Cardiovascular disease secondary to atherosclerosis is the main cause of morbidity and mortality in the world. Cardiovascular risk stratification has proven to be an insufficient approach to detect those subjects who are going to suffer a cardiovascular event, which is why for years other markers have been sought to help stratify each individual with greater precision. Two-dimensional vascular ultrasound is a excellent method for vascular risk assessment.
La enfermedad cardiovascular secundaria a aterosclerosis es la principal causa de morbilidad y mortalidad en el mundo. La estratificación del riesgo cardiovascular ha demostrado ser una aproximación insuficiente para detectar aquellos sujetos que van a padecer un evento cardiovascular por lo que desde hace años se buscan otros marcadores que ayuden a estratificar cada individuo con mayor precisión, la ecografía vascular en dos dimensiones es un excelente método para la evaluación de riesgo vascular.
Cardiovascular disease (CVD) secondary to atherosclerosis remains the leading cause of morbidity and mortality worldwide. This process develops progressively and silently from the earliest years of life and is distributed throughout the arterial tree and accelerated by certain cardiovascular risk factors (CVRFs).1,2 Cardiovascular risk stratification (CVR) of an individual based on the effect of these CVRFs (sex, age, blood pressure, dyslipidaemia, presence of diabetes, or history of smoking) has proven an insufficient approach to detect with sufficient sensitivity and specificity