Obese patients with lipid discordance (non-HDL cholesterol levels 30mg/dl above the LDL-c value) may have a greater prevalence of carotid atherosclerotic plaque (CAP). Our study objectives were: (1) To assess the prevalence of lipid discordance in a primary prevention population of obese patients; (2) To investigate the association between lipid discordance and presence of CAP.
MethodsObese subjects aged >18 years (BMI≥30kg/m2) with no cardiovascular disease, diabetes, or lipid-lowering treatment from six cardiology centers were included. Lipid discordance was defined when, regardless of the LDL-c level, the non-HDL cholesterol value exceeded the LDL-c value by 30mg/dl. Presence of CAP was identified by ultrasonography. Univariate and multivariate analyses were performed to explore the association between lipid discordance and presence of CAP.
ResultsThe study simple consisted of 325 obese patients (57.2% men; mean age, 52.3 years). Prevalence of lipid discordance was 57.9%. CAP was found in 38.6% of patients, but the proportion was higher in subjects with lipid discordance as compared to those without this lipid pattern (44.4% vs. 30.7%, p=0.01). In both the univariate (OR: 1.80; 95% CI: 1.14–2.87; p=0.01) and the multivariate analysis (OR: 2.07; 95% CI: 1.22–3.54; p=0.007), presence of lipid discordance was associated to an increased probability of CAP.
ConclusionIn these obese patients, lipid discordance was associated to greater prevalence of CAP. Evaluation of obese patients with this strategy could help identify subjects with higher residual cardiovascular risk.
Los pacientes obesos con discordancia lipídica podrían tener una mayor prevalencia de aterosclerosis subclínica. Los objetivos de nuestro trabajo fueron: 1) determinar la prevalencia de discordancia lipídica en una población de pacientes obesos en prevención primaria; 2) investigar la asociación entre la discordancia lipídica y la presencia de placa aterosclerótica carotídea (PAC).
MétodosSe incluyeron sujetos mayores de 18 años obesos (índice de masa corporal ≥30kg/m2) sin enfermedad cardiovascular, diabetes, o tratamiento hipolipemiante, provenientes de 6 centros de cardiología. Se definió «discordancia lipídica» cuando, independientemente del valor de c-LDL, el valor de colesterol no HDL superaba 30mg/dL el valor de c-LDL. Se identificó la presencia de PAC por ultrasonido. Se realizaron análisis uni y multivariados explorando la asociación entre la discordancia lipídica y la presencia de PAC.
ResultadosSe incluyeron 325 pacientes obesos (57,2% hombres, edad media: 52,3 años). La prevalencia de discordancia lipídica fue del 57,9%. Mostraron PAC el 38,6% de los pacientes. Esta proporción fue mayor en los sujetos con discordancia lipídica en comparación con los pacientes sin este patrón lipídico (44,4% vs. 30,7%, p=0,01). En el análisis univariado (OR: 1,80; IC95%: 1,14-2,87; p=0,01) y en el multivariado (OR: 2,07; IC95%: 1,22-3,54; p=0,007), la presencia de discordancia lipídica se asoció con una mayor probabilidad de presentar PAC.
ConclusiónEn pacientes obesos, la discordancia lipídica se asoció con una mayor prevalencia de PAC. Evaluar pacientes obesos con esta estrategia podría identificar a los sujetos con mayor riesgo cardiovascular residual.
Obesity is currently considered a worldwide epidemic.1 Weight increase is associated with other cardiovascular risk factors such as arterial hypertension, dyslipidemia, diabetes, and metabolic syndrome.2 In the general population, a higher body mass index (BMI) is associated with increased cardiovascular morbidity and mortality.3
The lipid profile of obese individuals is usually characterized by high triglyceride levels, low HDL-cholesterol concentrations, and a greater presence of remnant cholesterol and small and dense LDL-cholesterol particles.4 However, not all obese subjects have the metabolic alterations commonly seen in patients of this kind. Thus, it has been postulated that cardiovascular risk in obese patients is not homogeneous.5–7 Although LDL-cholesterol is considered the primary therapeutic target, recent guides recognize non-HDL-cholesterol as a relevant lipid target.8–10 This lipid marker is easy to record and affords greater precision in estimating the total atherogenic particles. A consensus has been reached which defines the non-HDL-cholesterol target as 30mg/dl above the LDL-cholesterol target.
