To assess remission of type 2 diabetes mellitus (T2DM) after bariatric surgery, to analyze potential conditioning factors, and to compare Spanish and American remission criteria.
Material and methodsA retrospective study of diabetic patients undergoing Roux-en-Y gastric bypass from 2009 to 2015. Data collected included age, sex, time since T2DM diagnosis, antidiabetic drugs, insulin (type and dose), weight and BMI, percent excess weight lost, HbA1c, blood glucose levels, and course of T2DM after surgery according to Spanish and American criteria, including a descriptive analysis and correlation between both.
ResultsThe study sample consisted of 106 patients. Outcomes one year after surgery was as follows (Spanish criteria): complete remission 65.9%, partial remission 5.5%, improvement 18.9%, no change 9.7% (at 5 years: 68.4, 5.3, 10.5, and 15.8%, respectively). Outcomes according to ADA criteria were as follows: complete remission 61.5%, partial remission 5.3%, and no remission 28.6% (after 5 years, complete remission 68.4%). There was a good correlation between both classifications (rho=0.974; p<0.001). Mean HbA1c levels: 7.3±1.8% at baseline; 5.7±1% at one year; 6.3±1.2% at 5 years. Chance of remission was lower in patients aged over 50 years (54.4% vs. 88.2%; p=0.001), with T2DM diagnosed more than 10 years before (26.3% vs. 81.8%; p<0.001), on insulin treatment (31.3% vs. 87.9%; p<0.001), and with HbA1c levels ≥8% (40% vs. 77%; p=0.001).
ConclusionsAt our hospital, bariatric surgery is associated to a high remission rate of T2DM in patients with morbid obesity, with a good correlation between Spanish and American criteria. Age over 50 years old, long T2DM duration, poorer baseline metabolic control, and previous insulin treatment are markers of poorer response.
Evaluar la remisión de la diabetes mellitus tipo 2 (DM-2) tras cirugía bariátrica; analizar potenciales factores condicionantes y comparar criterios de remisión nacionales y americanos.
Material y métodosEstudio retrospectivo de pacientes diabéticos sometidos a bypass gástrico en Y de Roux entre 2009-2015. Variables recogidas: edad, sexo, años de evolución de DM-2, antidiabéticos, insulina (tipo y dosis), peso e IMC, porcentaje de sobrepeso perdido, HbA1c, glucemia y evolución de la DM-2 tras cirugía según criterios nacionales y americanos. Análisis descriptivo y correlación entre ambos consensos.
ResultadosSe incluyeron 106 pacientes. Al año de la intervención (criterios nacionales): remisión completa 65,9%, remisión parcial 5,5%, mejoría 18,9% y sin cambios 9,7% (a los 5 años: 68,4; 5,3; 10,5 y 15,8%, respectivamente). Según criterios ADA: remisión completa 61,5%, remisión parcial 5,3% y sin remisión 28,6% (a los 5 años, remisión completa 68,4%). Buena correlación entre ambas clasificaciones (Rho=0,974; p<0,001). HbA1c media inicial: 7,3±1,8%; al año: 5,7±1%; a 5 años: 6,3±1,2%. Resultaron marcadores de peor probabilidad de remisión: edad superior a 50 años (54,4 vs. 88,2%; p=0,001), DM-2 de más de 10 años (26,3 vs. 81,8%; p<0,001), tratamiento con insulina (31,3 vs. 87,9%; p<0,001) y HbA1c≥8% (40 vs. 77%; p=0,001).
ConclusionesEn nuestro centro, la cirugía bariátrica se asocia a una elevada tasa de remisión de DM-2 en pacientes con obesidad mórbida intervenidos, existiendo una buena correlación entre los criterios nacionales y los americanos. La edad superior a 50 años, una larga evolución de la DM-2, un peor control metabólico inicial y el tratamiento previo con insulina son marcadores de peor respuesta.
