To document the opinion of primary care physicians on hypothyroidism and explore their educational and research needs.
MethodsA web-based survey was released through Healthcare Management offices in Madrid to be answered anonymously by the doctors at the health centers.
ResultsFive hundred and forty-six out of 3897 (14%) physicians completed the survey. More than 90% of respondents agreed that hypothyroidism is a common and easily managed health problem and that its poor control increases healthcare costs. This percentage was higher in older doctors and those with longer professional experience. 88.1% of respondents showed interest in educational activities (86.6% in receiving and 20.9% in providing education). The preference for clinical sessions in the health center (71.5%) exceeded that of sessions in the hospital (20.2%), while the preference for online courses (67.8%) exceeded that of face-to-face courses (50.9%). 53.5% of interviewees expressed interest in research on hypothyroidism. Women and professionals with a higher number of hypothyroid patients under their care were more likely to be interested in educational and research activities.
ConclusionPrimary care physicians in the Community of Madrid are aware of the health problem posed by thyroid hormone deficiency and are clearly in favour of participating in educational and research activities in this area of knowledge.
Conocer la opinión de los médicos de atención primaria sobre el hipotiroidismo y explorar sus necesidades formativas y de investigación.
MétodosA través de las direcciones asistenciales de atención primaria de Madrid se divulgó una encuesta basada en la web para ser contestada de forma anónima por los médicos de los centros de salud.
ResultadosQuinientos cuarenta y seis de 3897 (14%) médicos completaron la encuesta. Más del 90% de los encuestados estaba de acuerdo con que el hipotiroidismo es un problema de salud frecuente y de fácil manejo y con que su mal control aumenta el gasto sanitario. Este porcentaje fue mayor en los médicos de mayor edad y experiencia profesional. El 88,1% de los encuestados mostró interés en participar en actividades formativas (el 86,6% en recibir y el 20,9% en impartir formación). La preferencia por sesiones clínicas en el centro de salud (71,5%) superó a la de sesiones en el hospital (20,2%), mientras que la preferencia por cursos online (67,8%) superó a la de cursos presenciales (50,9%). El 53,5% de los entrevistados manifestó interés por la investigación en hipotiroidismo. Las mujeres y los profesionales con mayor número de pacientes hipotiroideos en sus consultas fueron más proclives a interesarse por actividades formativas y de investigación.
ConclusiónLos médicos de atención primaria de la Comunidad de Madrid son conscientes del problema sanitario que representa la deficiencia de hormona tiroidea y se muestran claramente favorables a la participación en actividades docentes y de investigación en esta área de conocimiento.
Hypothyroidism is the most common hormone deficiency among the general population and is predominantly managed in the primary care (PC) setting1. Large epidemiological studies have shown that the approximate prevalence of hypothyroidism in the general population ranges from 2% to 10%, that it is more common in women and that its incidence increases with age2,3. A recent Spanish study using PC registries found that 4.2% of men and 13.3% of women had hypothyroidism and that these percentages increased to 5.6–8.8% and 12.5–14.2%, respectively, in men and women over the age of 60 years4.
Hypothyroidism is generally considered easy to manage, and levothyroxine is well tolerated5. However, even though the benefits of hormone replacement therapy for hypothyroidism are irrefutable, poor disease control, whether due to deficient or excess levothyroxine, is a common clinical issue6. Overtreatment with levothyroxine, which manifests as a fall in serum thyroid-stimulating hormone (TSH) levels, increases the risk of cardiovascular disease and fractures7. In contrast, undertreatment, which manifests as elevated TSH levels, is associated with a greater risk of dyslipidaemia and ischaemic heart disease8. Both scenarios result in more medical appointments and complementary tests and, therefore, greater healthcare costs.
Even though most hypothyroid patients are diagnosed and treated by their GPs, information about the management of hypothyroidism in the Spanish PC setting is very scarce. In fact, clinical guidelines of this hormone deficiency in family medicine journals are rare9 and, to date, only one survey on the management of hypothyroidism by primary care doctors has been published10. The aims of this study were: 1) to find what primary care doctors think about hypothyroidism as a health problem; and 2) to analyse their educational and research needs in this medical field.