There is evidence that the presence of carotid atherosclerotic plaque (CAP) improves the prediction of cardiovascular events when this information is incorporated into a model constructed with the traditional risk factors.11 Likewise, the prevalence of CAP among obese patients is considerable, and increases with increasing risk scores (based on the risk factors).6
Taking the above into account, we raise the possibility that obese individuals with non-HDL-cholesterol levels 30mg/dl above the LDL-cholesterol levels (lipid discordance) have a greater prevalence of subclinical atheromatosis.
The objectives of the present study were: (1) to determine the prevalence of lipid discordance in a population of obese adults seen in cardiovascular prevention clinics without cardiovascular disease, diabetes or lipid-lowering treatment; and (2) to investigate the association between lipid discordance and the presence of CAP.
Material and methodsA multicenter, descriptive cross-sectional study was made of consecutive samples from cardiovascular prevention clinics in 6 cardiology centers of the Ciudad Autónoma de Buenos Aires and Gran Buenos Aires (Argentina).
The study included individuals over 18 years of age with obesity (BMI≥30kg/m2) who were evaluated in the clinic for the screening of cardiovascular risk or the management of risk factors. The exclusion criteria were: (1) previous cardiovascular disease; (2) a personal history of diabetes mellitus; (3) previous lipid-lowering treatment; (4) hypertriglyceridemia secondary to thyroid gland disorders, renal failure, toxic agents or drugs.
Clinical and laboratory parameters (lipid profile with 12h fasting, including total cholesterol, HDL-cholesterol and triglycerides) were analyzed. The Friedewald formula was used to calculate LDL-cholesterol. The triglyceride/HDL-cholesterol ratio was used as an insulin resistance marker. Remnant cholesterol was calculated from the following formula: (total cholesterol)–(HDL-c)–(LDL-c). The Castelli index was used to calculate the total cholesterol/HDL-cholesterol ratio.
Independently of the LDL-cholesterol level, a patient was taken to present “lipid discordance” when the non-HDL-cholesterol concentration exceeded the LDL-cholesterol level by 30mg/dl.