Obesity and type 2 diabetes mellitus (DM2) are leading public health problems due to their high and increasing prevalence and important associated healthcare costs.1,2. In Spain, the Di@bet.es study confirmed the high prevalence of DM2 (13.8%), as well as the clear link between both disorders (>50% of all diabetics were obese).3 The Canary Islands heads the Spanish national ranking for the prevalence of both disorders, as well as for mortality attributable to diabetes.4
The optimal approach to both disease conditions remains a challenge for clinicians. Lifestyle modifications and drug treatments afford modest weight reductions (usually <10%), but the reversal of DM2 is not achieved. Even adequate metabolic control is often not reached. The possibility of using bariatric surgery (BS) as a treatment strategy for reverting or improving DM2 is attracting increasing interest. Many data show metabolic surgery to afford improved glycemic control and to reduce the cardiovascular risk factors in patients with obesity and DM2 as compared to different medical interventions.5
Bariatric surgery exerts potent action at different levels simultaneously. Apart from the restrictive and/or malabsorptive component of the different procedures, which limits nutrient intake or absorption, respectively, BS is characterized by an endocrine and biochemical regulatory component that facilitates dramatic weight loss, and this in turn results in important improvements in carbohydrate metabolism. The known underlying mechanisms include increased levels of peptide YY (anorexigenic action) and decreased ghrelin levels (orexigenic action). In turn, the incretin effect of surgery, with increased circulating levels of GLP-1 and GIP, stimulates insulin secretion, lowers glucagon secretion, and increases the sensation of satiety at the level of the central nervous system.6 Although no studies are available in our setting, a number of trials7–10 have demonstrated a significant increase in DM2 remission as compared to conventional therapy up to 5 years following surgery, even in patients with grade 1 obesity or overweight.
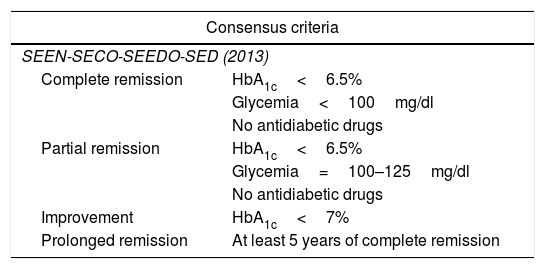
It is difficult to establish comparisons among the existing studies, since the DM2 remission criteria used are different. This has obliged the main scientific bodies to position themselves on this matter. The most commonly used criteria in our setting are those of the SEEN-SECO-SEEDO-SED consensus of 201311 and those of the American Diabetes Association (ADA) of 200912 (Table 1).
Type 2 diabetes mellitus remission criteria.
| Consensus criteria | |
|---|---|
| SEEN-SECO-SEEDO-SED (2013) | |
| Complete remission | HbA1c<6.5% |
| Glycemia<100mg/dl | |
| No antidiabetic drugs | |
| Partial remission | HbA1c<6.5% |
| Glycemia=100–125mg/dl | |
| No antidiabetic drugs | |
| Improvement | HbA1c<7% |
| Prolonged remission | At least 5 years of complete remission |
| No changes | Remaining cases |
|---|---|
| ADA (2009) consensus criteria | |
| Complete remission | HbA1c<6% |
| Blood glucose<100mg/dl | |
| No antidiabetic drugs | |
| Partial remission | HbA1c<6.5% |
| Blood glucose=100–125mg/dl | |
| No antidiabetic drugs | |
| Prolonged remission | At least 5 years of complete remission |
| No changes | Remaining cases |
ADA: American Diabetes Association; HbA1c: glycosylated hemoglobin; SECO: Sociedad Española de Cirugía de la Obesidad; SED: Sociedad Española de Diabetes; SEEDO: Sociedad Española para el Estudio de la Obesidad; SEEN: Sociedad Española de Endocrinología y Nutrición.
The present study was designed to analyze the potential benefit of BS in patients with DM2 in our setting, as well as to identify the factors associated with an improved response, with a view to allowing the selection of those patients who stand to benefit most from BS. Lastly, an analysis was made of the correlation between the DM2 remission classifications of the Spanish national and American consensuses.
Material and methodsA retrospective study was made of diabetic patients monitored at nutrition clinics following Roux-en-Y gastric bypass surgery (RYGB) between January 2009 and November 2015 (n=106). A variant of RYGB adjusted to the body mass index (BMI) is performed at our center. It involves the creation of a small gastric reservoir with a capacity of about 15–30ml, a 100-cm biliopancreatic loop, and a feed loop with a length conditioned to the BMI:
- -
Patients with a BMI 40–45kg/m2: 170cm feed loop.
- -
Patients with a BMI 45–50kg/m2: 260cm feed loop.
- -
Patients with a BMI 50–55kg/m2: 350cm feed loop.
- -
Patients with a BMI 55–60kg/m2: 440cm feed loop.
- -
Patients with a BMI >60kg/m: 530cm feed loop.
We always check that there is at least 180cm of common loop.
