To assess the atherosclerotic burden in hypertensive patients with prediabetes without cardiovascular disease.
Patients and methodsWe included patients with hypertension and prediabetes (fasting blood glucose: 100–125mg/dl and/or glycohemoglobin A1c: 5.7–6.4%), excluding those with established cardiovascular disease or those at very high risk. We recorded major vascular risk factors. Subclinical arteriosclerosis was measured by the ankle/brachial index (ABI) and carotid intima-medial thickness (IMT). Subclinical arteriosclerosis was mild if IMT was >75p adjusted by age and sex and/or ABI was 0.7–0.9 and was considered moderate-severe when there was plaque and/or ABI<0.7.
ResultsWe included 53 patients, 63±7 years-old; women: 50.9% (95% CI: 36.8–64.9). Atherosclerotic burden was detected in 66.0% (95% CI: 51.7–78.5) of subjects. 24.5% (95% CI: 13.8–38.3) of patients had mild arteriosclerosis disease and 41.5% (95% CI: 28.1–55.9) had moderate-severe. This allowed us to re-stratified as very high vascular risk the 41.5% (95% CI: 28.1–55.9) of patients. 45.4% (95% CI: 16–74.8) of subjects with moderate initial risk were considered high or very high risk. In multivariate analyses, only smoking was associated with atherosclerotic burden (P=.07).
ConclusionsTwo thirds of hypertensive patients with prediabetes had subclinical arteriosclerotic disease when they were evaluated by the ankle/brachial index and carotid ultrasonography. Approximately forty percent of patients were re-stratified as very high vascular risk. Nearly half of the prediabetic hypertensive patients initially classified as moderate risk were considered high or very high risk.
Conocer la carga aterosclerótica (carga ATC) de pacientes hipertensos prediabéticos sin enfermedad cardiovascular.
Pacientes y métodosSeleccionamos pacientes hipertensos en situación de prediabetes (glucemia en ayunas 100-125mg/dl y/o glicohemoglobina A1c 5,7-6,4%), excluyendo aquellos con enfermedad cardiovascular establecida o de muy alto riesgo. Registramos los principales factores de riesgo vascular. Se calculó el índice tobillo/brazo (ITB) y el grosor íntima-media (GIM) carotídeo. Se consideró enfermedad arteriosclerosa ligera cuando el GIM fue >percentil75 para edad y sexo y/o ITB de 0,70-0,90 y moderada-grave en presencia de placa ateromatosa y/o ITB<0,7.
ResultadosIncluimos 53 pacientes, de 63±7años; mujeres: 50,9% (IC95%: 36,8-64,9). Se detectó carga ATC en el 66,0% (IC95%: 51,7-78,5) de los sujetos. El 24,5% (IC95%: 13,8-38,3) de los pacientes presentaron enfermedad arteriosclerosa ligera y un 41,5% (IC95%: 28,1-55,9) moderada-grave. Esto nos permitió reclasificar como de riesgo vascular muy alto a un 41,5% (IC95%: 28,1-55,9) de los pacientes. Un 45,4% (IC95%: 16-74,8) de los sujetos de riesgo inicial moderado pasaron a considerarse de alto o muy alto riesgo. En el análisis multivariante los fumadores o exfumadores presentaron 2,3 veces más riesgo (odds ratio=2,3; IC95%: 0,6-7,6) de presentar carga ATC, aunque sin alcanzar significación estadística.
ConclusionesDos tercios de los pacientes hipertensos con prediabetes tienen enfermedad arteriosclerótica silente cuando se evalúan mediante el ITB y la ecografía carotídea. Aproximadamente un 40% de los sujetos fueron reclasificados como de muy alto riesgo. Cerca de la mitad de los hipertensos prediabéticos clasificados inicialmente como de riesgo moderado pasaron a considerarse de riesgo alto o muy alto. El tabaquismo parece ser el factor de riesgo más relacionado con la presencia de carga ATC.
Estimation of individual vascular risk (VR) is essential before deciding on the appropriate therapeutic strategy. To this end, there are a number of assessment scales, such as the Framingham index or the SCORE project table, derived from studies in large patient cohorts. However, several studies have shown that the risk estimation they provide may not be accurate, as they have a low predictive value. In fact, a large number of individuals having a vascular event were not classified as high risk.1 This has led to an intensified search for new markers and bloodless techniques for early detection of subclinical atherosclerotic lesions.2
Atherosclerotic (ATS) burden is a concept which has gained great interest as a powerful predictor of cardiovascular events. It is also associated with a poor prognosis once such an event has occurred.3 ATS burden is the consequence of the actual effect vascular risk factors have on the individual, whether known about or not. Determining ATS burden enables us to tackle the actual risk the person has of having a cardiovascular event (stroke, myocardial infarction, etc.).