Material and methodsStudy designA survey aimed at PC doctors working in the Community of Madrid was designed10. The target population of our study therefore consisted of all GPs working within the regional primary care system (GAAP) of the Community of Madrid (n = 3897), that is, within the Madrid public health system which, at the time of the study, served 6,784,804 inhabitants11.
The survey comprised questions about demographic data, the attitude of doctors to the screening, diagnosis and treatment of hypothyroidism and, finally, what they thought about hypothyroidism and their educational and research needs in this medical field. The results of these latter aspects – what PC doctors thought about hypothyroidism and their educational and research needs – are discussed in this article. Our study focussed exclusively on primary hypothyroidism in adult patients. Secondary hypothyroidism was excluded due to its low prevalence, as was hypothyroidism in children and pregnant women due to its special clinical characteristics.
This study was approved by the Hospital Universitario Puerta de Hierro Majadahonda Independent Ethics Committee and by the GAAP Central Research Committee (code 37/19). After its approval, the Directors of the GAAP's seven healthcare directorates were informed of our project so that it could be forwarded to all the healthcare centres of Madrid. The survey was hosted on a forms creation website (https://www.google.com/forms/about/?utm_source=gaboutpage&utm_medium=formslink&utm_campaign=gabout) so that it could be answered anonymously and voluntarily. The password-protected data were stored on the website until the end of the established time frame, at which point they were collated in a database for statistical processing.
Question creation strategyMost of the questions were specifically designed to be yes or no questions. Other questions were multiple choice, with the possibility to choose one or more of the possible answers. To avoid bias in the multiple-choice questions, wording that led the respondent to a particular answer was avoided as far as possible, and a wide range of options arranged alphabetically or randomly was included.
The questions asking the opinion of the doctors explored four specific aspects of clinical practice: 1) disease frequency (I believe that hypothyroidism is a common health problem that should concern primary care doctors); 2) the health expenditure that it entails (I believe that poorly-controlled hypothyroidism increases the use of resources and healthcare costs); 3) the difficulty managing hypothyroidism in primary care (I believe that treatment with levothyroxine is easy to manage and does not usually cause my patients any problems); and 4) treatment adherence (I believe that most of my patients take their levothyroxine tablets correctly).
Regarding the questions about educational and research needs, the participants were asked if they were interested in these activities, and those who answered "Yes" were then asked to specify their preferred formats for both activities.
Statistical analysisThe results are shown as mean (standard deviation [SD]) for normal data and median (interquartile range [IQR]) for non-parametric data. The Kolmogorov-Smirnov test was used to check the goodness of fit to a normal distribution. Student's t-test was used to compare means between two groups if the data fit a normal distribution, while the Mann-Whitney U test was used for data that did not fit a normal distribution. The qualitative variables are described as absolute values and percentages. Given that not all participants answered all the questions, on some occasions, it was necessary to indicate the sample size used for the statistical calculations. The chi-squared test and Fisher's exact test were used to compare proportions. A p-value less than 0.05 was considered statistically significant.
ResultsProfessionals surveyedIn total, 556 doctors completed the survey, 10 of which were excluded owing to a lack of data, leaving 546 valid surveys. Most of the respondents were women (74.0%), the mean age was 50.9 (8.5) years and the length of time in professional practice was 23.8 (8.3) years. The demographic data of the doctors surveyed, including their geographical distribution in the Community of Madrid, is shown in Table 1.
Demographic and professional characteristics of the GPs participating in the study.