We calculated the Framingham score for coronary events used in the third report of the expert panel of the National Cholesterol Education Program on the detection, evaluation and treatment of high blood cholesterol in adults (ATP III).12 We likewise estimated the score recommended by the most recent North American guides on cholesterol management (ACC/AHA 2013).13
The carotid arteries were subjected to noninvasive two-dimensional ultrasound exploration. The presence of CAP was defined by the following criteria: (1) abnormal wall thickness (defined as a media-intima thickness of >1.5mm); (2) abnormal structure (protrusion toward the vascular lumen, loss of alignment with the adjacent wall); and (3) abnormal wall echogenicity.
The prevalence of lipid discordance was explored in the different BMI tertiles.
Statistical analysis. Continuous data between two groups were analyzed using the Student t-test in the presence of a normal distribution, or with the Mann–Whitney–Wilcoxon test in the presence of a non-normal distribution. Categorical data were analyzed with the chi-squared test. Continuous variables were reported as the mean±standard deviation (SD), while categorical variables were presented as percentages.
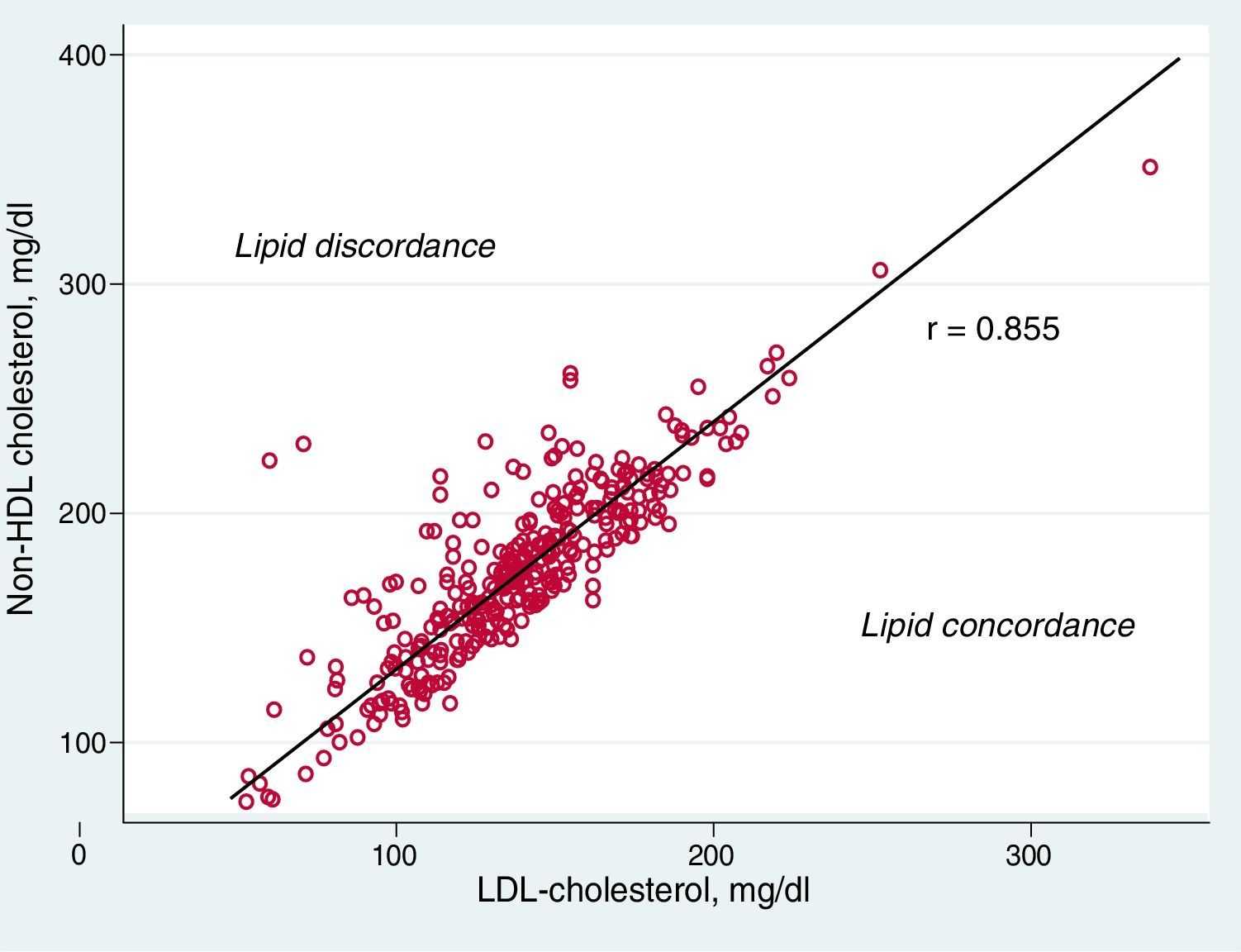
The correlation between LDL-cholesterol and non-HDL-cholesterol was estimated using the Pearson test.
A multiple logistic regression model was developed to explore the association between the lipid discordance pattern and the presence of CAP, those variables being entered that showed p<0.05 in the univariate analysis, as well as those parameters regarded as clinically relevant (age and gender). The strength of the association was expressed by the odds ratio (OR) with a corresponding 95% confidence interval (95%CI). Statistical significance was defined by p<0.05.
Ethical considerations. The study was conducted in compliance with the recommendations for medical research of the Declaration of Helsinki, Good Clinical Practice standards, and the applicable ethical regulations.
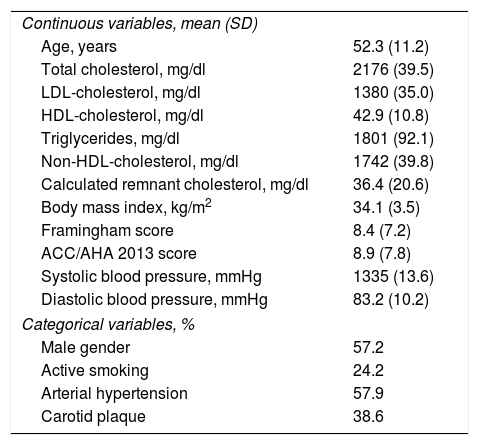
ResultsA total of 325 obese patients were included in the study. Of these, 57.2% were males, and the mean age was 52.3 years. The concentrations (mean±SD) corresponding to total cholesterol, LDL-cholesterol, HDL-cholesterol and triglycerides were 217.6±39.5, 138.0±35, 42.9±10.8 and 180.1±92.1mg/dl, respectively. Table 1 describes the characteristics of the study population.