There are several well-documented methods for assessing and quantifying the ATS burden, such as the ankle-brachial index (ABI), carotid intima-media thickness (IMT) and the measurement of coronary calcium.
A low ABI (<0.90) is diagnostic of peripheral arterial disease, despite the fact that more than 80% of these patients do not have clinical manifestations, and it constitutes an equivalent of coronary risk,4 as it is associated with a greater likelihood of angina, myocardial infarction, congestive heart failure, need for coronary bypass, stroke and carotid and peripheral vascular surgery.5–7
The ABI adds predictive power of VR to risk scales based on traditional VR factors.8 People with a low ABI should be considered as high VR and candidates not only for intensive treatment of their risk factors but probably also for an active search for arteriosclerosis in other vascular territories.9
B-mode ultrasound has become the technique of choice for visualising IMT and atherosclerotic plaques in medium/large-lumen arteries (carotid, femoral or radial). There is evidence that IMT predicts stroke and myocardial infarction.10,11 In coronary heart disease, some studies have shown that atherosclerosis in the carotid artery and aorta are markers of the presence of coronary atherosclerosis.12
Although the IMT is a continuous variable without a clear upper cut-off point, a value >0.9mm is generally considered pathological, identifying the patient as high risk. Other consensus documents, such as that of the American Society of Echocardiography, consider an IMT greater than the 75th percentile adapted to the age, ethnicity and gender of the population.13
Atheroma plaques mean IMT values greater than 1.5mm or focal thickening >50% of the value of the surrounding IMT. In addition, it is also possible to characterise their content: a hypoechoic plaque is associated with the presence of lipids, while a hyperechoic plaque is predominantly fibrous. Numerous studies have shown that the predictive value of atherosclerotic plaques is higher than that of IMT in the estimation of VR.14
The aim of this study was to assess the ATS burden of hypertensive patients with prediabetes without known cardiovascular disease, using carotid ultrasound and ABI.
Material and methodsThis was cross-sectional descriptive study conducted in an urban health centre. We assessed 53 patients with hypertension and prediabetes criteria (baseline fasting blood glucose 100–125mg/dl and/or glycosylated haemoglobin A1c 5.7–6.4%) who attended the VR clinic for follow-up, excluding those with known cardiovascular disease or with very high VR.
Sociodemographic variables (age, gender), clinical variables (body mass index, smoking, previous lipid-lowering drug treatment, blood pressure (BP) control, ATS burden, carotid atherosclerosis, peripheral arterial disease) and laboratory tests (glycosylated haemoglobin A1c, total cholesterol [TC], low density lipoprotein cholesterol [LDL-C], high density lipoprotein cholesterol [HDL-C], triglycerides [TG]) were all analysed. We considered TG values ≥150mg/dl with low HDL-C (<40mg/dl in males and <50mg/dl in females) as atherogenic dyslipidaemia. We considered BP to be well controlled when below 140/90mmHg.
The patients’ VR was determined at the beginning of the study and after the investigations were performed. For that, we followed the recommendations of the European Society of Cardiology (ESC) 2016 Guidelines on cardiovascular disease prevention in clinical practice, using the SCORE risk table for populations from low-risk countries.15 In patients on drug therapy, their TC and systolic blood pressure (SBP) values before the start of the treatment were used.
The patients had their ABI assessed by vascular Doppler (Huntleigh portable Doppler with 8MHz probe) and carotid ultrasonography (SonoSite NanoMaxx ultrasound in B-mode with a 10–5MHz broadband linear transducer). Both carotids were examined for the presence of plaques along the length of the common carotid, carotid bulb and internal and external carotids. The mean IMT was obtained using automated software (Sonosite, SonoCalc IMT Software) at the level of the posterior wall (distal to the transducer) of both common carotids 1cm prior to the bifurcation, considering the measurements in six sections (3 different angles on the right and left sides).
Two degrees of atherosclerosis were defined according to the results of the ABI and IMT. The ATS burden was classified as follows:
- •
Mild atherosclerosis (ATS 1) when the IMT exceeded 75% of the percentile for age and gender (with no atheroma) and/or the ABI was in the range 0.70–0.90.
- •
Moderate-severe arteriosclerosis disease (ATS 2–3) when the atheroma was found and/or the ABI was less than 0.70.
Patients with ABI greater than 0.90 and an IMT lower than the 75th percentile without the presence of atheroma were considered free of atherosclerosis (ATS 0).
We carried out a descriptive, bivariate and multivariate statistical analysis using multiple logistic regression (with the enter method), taking the presence of ATS burden as a dependent variable (SPSS 20.0, IBM). The local IEC approved the study and all patients signed the informed consent form.