| All(n = 546) | Women(n = 404) | Men(n = 142) | |
|---|---|---|---|
| Age, years | 50.9 (8.5) | 50.3 (8.5) | 52.4 (8.3)* |
| Years of professional experience | 23.8 (8.3) | 23.2 (8.3) | 25.3 (8.2)** |
| Non-healthcare activities | |||
| Any | 352 (64.5) | 256 (63.4) | 96 (67.6) |
| Teaching activity | 298 (45.4) | 211 (54.7) | 77 (54.2) |
| Research activity | 98 (17.9) | 70 (17.3) | 28 (19.7) |
| Management activity | 71 (13.0) | 50 (12.4) | 231 (14.8) |
| Number of hypothyroid patients seen per year | |||
| New diagnosis | 7 (5−12) | 7 (5−12) | 7 (5−10) |
| In follow-up | 50 (30−90) | 50 (30−90) | 50 (30−90) |
| Health area | |||
| South | 62 (11.4) | 50 (12.4) | 12 (8.5) |
| North | 67 (12.3) | 52 (12.9) | 15 (10.6) |
| North-east | 80 (14.7) | 61 (15.1) | 19 (13.4) |
| East | 99 (18.1) | 80 (19.8) | 19 (13.4) |
| West | 61 (11.2) | 46 (11.4) | 15 (10.6) |
| Central | 70 (12.8) | 43 (10.6) | 27 (19.0) |
| South-east | 107 (19.6) | 72 (17.8) | 35 (24.6) |
The data represent the mean (SD) for quantitative variables of normal distribution (age, professional experience) or the median (interquartile range) for quantitative variables of non-normal distribution (number of hypothyroid patients seen per year) and the number (percentage) for qualitative variables (non-healthcare activities, health areas).
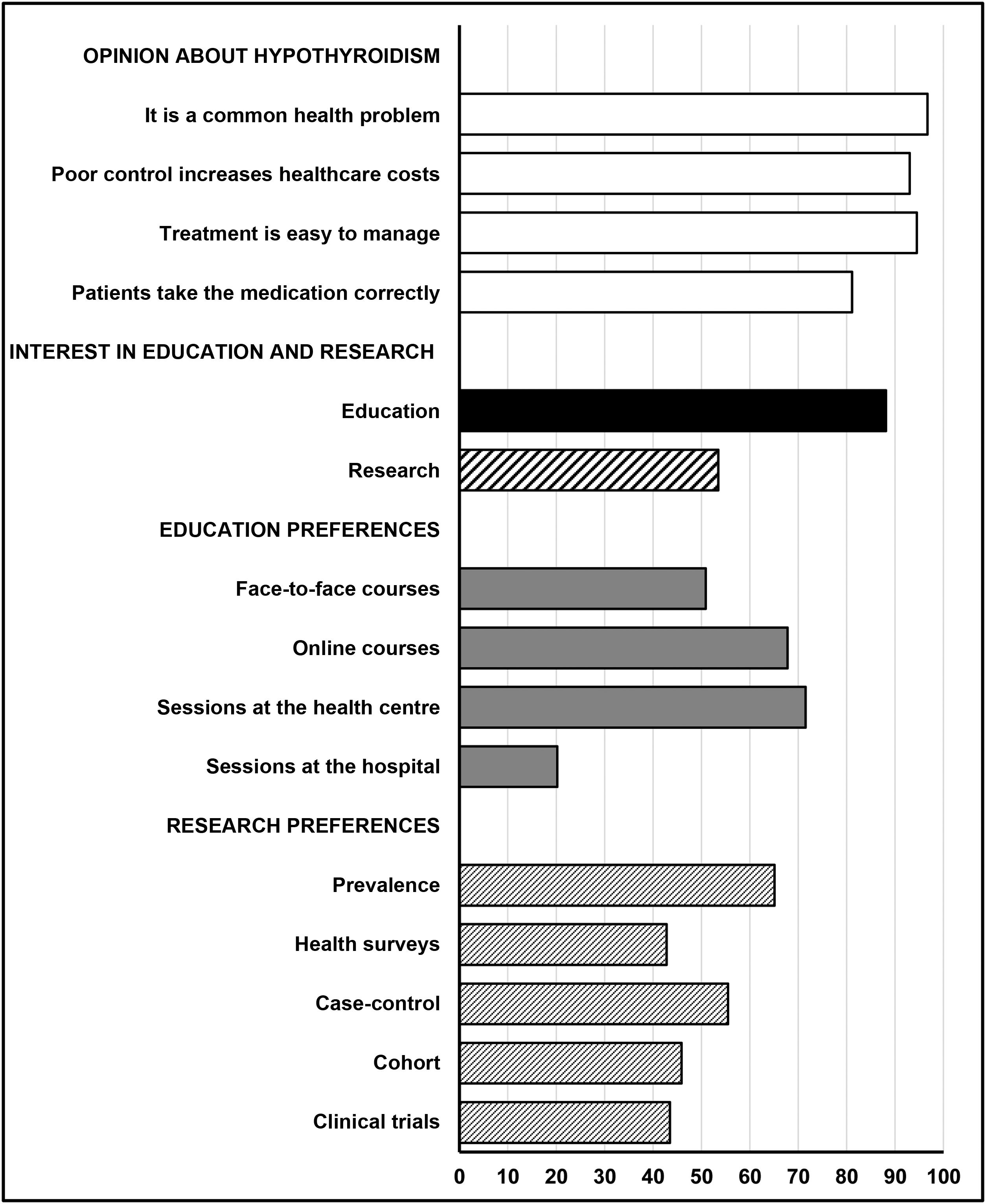
Most of the GPs agreed that hypothyroidism is a common health problem that should concern them (96.7%), that poorly-controlled hypothyroidism increases the use of resources and healthcare costs (93.0%) and that treatment with levothyroxine is easy to manage and does not usually cause patients any problems (94.5%). Moreover, 81.1% believed that their patients were taking their levothyroxine tablets correctly (Fig. 1).