individuals who will suffer a cardiovascular event (CVD) in the form of ischaemic heart disease, cerebrovascular disease, or peripheral artery disease. According to these guidelines, one in five men, and almost half of the women who suffer CVD, would not be indicated for initiating lipid-lowering treatment in primary prevention, and therefore for years now other markers have been sought to help stratify the CVR of each individual with greater precision.3
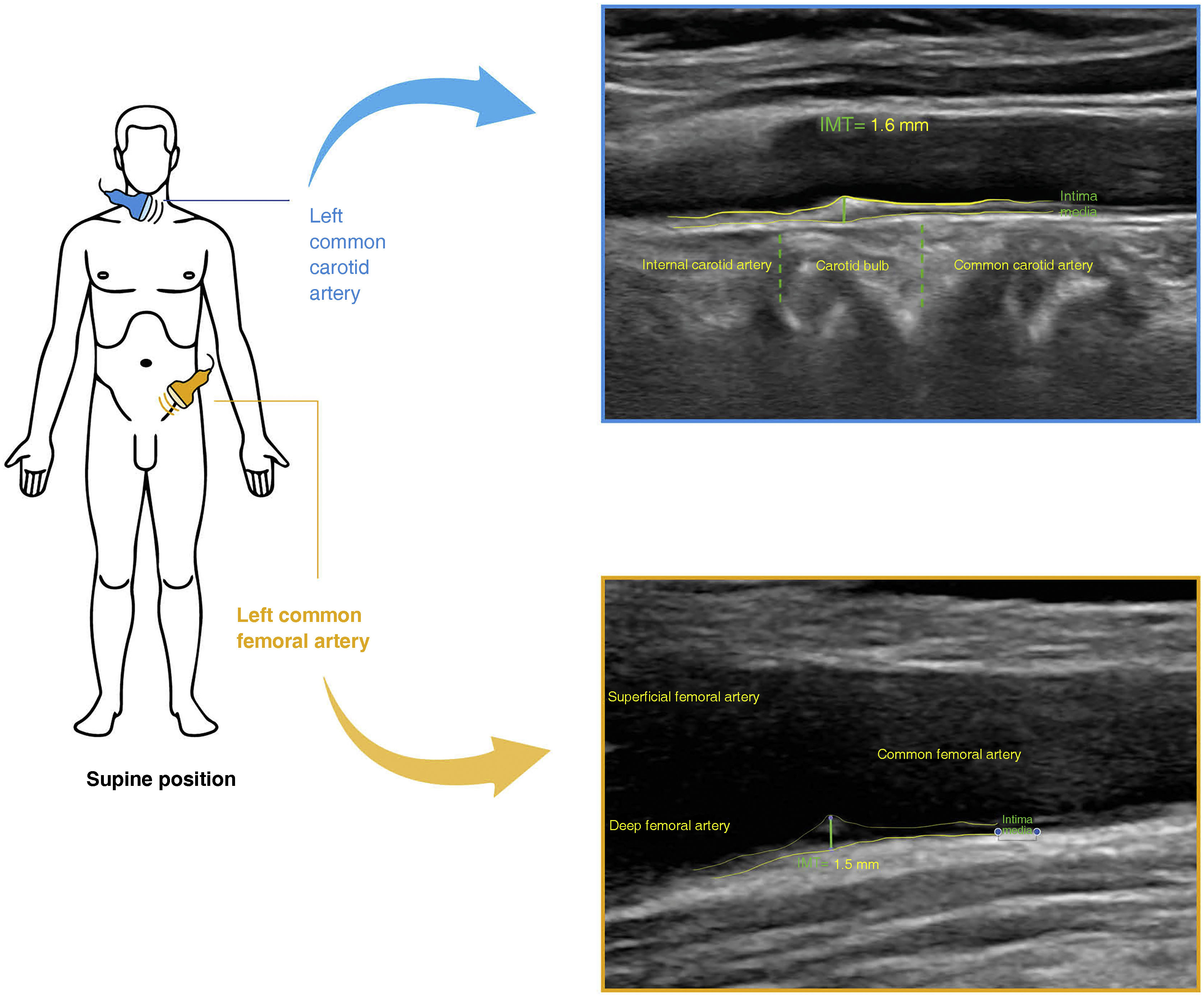
Vascular ultrasound as a method of detecting subclinical atherosclerosisTechnological developments associated with biomedical sciences have made it possible to observe the natural evolution of atherosclerotic lesions non-invasively.1,2 Two dimensional vascular ultrasound (2D-VUS) allows the observation and grading of lesions from early stages, using intima-media thickness (IMT), defined as the distance between the intima layer, at the interface between the arterial lumen and the beginning of the arterial wall, and the end of the media layer, at the boundary between the media and adventitia layers (Fig. 1). The increase in carotid artery IMT has been directly related to the incidence of CVD in population studies,1,2 and a definition of advanced lesion or atheromatous plaque in the carotid artery was established by consensus as early as 2006, a lesion with an IMT ≥ 1.5 mm or thickening > 50% with respect to adjacent segments.1,4 The presence of atheromatous plaque in the carotid artery has been shown to be robustly and independently associated with