The following variables were recorded: age, gender, years from diabetes onset, antidiabetic treatment, the type and dose of insulin, the date of surgery, the surgical procedure, weight and the BMI (maximum, presurgery and at each annual visit), the percentage of overweight lost, DM progression after surgery (according to Spanish national and American consensus criteria), HbA1c and glycemia at each annual visit. A descriptive analysis of the above variables was made, and correlations were established between the classifications of both consensuses. In order to identify possible predictors of DM remission in the patients operated on, we divided the sample into two groups: (a) patients in complete remission; and (b) the remainder of the sample. The following variables were compared between the two groups: age, time from DM onset, insulin treatment before surgery, and the BMI before surgery.
Statistical analysisQualitative variables were reported with their frequency distribution. Quantitative variables were reported as the mean±standard deviation (SD). Continuous variables were compared using the Student t-test, while categorical variables were contrasted with the chi-squared test. Statistical significance was considered for p<0.05. The SPSS version 24 statistical package (IBM, 2016) was used throughout.
ResultsPatients undergoing RYGB in the period January 2009 and November 2015 were included in the study. Table 2 shows the baseline characteristics of the patients.
Baseline characteristics of the study sample.
| Cohort (n=106) | |
|---|---|
| Age (years), mean±SD | 51.8±9.1 |
| Female gender, n (%) | 88 (83) |
| Duration of DM2 (years), mean±SD | 6.6±5.6 |
| Pharmacological treatment | |
| OADs, n (%) | 95 (89.6) |
| A-GLP-1 | 10 (9.4) |
| Insulin, n (%) | 37 (34.9) |
| Baseline | 11 (10.4) |
| Mixtures | 16 (15.1) |
| Bolus-basal | 10 (9.4) |
| Daily insulin dose (U/day), mean±SD | 86.2±47.8 |
| Maximum weight (kg), mean±SD | 129.5±21.1 |
| Maximum BMI (kg/m2), mean±SD | 49.6±6.6 |
| Weight before surgery (kg), mean±SD | 119.9±20.2 |
| BMI before surgery (kg/m2), mean±SD | 45.7±5.9 |
| HbA1c(%), mean±SD | 7.3±1.8 |
GLP-1 A: glucagon-like peptide-1 analog; OADs: oral antidiabetic drugs; SD: standard deviation; DM2: type 2 diabetes mellitus; HbA1c: glycosylated hemoglobin; BMI: body mass index.
The mean duration of follow-up was 3.5 years (range: 1–8). Table 3 shows the evolutive changes of the anthropometric and metabolic parameters and of DM in the first 5 years after surgery. A very good correlation was observed between the Spanish national and American classifications of DM remission after BS (rho=0.974; p<0.001) (Fig. 1).
Evolution of anthropometric and metabolic parameters.
| 1 year | 2 years | 3 years | 4 years | 5 years | |
|---|---|---|---|---|---|
| n | 106 | 101 | 49 | 29 | 23 |
| BMI | 31.3±4.4 | 30.9±4.3 | 30.7±3.9 | 31.9±3.6 | 32.9±4.1 |
| POL | 59.4±22.4 | 61.5±16 | 62.6±17.2 | 57.4±13.3 | 53.5±15.3 |
| Glucose | 97.8±30.6 | 103.8±37.7 | 109.1±36.9 | 106.6±36.8 | 107.6±34.5 |
| HbA1c | 5.7±1 | 5.8±1 | 6.2±1.1 | 6.2±1 | 6.3±1.2 |
| DM (1) | |||||
| CR | 65.9% | 68.2% | 53.8% | 61.9% | 68.4% |
| PR | 5.5% | 2.3% | 7.7% | 14.3% | 5.3% |
| I | 18.9% | 27.3% | 23.1% | 23.8% | 10.5% |
| DM (2) | |||||
| CR | 61.5% | 65.9% | 57.7% | 57.1% | 68.4% |
| PR | 9.9% | 4.5% | 3.8% | 19% | 5.3% |
DM (1): evolution of type 2 diabetes mellitus according to Spanish national consensus criteria; DM (2): evolution of type 2 diabetes mellitus according to American Diabetes Association (ADA) consensus criteria; BMI: body mass index; I: improvement; POL: percentage overweight lost; CR: complete remission; PR: partial remission.