Doctors who believed hypothyroidism is a common health problem that is easy to treat were significantly older and had significantly more professional experience than those who did not think this (Table 2). In contrast, no significant relationship was found between the opinions of the respondents and the number of hypothyroid patients seen in their practice, new patients or patients in follow-up (Table 2), nor with gender or non-healthcare professional activities (data not shown).
Influence on the opinion and interests of GPs of age, professional experience and number of hypothyroid patients seen.
| Age (years) | Years of experience | Newly-diagnosed patients | Patients in follow-up | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Mean (SD) | N | Mean (SD) | N | Median (IQR) | N | Median (IQR) | ||
| Opinion about hypothyroidism | |||||||||
| It is a common health problem | No | 18 | 41.9 (8.3) | 18 | 15.1 (7.3) | 18 | 7.5 (4.5−12) | 18 | 42 (30−57.5) |
| Yes | 528 | 52.1 (8.3) ** | 528 | 24.0 (8.2)** | 507 | 7 (5−12) | 499 | 50 (30−90) | |
| Poor control increases healthcare costs | No | 38 | 49.8 (9.5) | 38 | 23.0 (9.0) | 36 | 8 (5−10) | 36 | 47.5 (30−60) |
| Yes | 508 | 50.9 (8.4) | 508 | 23.8 (8.3) | 489 | 7 (5−12) | 481 | 50 (30−90) | |
| Treatment is easy to manage | No | 30 | 47.1 (9.3) | 30 | 20.1 (9.1) | 30 | 6 (5−12) | 30 | 35 (30−62.5) |
| Yes | 516 | 51.1 (8.4) * | 516 | 24.0 (8.2)* | 495 | 7 (5−12) | 487 | 50 (30−90) | |
| Patients take the medication correctly | No | 103 | 49.4 (8.8) | 103 | 22.5 (8.7) | 98 | 8 (5−15) | 96 | 50 (30−100) |
| Yes | 443 | 51.2 (8.4) | 443 | 24.0 (8.2) | 427 | 7 (5−10) | 421 | 50 (30−80) | |
| Interest in activities about hypothyroidism | |||||||||
| Education | No | 65 | 51.1 (8.6) | 65 | 24.2 (8.4) | 62 | 5 (4−10) | 62 | 50 (25−82.5) |
| Yes | 481 | 50.8 (8.5) | 481 | 23.7 (8.3) | 463 | 8 (5−12)* | 455 | 50 (30−90) | |
| Research | No | 254 | 50.6 (9.0) | 254 | 23.4 (8.8) | 243 | 6 (4−10) | 239 | 40 (30−80) |
| Yes | 292 | 51.0 (8.1) | 292 | 24.1 (7.9) | 282 | 8 (5−12)* | 278 | 50 (30−100)* | |
The data represent the mean (SD) for quantitative variables of normal distribution (age, years of experience) or the median (interquartile range) for non-parametric quantitative variables (newly-diagnosed patients, patients in follow-up).
Of the 546 professionals surveyed, 481 (88.1%) were interested in participating in educational activities on hypothyroidism. Specifically, 473 (86.6%) were interested in receiving training and 144 (20.9%) also in participating as teachers. In order of popularity, the preferred activities were: sessions at the health centre (71.5%), online courses (67.8%), face-to-face courses (50.9%) and clinical sessions at the hospital (20.2%) (Fig. 1).
