Diabetic amyotrophy or Bruns-Garland syndrome is a rare disorder affecting less than 1% of all diabetic patients. It manifests as unilateral or bilateral muscle pain, weakness and atrophy in the proximal region of the lower limbs. It is more common in the fifth decade of life among patients who have suffered type 2 diabetes for several years. However, the condition is not directly related to the severity of diabetes, and may even precede its diagnosis.1 The underlying etiopathogenesis is multifactorial and little known, and the diagnosis is based on the clinical findings and the exclusion of other possible causes. The present case is of interest in that it suggests a new mechanism that may influence the course of the disease.
A 53-year-old woman presented with reactive depression following the death of a relative and the onset of type 2 diabetes three months before admission, with glycemia 224mg/dl and HbA1c: 10.9%. Weight: 56kg, height: 1.5m; the body mass index (BMI): 24.9kg/m2. Treatment was started with the prescription of a 1200kcal diet and metformin 850mg/12h, with good patient adherence. Concomitant to the diagnosis of type 2 diabetes, she developed right lumbosciatalgia, which subsequently became bilateral, with very poor pain control despite the treatment prescribed (Table 1). The patient was admitted to Neurology for the evaluation of bilateral subacute lumbosacral radiculoplexus neuropathy, exhibiting gradual worsened gait, with falls and the need for crutches over the previous few weeks. She was seen to have lost weight (10kg) from the time of her diabetes diagnosis, this being largely attributable to the prescribed diet. The neurological examination revealed predominantly proximal paraparesis in addition to quadriceps atrophy and areflexia of the lower extremities, with no sphincter involvement. The electromyogram showed bilateral spontaneous activity at L2-S2 level, consistent with lumbosacral radiculoplexus neuropathy, with motor axonal degeneration and abundant signs of acute and active denervation. Lumbar and pelvic magnetic resonance imaging and thoracoabdominal computed tomography ruled out compressive and infiltrative causes. Lumbar puncture showed slightly elevated proteins in the cerebrospinal fluid (0.57g/l), while the remaining parameters proved normal, including histopathology and the microbiological data. The laboratory test results only showed a decrease in HbA1c concentration (6.6%). The liver function and lipid profile, albumin, sideremia, the transferrin saturation index, ferritin, ionogram, calcemia, vitamin D, vitamin B12, and folic acid were all normal. No anti-GAD or anti-ganglioside antibodies were detected, and cytomegalovirus (CMV) and HIV testing proved negative. The funduscopy findings and the absence of microalbuminuria allowed us to discard the possibility of microangiopathic complications.
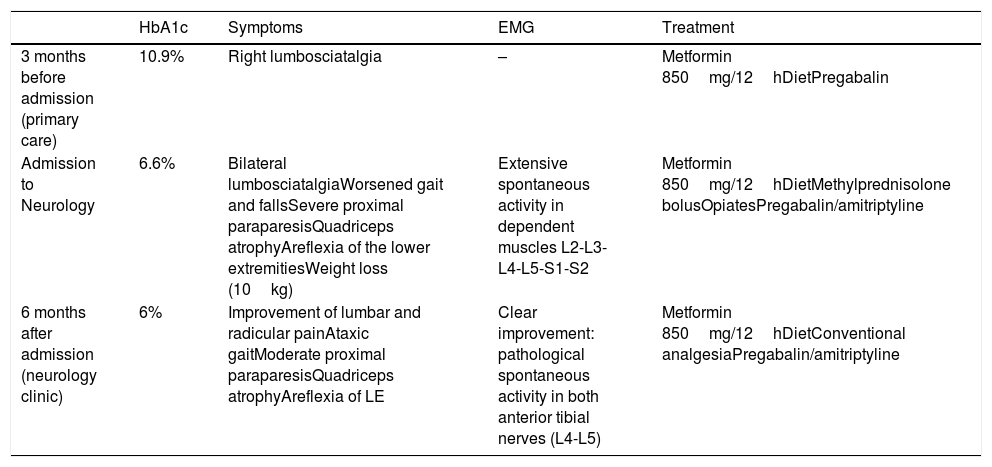
Summary of the present case.
| HbA1c | Symptoms | EMG | Treatment | |
|---|---|---|---|---|
| 3 months before admission (primary care) | 10.9% | Right lumbosciatalgia | – | Metformin 850mg/12hDietPregabalin |
| Admission to Neurology | 6.6% | Bilateral lumbosciatalgiaWorsened gait and fallsSevere proximal paraparesisQuadriceps atrophyAreflexia of the lower extremitiesWeight loss (10kg) | Extensive spontaneous activity in dependent muscles L2-L3-L4-L5-S1-S2 | Metformin 850mg/12hDietMethylprednisolone bolusOpiatesPregabalin/amitriptyline |
| 6 months after admission (neurology clinic) | 6% | Improvement of lumbar and radicular painAtaxic gaitModerate proximal paraparesisQuadriceps atrophyAreflexia of LE | Clear improvement: pathological spontaneous activity in both anterior tibial nerves (L4-L5) | Metformin 850mg/12hDietConventional analgesiaPregabalin/amitriptyline |
LE: lower extremities; EMG: electromyogram; HbA1c: glycosylated hemoglobin.
Having discarded compressive/infiltrative causes, and based on the suggestive clinical findings, Bruns-Garland syndrome was diagnosed. Treatment was started with intravenous boluses of methylprednisolone, opiates for pain control, and rehabilitation. After 5 months, there was less pain and improved motor balance, and part of the medication could be suspended. Table 1 details the clinical characteristics and the electromyographic findings.
In Bruns-Garland syndrome, immune-mediated inflammation is central to the physiopathology of the disorder, causing microvasculitis with the presence of mono- and polymorphonuclear cells and immune complexes and complement activation. Microvascular damage results in ischemia of the vasa nervorum of the nerve roots and plexuses. This causes degenerative axonal damage and demyelination, with subsequent focal atrophy of muscle fibers alternating with healthy fibers. Although the diagnosis is clinical, it is confirmed by the electrodiagnostic findings, showing multifocal axonal damage of the nerve roots and plexuses secondary to demyelination and denervation,2 as seen in our case. Biopsy of the nerve of the affected muscle is reserved for cases posing greater diagnostic difficulties.
Of note in the present case was the important decrease in HbA1c concentration in a short time period (3.3% in 3 months), which may have played a role in the worsening of amyotrophy. In this regard, it is possible that the same unclear mechanisms involved in the transient worsening of diabetic retinopathy as a result of the rapid improvement in glycemic control3,4 could be implicated in the worsening of the microangiopathic alterations of the vasa nervorum in the context of Burns-Garland syndrome. In fact, a similar phenomenon has been described in so-called insulin neuritis, which consists of neuropathy attributed to a rapid improvement in glycemic control using insulin in individuals with a long history of hyperglycemia. Endoneural ischemia and apoptosis due to sudden glucose deprivation have been described as implicated physiopathological elements.5
In conclusion, we report a case of Bruns-Garland syndrome associated with a rapid improvement in glycemic control. This case should cause us to ponder whether the sudden optimization of glycemic control could act as a triggering factor for a poor course of the disease. However, prospective observational studies are needed to support this hypothesis, as well as translational research into the mechanisms involved.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Simó-Servat A, Besora S. Amiotrofia diabética síndrome de Bruns-Garland asociado a rápida mejoría en el control metabólico. Endocrinol Diabetes Nutr. 2020;67:218–219.