured muscle tissue without tension, well vascularised, healthy, will supposedly offer better results.
In recent years, multiple studies have been published pointing to a deterioration of clinical outcomes over time, with several authors reporting that the worsening begins to appear between 41 and 60 months.11,19 In our study, although longer-term follow-up is at a median of 37.5 months, no deterioration was observed (Table 1).
Evaluation of the Cleveland Clinic Score with time in different series.
| Authors | N | CCS Pre | CCS Postop1 (months) | CCS Postop2 (months) | P* | |
|---|---|---|---|---|---|---|
| Classical sphincteroplasty | ||||||
| Evans et al.20 (2006) | 33 | 9.71 | 6.36 (< 42) | 4.73 (> 42) | >.05 | |
| Lehto et al.21 (2013) | 56 | 11.8 | 9.5 (22.8) | 12 (89.3) | .003 | |
| Johnson et al.22 (2010) | 33 | 12 | 7 (12) | 9 (103) | ≤.05 | |
| Pla-Mart et al.17 (2020) | 35 | 15.7 | 6.1 (30) | 8.4 (110) | >.05 | |
| Combined sphincteroplasty | ||||||
| Maslekar et al.13 (2007) | 64 | 12 | 5 (12) | 7 (84) | .09 | |
| Serie actual | 20 | 15.5 | 2.5 (12) | 3 (55) | .78 |
CCS, Cleveland Clinic Score; Postop1, early postoperative; Postop2, late postoperative; Pre, preoperative.
In conclusion, we believe that "anatomical sphincteroplasty with combined reconstruction of the IAS and EAS" is a safe, reproducible technique with a low percentage of complications and very good short- and medium-term results, with no deterioration observed during the time evaluated.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: García-Armengol J, Martínez-Pérez C, Roig-Vila JV. Esfinteroplastia anatómica mediante reconstrucción combinada del esfínter anal interno y externo en el tratamiento quirúrgico de la incontinencia anal. Cir Esp. 2022;100:580–584.