Interest in educational activities was not related to age or years of professional experience but was associated with the number of newly-diagnosed hypothyroid patients (Table 2). Interest in these activities was significantly higher in women (93.1% vs 73.9%; p < 0.01), both in general education and training to be an assistant. However, it was not related to the conduct of non-healthcare activities (Table 3). No significant relationships were found between the different types of educational activity and gender or the conduct of non-healthcare activities, with the only exception being that professionals who also conducted research were more favourable to in-hospital clinical sessions than those not involved in research (28.9% vs 18.2%; p < 0.05) (Table 4).
Primary care doctors' interest in participating in hypothyroidism educational and research activities.
| Activities of interest | Gender | Teaching activity | Research activity | Management activity | ||||
|---|---|---|---|---|---|---|---|---|
| Women(404) | Men(142) | No(248) | Yes(298) | No(448) | Yes(98) | No(475) | Yes(71) | |
| General education | 376 (93.1) | 105 (73.9)*** | 215 (86.7) | 266 (89.3) | 391 (87.3) | 90 (91.8) | 419 (88.2) | 62 (87.3) |
| Learning | 370 (91.6) | 103 (75.2)*** | 213 (85.9) | 260 (87.2) | 386 (86.2) | 87 (88.8) | 413 (86.9) | 60 (84.5) |
| Teaching | 87 (21.5) | 27 (19.0) | 39 (15.7) | 75 (25.2)** | 82 (18.3) | 32 (37.2)** | 95 (20.0) | 19 (26.8) |
| Research | 227 (56.2) | 65 (45.8)* | 108 (43.5) | 184 (61.7)*** | 222 (49.6) | 70 (71.4)*** | 246 (51.8) | 46 (64.8)* |
The data represent the absolute values (percentages) of affirmative answers for each of the activities of interest about which they were asked.
The numbers in brackets in the headings of each column denote the number of subjects in each group or subgroup.
Types of educational activity favoured by the primary care doctors who expressed an interest in hypothyroidism training.
| Type of educational activity | Gender | Teaching activity | Research activity | Management activity | ||||
|---|---|---|---|---|---|---|---|---|
| Women(376) | Men(105) | No(215) | Yes(266) | No(391) | Yes(90) | No(419) | Yes(62) | |
| Face-to-face courses | 186 (49.5) | 59 (56.2) | 106 (49.3) | 139 (52.3) | 195 (49.9) | 50 (55.6) | 214 (51.1) | 31 (50.0) |
| Online courses | 261 (69.4) | 65 (61.9) | 146 (67.9) | 180 (67.7) | 262 (67.0) | 64 (71.1) | 278 (66.3) | 48 (77.4) |
| Clinical sessions at the health centre | 270 (71.8) | 74 (70.5) | 144 (67.0) | 200 (75.2) | 274 (70.1) | 70 (77.8) | 295 (70.4) | 49 (79.0) |
| Clinical sessions at the hospital | 80 (21.3) | 17 (16.2) | 41 (19.1) | 56 (21.1) | 71 (18.2) | 26 (28.9)* | 80 (19.1) | 17 (27.4) |
The data represent the absolute values (percentages) of affirmative answers for each of the activities of interest about which they were asked.
The numbers in brackets in the headings of each column denote the number of subjects in each group or subgroup.
In total, 292 patients (53.5%) were interested in participating in some research projects. Their preferences were: prevalence studies (65.1%), case-control studies (55.5%), cohort studies (45.9%), clinical trials (43.5%) and health surveys (42.8%) (Fig. 1).
GPs interested in research saw a greater number of hypothyroid patients in their practice (Table 2). Interest in research was significantly higher among women than men (56.2% vs 45.8%; p < 0.05) as well as among professionals who had already conducted non-healthcare activities versus those who had not, whether teaching (61.7% vs 43.5%; p < 0.001), research (71.4% vs 49.6%; p < 0.001) or management (64.8% vs 51.8%, p < 0.05) (Table 3).