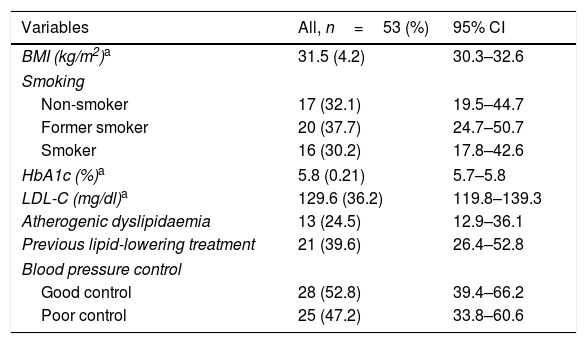
ResultsThe study included 53 patients with hypertension (27 females and 26 males), aged from 50 to 77, with a mean age of 63 (SD=6.9). The distribution of variables studied is shown in Table 1.
Characteristics of the study population.
| Variables | All, n=53 (%) | 95% CI |
|---|---|---|
| BMI (kg/m2)a | 31.5 (4.2) | 30.3–32.6 |
| Smoking | ||
| Non-smoker | 17 (32.1) | 19.5–44.7 |
| Former smoker | 20 (37.7) | 24.7–50.7 |
| Smoker | 16 (30.2) | 17.8–42.6 |
| HbA1c (%)a | 5.8 (0.21) | 5.7–5.8 |
| LDL-C (mg/dl)a | 129.6 (36.2) | 119.8–139.3 |
| Atherogenic dyslipidaemia | 13 (24.5) | 12.9–36.1 |
| Previous lipid-lowering treatment | 21 (39.6) | 26.4–52.8 |
| Blood pressure control | ||
| Good control | 28 (52.8) | 39.4–66.2 |
| Poor control | 25 (47.2) | 33.8–60.6 |
95% CI: 95% confidence interval; BMI: body mass index; HbA1c: glycosylated haemoglobin A1c.
ATS burden was detected in 66.0% (95% CI: 51.7–78.5) of the patients. Of the patients with ATS burden, 100% had carotid atherosclerosis (increased IMT or atheroma) and 14.3% (95% CI: 2.7–25.9) had peripheral arterial disease (ABI<0.90).
ATS burden was mild (ATS 1) in 24.5% (95% CI: 13–36) and moderate/severe (ATS 2–3) in 41.5% (95% CI: 28–55) of the patient studied.
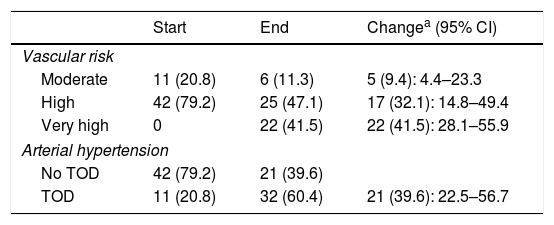
50% (95% CI: 34.2–65.8) of the patients initially considered as having no organ damage had their classification changed to target organ damage. The previous VR, and also therefore the LDL-C target, was reclassified in 41.5% (95% CI: 28.1–55.9) of the patients (Table 2). A total of 45.4% (95% CI: 16–74.8) of patients with moderate initial risk were reclassified as high or very high risk.
Change in vascular risk and target organ damage (TOD).
| Start | End | Changea (95% CI) | |
|---|---|---|---|
| Vascular risk | |||
| Moderate | 11 (20.8) | 6 (11.3) | 5 (9.4): 4.4–23.3 |
| High | 42 (79.2) | 25 (47.1) | 17 (32.1): 14.8–49.4 |
| Very high | 0 | 22 (41.5) | 22 (41.5): 28.1–55.9 |
| Arterial hypertension | |||
| No TOD | 42 (79.2) | 21 (39.6) | |
| TOD | 11 (20.8) | 32 (60.4) | 21 (39.6): 22.5–56.7 |
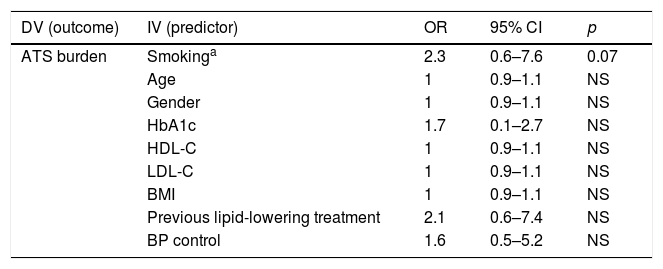
Smokers or former smokers had a 2.3 times higher risk (odds ratio=2.3; CI 95%: 0.6–7.6) of having ATS burden, although without reaching statistical significance. The remaining variables (age, gender, glycosylated haemoglobin A1c, TG, LDL-C, previous lipid-lowering drug therapy, BP control) were not significantly associated with the presence of ATS burden (Table 3).