the incidence of CVD in the general middle-aged population,5,6 with earlier onset in populations with higher CVR, such as subjects with primary dyslipidaemia,7 diabetes,8 or with a single long-standing CVRF such as smoking.9 Recently, both the European Society of Cardiology and the European Society of Atherosclerosis have recognised the presence of plaque in the carotid artery wall detected by means of 2D-VUS as an advanced atherosclerotic lesion that would mean reclassifying a given individual’s CVR.10
Until recently, femoral artery assessment by 2D-VUS has been equally accessible, included in the assessment of subclinical atherosclerosis. The presence of plaque in this location has been shown to be more frequent and earlier than in the carotid artery, especially in male smokers,5,7–9 and to be more associated with CVRF and coronary calcium than plaques in the carotid artery.8,9 Prospective studies have demonstrated the added value in the prediction of CVD of detecting atherosclerosis in both the carotid and the femoral territories.5,9
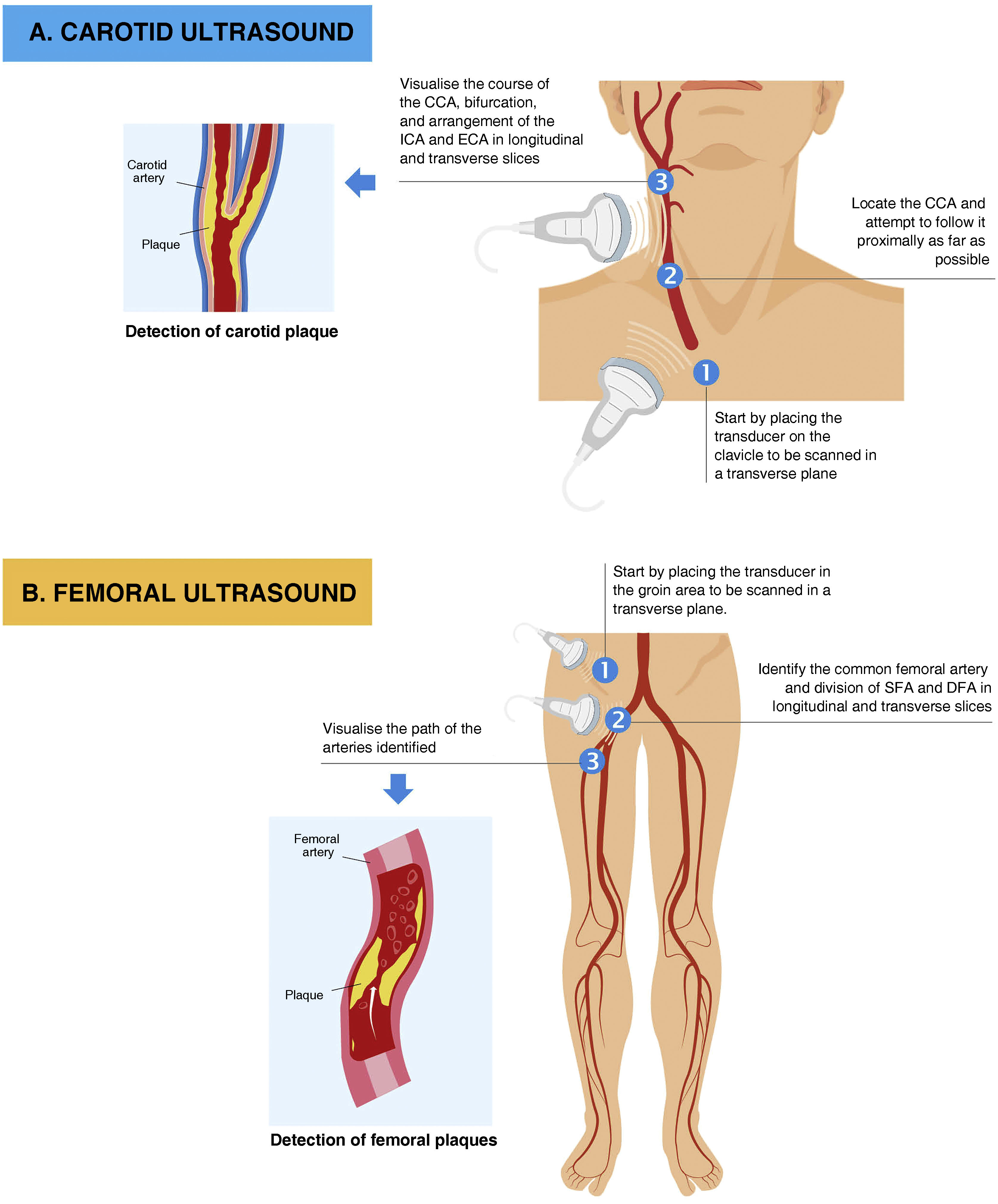
How is it done?Protocol for scanning: equipment, patient position, and systematics of the techniqueCarotid and femoral artery ultrasound scans are preferably performed with a scanner equipped with a high-frequency linear probe (≥7 MHz) that allows images of acceptable quality with a depth of field of between 3 and 4 cm, applying an average gain of 60 dB1,1 although even portable devices have demonstrated their ability to detect plaques in the arterial wall.