In terms of types of research, it was observed that a significantly higher proportion of men preferred cohort studies than women (58.5% vs 42.3%; p < 0.05). A greater proportion of research doctors preferred cohort studies (57.1% vs 42.3%; p < 0.05) and clinical trials (58.6% vs 38.7%; p < 0.05) than doctors not involved in research activities. Professionals involved in management tended to prefer case-control studies to those who did not perform such activities (71.7% vs 52.4%; p < 0.05) (Table 5).
Types of research activity favoured by the primary care doctors who expressed an interest in hypothyroidism research.
| Type of research activity | Gender | Teaching activity | Research activity | Management activity | ||||
|---|---|---|---|---|---|---|---|---|
| Women(227) | Men(65) | No(108) | Yes(184) | No(222) | Yes(70) | No(246) | Yes(46) | |
| Prevalence studies | 153 (67.4) | 37 (56.9) | 68 (63.0) | 122 (66.3) | 136 (61.3) | 54 (77.1)* | 155 (63.0) | 35 (76.1) |
| Health surveys | 104 (45.8) | 21 (32.3) | 42 (38.9) | 83 (45.1) | 91 (41.0) | 34 (48.6) | 104 (42.3) | 21 (45.7) |
| Case-control studies | 124 (54.6) | 38 (58.5) | 64 (59.3) | 98 (53.3) | 118 (53.2) | 44 (62.9) | 129 (52.4) | 33 (71.7)* |
| Cohort studies | 96 (42.3) | 38 (58.5)* | 56 (51.9) | 78 (42.4) | 94 (42.3) | 40 (57.1)* | 108 (43.9) | 26 (56.5) |
| Clinical trials | 94 (41.4) | 33 (50.8) | 39 (36.1) | 88 (47.8) | 86 (38.7) | 41 (58.6)** | 110 (44.7) | 17 (37.0) |
The data represent the absolute values (percentages) of affirmative answers for each of the activities of interest about which they were asked.
The numbers in brackets in the headings of each column denote the number of subjects in each group or subgroup.
This is the first Spanish study to present PC doctors' opinions on hypothyroidism and their educational and research needs in this medical field. The importance of hypothyroidism as a health problem and its growth in recent years is beyond doubt, as shown by the fact that thyroid hormone prescriptions have doubled over the last 20 years12. The primary care doctors of the Community of Madrid are aware of this problem, as shown by the positive responses given by more than 90% of those surveyed to questions about its prevalence and the healthcare costs associated with its poor control. Moreover, the majority recognise that it is relatively easy to treat, and more than 80% believe that patients take their medication correctly. Older doctors and those with more experience are more inclined to think hypothyroidism is common and easy to manage. Although in line with other studies5,13, this opinion contradicts the data in the literature, which show that poor hypothyroidism treatment and control is common. In the Colorado study, just 60% of patients who took thyroid medication had TSH levels within normal range2, while in a Spanish study, 32.5% of hypothyroid patients exhibited abnormal TSH values6.
Continuing medical education can be part of a lifelong learning process that doctors undertake from the onset of their professional careers to keep up-to-date14. It facilitates competent clinical practice and is essential to achieve a high standard of healthcare. The primary care doctors of Madrid are aware of this, as shown by the fact that more than 90% of those surveyed expressed an interest in educational activities in hypothyroidism. As might be expected, doctors who see more hypothyroid patients and those involved in teaching and research activities showed a greater interest in both educational and research activities.
It is striking that most doctors surveyed considered hypothyroidism to be easy to manage yet still wished to receive training. This suggests they face problems or difficulties managing these patients in their clinical practice. As such, the doctors' interest in hypothyroidism educational activities could be related to gaps in their knowledge of this hormone deficiency, as has been shown in other studies13. It has been observed that the main driver for GPs' learning was discomfort during their daily work if a possible lack of knowledge or skills was perceived15. Several studies suggest that educational initiatives improve doctors' knowledge and skills in managing common chronic conditions like diabetes16, so it is reasonable to think such initiatives may also have a considerable impact on understanding thyroid diseases.