The identified markers of a lesser probability of achieving DM remission after surgery (according to national criteria) were: age >50 years (54.4% vs. 88.2%; p=0.001), DM2 duration >10 years (26.3% vs. 81.8%; p<0.001), HbA1c≥8% before surgery (40% vs. 77%; p=0.001) and treatment with insulin before surgery (31.3% vs. 87.9%; p<0.001). By contrast, no association with DM2 remission was observed for the BMI before surgery (p=0.729) or for the percentage overweight lost after BS (p=0.710) (Fig. 2). The behavior with the ADA criteria was identical, the markers of a lesser probability of achieving DM remission after surgery being: age >50 years (49.1% vs. 79.4%; p=0.004), DM2 duration >10 years (26.3% vs. 72.7%; p<0.001), HbA1c≥8% before surgery (36% vs. 68.9%; p=0.005) and treatment with insulin before surgery (21.9% vs. 82.8%; p<0.001). Similarly, no association with DM2 remission was observed for the BMI before surgery (p=0.343) or for the percentage overweight lost after BS (p=0.440). In patients receiving insulin, high insulin doses (>80U/day) were associated with poorer remission rates according to the national criteria (7.7% vs 46.7%; p=0.023).
DiscussionType 2 diabetes mellitus has traditionally been considered a chronic disease, because fewer than 15% of all patients achieved remission with conventional treatment (lifestyle modifications and drug therapy).13,14 In our study, 65.9% of the patients achieved complete remission of DM2 at one year. This figure is in the upper range of the DM2 remission rates documented in the clinical trials published to date (30–63%).5
The percentage of patients in remission in our sample remained constant at 5 years, though a decrease in this figure was seen in the third year of follow-up. We find no explanation for this observation. A slow but progressive increase was seen in HbA1c (without reaching >6.5%). In concordance with our results, the available data show a decrease in percentage DM2 remission over time (with a reappearance of the disease in 35–50% of all cases over the longer term). However, the median disease-free period after RYGB is 8.3 years,15,16 and most patients subjected to BS maintain substantial improvements in glycemic control for at least 5 years.7
In coincidence with our own observations, a younger age, a shorter time from the onset of DM2, no prior insulin treatment, and better prior metabolic control are consistently associated in the literature with higher DM2 remission rates after BS.8,17,18 The explanation for this is probably that the benefit upon the pancreatic islets of the hormonal changes occurring after the reconstruction of gastrointestinal transit depends on the mass of beta-cells present at the time of BS (the more evolved the disease, the smaller the beta-cell mass and the lesser the probability of DM2 remission). The practical consequence of this should be the avoidance of surgical delays in obese diabetic patients in which BS is indicated.
The third objective of our study was to analyze the correlation between the Spanish national and the American criteria, which proved to be very good. We even found the association between the predictors of BS success and DM2 remission to be greater with the national criteria11 than with the American criteria.12 This suggests that our consensus criteria have at least the same consistency and external validity as those of the ADA. The mentioned criteria also offer the advantage of including a fourth category (“improvement”), which includes patients who have adequate metabolic control even if they are unable to discontinue drug treatment for DM2. This allows for a more exhaustive evaluation of BS success in terms of improved glycemic control.
The main strengths of our study are the large sample size and data compilation consistent with the main clinical trials conducted to date in the “real-life” clinical practice setting. By contrast, the most significant limitations of our study were its retrospective design and the short follow-up time (3.5 years on average), which possibly precluded the detection of more DM relapses. In any case, in the subgroup of patients with 5 years of follow-up, the remission levels remained virtually unchanged. This indicates that BS affords at least 5 years of good metabolic control, with the expected associated benefits in terms of a decrease in micro- and macrovascular complications over the long term. Another limitation of our study is the fact that C peptide was not measured before surgery, this peptide having been shown to be an important marker of DM2 remission after BS.19
In conclusion, our results show BS to be associated with high DM2 remission rates in morbidly obese individuals subjected to surgery at our center, with a very good correlation between the Spanish national and ADA disease remission criteria. A patient age of over 50 years, long-evolving DM2, poorer initial metabolic control (HbA1c≥8%) and prior insulin treatment are indicators of a poorer response to BS in terms of DM2 remission.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Pereyra-García Castro FM, Oliva García JG, García Nuñez MA, García Bray BF, Suarez Llanos JP, Moneva Arce ME, et al. Eficacia en la remisión de la diabetes mellitus tipo 2 en pacientes sometidos a cirugía bariátrica en nuestro medio. Endocrinol Diabetes Nutr. 2019;66:56–61.