Carotid artery ultrasound: Carotid artery ultrasound: to obtain the image, the patient must be placed in the supine position, with the neck extended and tilted 45° away from the side being scanned. The professional performing the test is positioned at the patient's bedside, either facing the patient or behind them. The scan begins with a transverse sweep in B-mode, from the base of the neck just above the clavicle in an upward direction until reaching the mandible, locating the carotid artery in the centre of the screen (Fig. 2). The transducer should be kept perpendicular to the plane of the skin at all times, with the probe marker facing left. This scan allows an initial assessment of the presence of plaques, some of which are not detected in the longitudinal projection because they are located in an area of the wall that is not perpendicular to the projection used. Then, after rotating the transducer 90° clockwise, the same arterial segment is visualised in the longitudinal projection. In this projection, we can obtain an image of both walls of the artery, although in general, sharper images are obtained of the posterior wall of the entire course of the common carotid artery (CCA) and the beginning of its main branches, which means we can quantify the IMT quickly (Fig. 1).
The first arterial segment to be visualised in the cross-sectional scan corresponds to the end of the CCA, which is distinguished by its regular calibre and its location just before it increases the calibre of the artery, known as the carotid bulb (CB). This segment is delimited between the end of the CCA and the branching into the external carotid artery and the internal carotid artery. The CB is visible in most patients and is where atheromatous plaques are most frequently detected (Fig. 1), therefore, except in cases of anatomical difficulty, it should never be left unexplored.1,4,5 We can use its location to locate the branches of the carotid artery, the internal carotid artery more frequently being in a superior and medial plane in the transverse projection, while the external carotid artery is located in the inferior and lateral plane.
Ultrasound of the femoral artery: the femoral artery is located medial to the vein, immediately below the inguinal ligament and above the muscular plane of the iliopsoas muscle. The vein has a larger diameter and collapses with moderate compression, while the artery shows its pulsatile characteristic during compression.
To perform the examination, the patient must be placed in the supine position, uncovering the inguinal area with the examiner positioned laterally to the patient. The examination is performed in two steps: the first, once the artery has been located by palpation, with the transducer perpendicular to the plane of the skin and with the probe marker facing to the right, is to perform a transversal sweep from the inguinal area in a caudal direction, identifying the distal segment of the common femoral artery (CFA) and its bifurcation into the superficial and deep femoral artery (Fig. 2). Once the transverse scan has been performed, we rotate the probe 90°, with the tip of the transducer in a caudal direction, so that we can see the longitudinal projection of the distal segment of the CFA followed by its bifurcation, which gives rise to the superficial and deep femoral artery. The aim is to obtain an image of the artery as horizontal as possible from the posterior wall of the most distal segment of the CFA and the beginning of the bifurcation because atheroma plaques can also be detected in this location more frequently than the other segments explored of the femoral artery.
Ultrasound is not the best procedure for characterising a complex lesion in either the carotid or femoral arteries, and other imaging tests should be considered, which are beyond the scope of this article.
For whom is it recommended?2D-VUS to detect atheromatous plaques in the carotid and femoral artery only makes sense in those subjects undergoing primary prevention of CVD. Screening for these lesions will be indicated for those in whom their detection is likely and in whom the presence of plaques will result in intensifying preventive, pharmacological, and lifestyle treatment. The effect of these treatments on these lesions is currently debated in the scientific community and is beyond the scope of this protocol. Moreover, the deterrent value of their visualisation for patient compliance with pharmacological treatment should not be underestimated.1–3
The observational data obtained in studies and the need to improve CVR stratification make 2D-VUS of the carotid and femoral artery advisable in the following groups:
- 1
Persons over 45 years of age with intermediate risk.1,6,9
- 2
Individuals with an extreme risk factor (e.g. primary hypercholesterolaemia) that may substantially modify their CVR.8
- 3
People with diabetes, especially at baseline or without other markers of CVR.8
- 4
Subjects classified as high CVR (not very high CVR) without clinical CVD.6,10
- 5
Individuals with doubts about starting treatment in primary prevention.5,6
Detection of plaques in medium-sized arteries has been shown to be a safe imaging method that improves CVR stratification. Due to its power, high predictive value, low cost, and safety, this scan could be implemented in the initial assessment of CVR in all patients in our routine clinical practice.
FundingNo funding was received for conducting this study.
Conflict of interestsThe authors have no conflict of interests to declare.