Travel issues and time constraints could explain why clinical sessions in the workplace rather than in the hospital were the preferred choice for most respondents. However, it is noteworthy that online courses were far preferable than face-to-face courses. This preference is consistent with other studies, showing that online learning is widely accepted among doctors17 and is an effective teaching method18. Online courses offer advantages such as a wide variety of content, flexible training times, easy access for geographically dispersed learners and greater adaptability to individual learner styles18. A recent systematic review showed a positive impact of online education in terms of GPs' knowledge and satisfaction19. In line with this, almost 80% of our respondents favour online learning. However, there are also barriers to this intervention, such as time constraints, poor technical skills, inadequate infrastructure and absence of institutional support20. Lack of personal interaction with colleagues and teachers can also be a drawback21. However, in this study, online learning was selected mainly in addition to face-to-face courses and sessions, but not instead, suggesting that the flexibility offered by online education is valued as additional to the benefits of a face-to-face experience.
More than half of respondents expressed an interest in participating in research, particularly women and doctors already performing non-healthcare activities. Research is one of the key functions of PC teams and contributes quality, effectiveness and efficiency to health services by supporting care informed on a scientific basis22. Our data seem consistent with previous findings showing that Spanish primary care doctors have a favourable attitude towards research23.
Although research advantages for both patients and professionals are well established, this activity is not without difficulties. PC doctors are aware of these and have identified several in previous studies, including care pressure, lack of time, institutional shortcomings, lack of multicentre lines of research, lack of incentives and preparation, and lack of motivation23,24. Lack of resources and support staff are also barriers that must be overcome24. Despite this, hypothyroidism is a disorder that lends itself to research in the primary care setting as it is a prevalent chronic condition. Moreover, it is precisely primary care doctors who remain in touch with patients throughout their lives and are ideally placed to detect the most common diseases in their earliest stages, facilitating direct access to the natural history of the disorder.
Our study suffers from the same limitations inherent to all surveys of professionals. In addition, its scope is restricted to hypothyroidism and the Community of Madrid, so it may not be possible to extrapolate its results to other chronic conditions or geographical areas. It is also possible that those doctors with a greater interest in hypothyroidism were more inclined to respond to the survey. Our study focused on exploring the educational and research needs of the doctors surveyed. However, it should be recognised that both training and research must go beyond the mere acquisition of knowledge, as they should be focussed on improving skills and performance. This is something that only future research will be able to establish.
However, it should be recognised that training and research must go beyond mere knowledge acquisition, as they should be focused on improving skills and performance. This is something that only future research will be able to establish. Moreover, the geographical distribution was similar, and all health areas achieved a response rate of at least 10%. These data are also of interest for clinical practice, given that PC doctors experience the disease first-hand and provide ongoing care to chronic patients. Our survey indirectly reflects the impact of the marked increase in women in clinical practice. The fact that women tend to prioritise teaching activities over research, as shown in Table 3, may have implications for current or future clinical practice and is worthy of more specific research. Our findings are also of interest from a health planning perspective, as if we deem continuing medical education to be the ethical responsibility of all doctors, it is also true that employers and health authorities have an increasing duty to train their professionals25.
Our previous study10 found that PC doctors had a proactive attitude towards the treatment and follow-up of their hypothyroid patients and that, despite slight deviations, they followed the recommendations proposed in the international guidelines. However, even though treating hypothyroidism is simple, PC professionals should be aware that levothyroxine replacement therapy undertreatment is associated with a negative impact on quality of life26 and an increased risk of heart disease27. In contrast, overtreatment with excessive doses of levothyroxine increases the risk of arrhythmia, cardiovascular disease and fractures7,28. We believe that the continuing medical education of doctors is a fundamental pillar for preventing or minimising these undesirable effects on the population's health.
In conclusion, PC doctors of the Community of Madrid are aware of the health problem of hypothyroidism, and the majority favour participating in teaching and research activities in this medical field. In the authors' opinion, better training of general practitioners, together with the research results they generate, could optimise the treatment of hypothyroid patients, reduce complications associated with abnormal TSH levels and decrease healthcare costs. Prospective interventional studies evaluating the effect of continuing medical education programmes on clinical outcomes that add value to patients with hypothyroidism are required.
Conflicts of interestThe authors declare that they have no conflicts of interest in relation to this study.
The authors would like to thank the seven healthcare directorates of Madrid who helped disseminate our survey and the primary care doctors who took the time to complete this survey.