Characteristics of the study population (No.=325).
| Continuous variables, mean (SD) | |
| Age, years | 52.3 (11.2) |
| Total cholesterol, mg/dl | 2176 (39.5) |
| LDL-cholesterol, mg/dl | 1380 (35.0) |
| HDL-cholesterol, mg/dl | 42.9 (10.8) |
| Triglycerides, mg/dl | 1801 (92.1) |
| Non-HDL-cholesterol, mg/dl | 1742 (39.8) |
| Calculated remnant cholesterol, mg/dl | 36.4 (20.6) |
| Body mass index, kg/m2 | 34.1 (3.5) |
| Framingham score | 8.4 (7.2) |
| ACC/AHA 2013 score | 8.9 (7.8) |
| Systolic blood pressure, mmHg | 1335 (13.6) |
| Diastolic blood pressure, mmHg | 83.2 (10.2) |
| Categorical variables, % | |
| Male gender | 57.2 |
| Active smoking | 24.2 |
| Arterial hypertension | 57.9 |
| Carotid plaque | 38.6 |
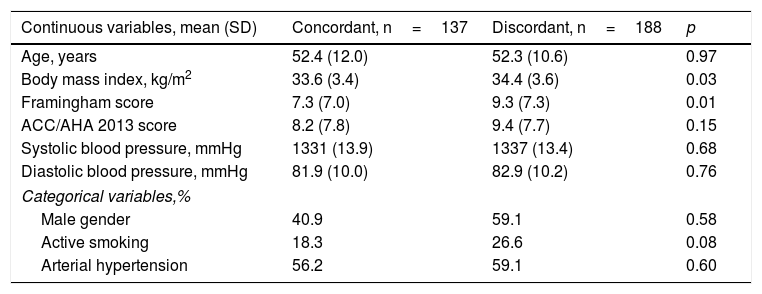
Lipid discordance was observed in 57.9% of the global sample (males 59.1%, females 56.2%). The patients with lipid discordance had a greater BMI (34.4±3.6kg/m2 vs. 33.6±3.4kg/m2; p=0.03) and a higher Framingham score (9.3±7.3% vs. 7.3±7.0%; p=0.01) than the subjects without lipid discordance. There were no significant differences in the other non-lipidic variables analyzed (Table 2).
Characteristics of the study population according to lipid profile (No.=325).
| Continuous variables, mean (SD) | Concordant, n=137 | Discordant, n=188 | p |
|---|---|---|---|
| Age, years | 52.4 (12.0) | 52.3 (10.6) | 0.97 |
| Body mass index, kg/m2 | 33.6 (3.4) | 34.4 (3.6) | 0.03 |
| Framingham score | 7.3 (7.0) | 9.3 (7.3) | 0.01 |
| ACC/AHA 2013 score | 8.2 (7.8) | 9.4 (7.7) | 0.15 |
| Systolic blood pressure, mmHg | 1331 (13.9) | 1337 (13.4) | 0.68 |
| Diastolic blood pressure, mmHg | 81.9 (10.0) | 82.9 (10.2) | 0.76 |
| Categorical variables,% | |||
| Male gender | 40.9 | 59.1 | 0.58 |
| Active smoking | 18.3 | 26.6 | 0.08 |
| Arterial hypertension | 56.2 | 59.1 | 0.60 |
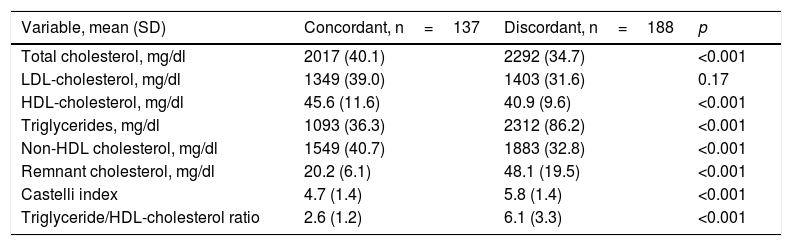
The HDL-cholesterol/triglyceride ratio was significantly higher in the patients with lipid discordance than in those without such a lipid profile (6.1±1.2 vs. 2.6±1.2; p<0.001). Table 3 describes the values of the lipid variables according to concordant or discordant lipid patterns.
Lipid values of the study population according to concordant or discordant profile.
| Variable, mean (SD) | Concordant, n=137 | Discordant, n=188 | p |
|---|---|---|---|
| Total cholesterol, mg/dl | 2017 (40.1) | 2292 (34.7) | <0.001 |
| LDL-cholesterol, mg/dl | 1349 (39.0) | 1403 (31.6) | 0.17 |
| HDL-cholesterol, mg/dl | 45.6 (11.6) | 40.9 (9.6) | <0.001 |
| Triglycerides, mg/dl | 1093 (36.3) | 2312 (86.2) | <0.001 |
| Non-HDL cholesterol, mg/dl | 1549 (40.7) | 1883 (32.8) | <0.001 |
| Remnant cholesterol, mg/dl | 20.2 (6.1) | 48.1 (19.5) | <0.001 |
| Castelli index | 4.7 (1.4) | 5.8 (1.4) | <0.001 |
| Triglyceride/HDL-cholesterol ratio | 2.6 (1.2) | 6.1 (3.3) | <0.001 |
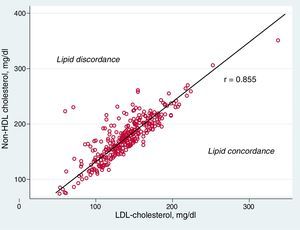
A good correlation was found between LDL-cholesterol and non-HDL-cholesterol (r=0.855). The distribution of LDL-cholesterol and non-HDL-cholesterol in the global population, together with the lipid discordance or concordance categories, are shown in Fig. 1.