Logistic regression analysis.
| DV (outcome) | IV (predictor) | OR | 95% CI | p |
|---|---|---|---|---|
| ATS burden | Smokinga | 2.3 | 0.6–7.6 | 0.07 |
| Age | 1 | 0.9–1.1 | NS | |
| Gender | 1 | 0.9–1.1 | NS | |
| HbA1c | 1.7 | 0.1–2.7 | NS | |
| HDL-C | 1 | 0.9–1.1 | NS | |
| LDL-C | 1 | 0.9–1.1 | NS | |
| BMI | 1 | 0.9–1.1 | NS | |
| Previous lipid-lowering treatment | 2.1 | 0.6–7.4 | NS | |
| BP control | 1.6 | 0.5–5.2 | NS |
ATS burden: present (mild, moderate/severe) or absent; OR: odds ratio.
Our idea for this study was based on the European Guidelines for the management of arterial hypertension (AHT)16 recommendation to look for subclinical organ damage, as there is evidence that it predicts cardiovascular death regardless of the score on the risk tables. This recommendation is of particular interest for patients with hypertension who are at moderate risk (classIIa recommendation, level of evidence B). Moreover, we selected hypertensive patients with prediabetes due to the evidence that VR increases even before the clinical diagnosis of diabetes.17
The concept of ATS burden is directly related to that of subclinical (or asymptomatic) organ damage, although there are different definitions; for example, in the case of IMT, ATS burden is considered when it exceeds 75% of the percentile for age and gender,13 while the European Society of Hypertension traditionally considers asymptomatic organ damage when IMT is greater than 0.9mm.
A high proportion of the patients we studied were receiving antihypertensive and/or lipid-lowering therapy. Therefore, when assessing the VR for these individuals, we used the TC and SBP figures from before they started treatment. We did this in an attempt to avoid underestimating their “actual” VR.
The most significant finding of the study was the high percentage of patients (66%) in whom ATS was detected, and particularly the percentage of hypertensive patients with prediabetes initially classified as having moderate risk who came to be considered high or very high risk (45.4%). This shows the importance of identifying ATS burden in hypertensive patients with prediabetes, as many of them are classified as moderate risk by the traditional risk scales. In the case of diabetic patients with hypertension, this assessment would have less practical use, as they are automatically included in the high-risk group and the finding of a high ATS burden would not substantially alter the therapeutic approach.
Of the measurements carried out, we consider the mean IMT to be the defining value, as previous studies have shown that the mean IMT value is better associated with the ATS burden in patients with hypertension than the maximum IMT.18
The IMT measurements were made in the segment of the common carotid most proximal to the bulb. Although there are various protocols regarding measurements, the most commonly used is the one for the common carotid artery for two main reasons: it is the most reproducible and it has demonstrated a similar ability to predict events as other more complex methods.
It was interesting to find that the majority had carotid atherosclerosis (increased IMT or atheroma) rather than decreased ABI, but this is explained by the capacity of vascular ultrasound to diagnose at an earlier stage in the atherosclerotic process.
With regard to the risk factors analysed, we found a marked, although not statistically significant, association between smoking and the presence of ATS burden which, in our opinion, is proof of the considerable endothelial damage smoking causes. The result is similar to that obtained by the ESPREDIA study.19
This study has a series of limitations. First of all, the small sample size limits statistical significance in the results. With this publication we are presenting the preliminary data of a bigger project that aims to include a larger number of subjects, and that should give it the statistical power necessary to obtain statistical significance for the strong association we found with certain variables such as smoking.
Secondly, the IMT was only measured in the common carotid artery, although the common carotid artery, carotid bulb and internal and external carotids were all assessed for atheroma. Another limitation is the cross-sectional nature of the study, which prevented us from establishing causal relationships.
We consider that the use of non-invasive techniques in primary care, such as the ABI and the carotid ultrasound, enable better assessment of the population's VR and an earlier and more appropriate tackling of the risk factors.
ConclusionsTwo thirds of hypertensive patients with prediabetes have ATS burden (mainly moderate/severe). Approximately 40% of the subjects were reclassified as very high risk after measuring the ABI and performing the carotid ultrasound. Nearly half of the hypertensive patients with prediabetes initially classified as being at moderate risk were reclassified as high or very high risk. Smoking seems to be the risk factor most related to the presence of ATS burden.
FundingThis work was funded with a FEA (Fundación Española de Arteriosclerosis [Spanish Arteriosclerosis Foundation])/SEA 2016 grant for Research in Primary Care.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ramírez Torres JM, López Téllez A, Valdivielso P, Barbancho Fernández MÁ. Evaluación de la carga aterosclerótica en hipertensos con prediabetes. Clín Investig Arterioscler. 2019;31:160–165.
This work received the award for the best communication in the area of Primary Care-Epidemiology at the 30th National Congress of the SEA (Sociedad Española de Arteriosclerosis [Spanish Atherosclerosis Society]) held in Cádiz in 2017.