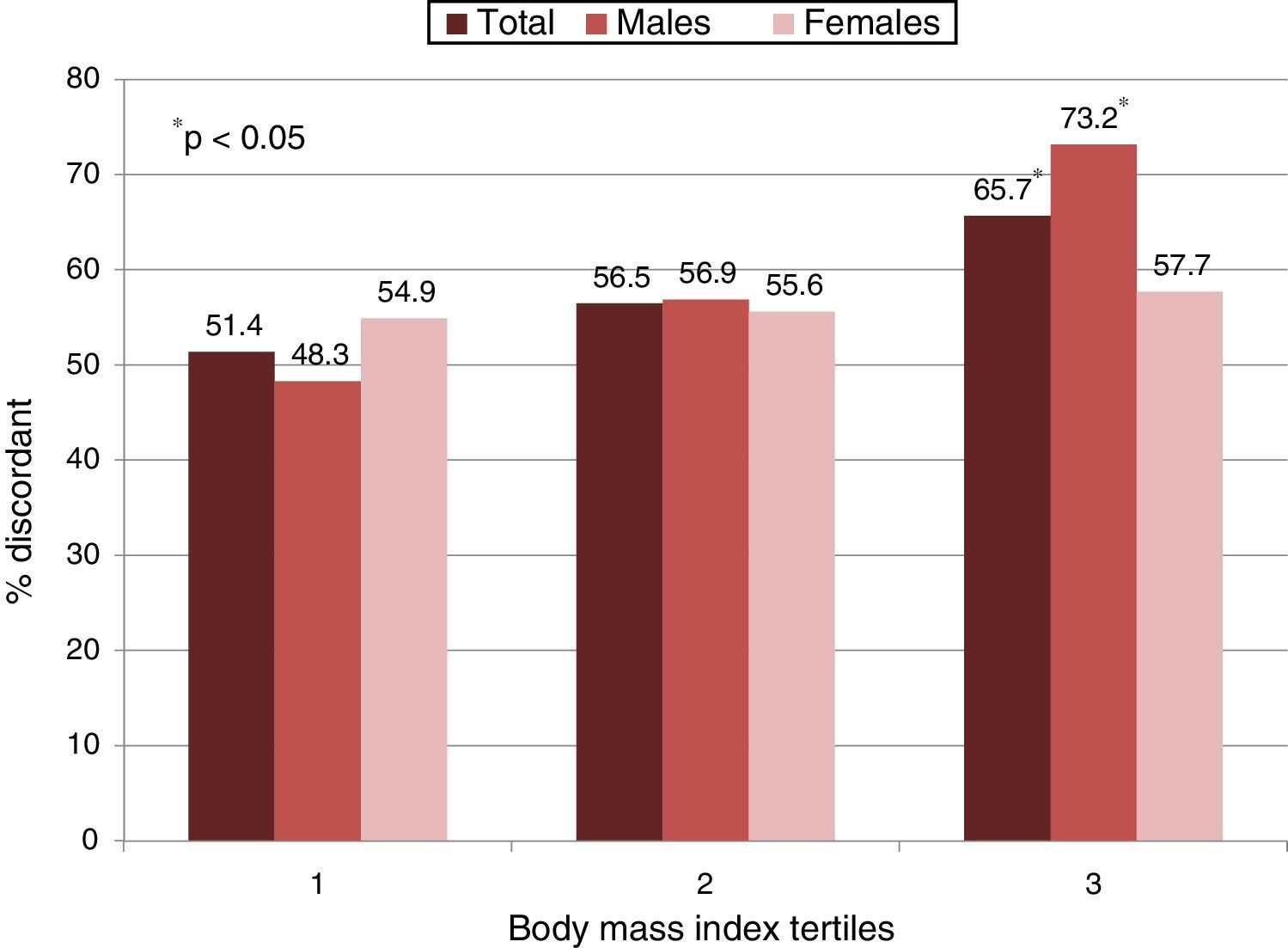
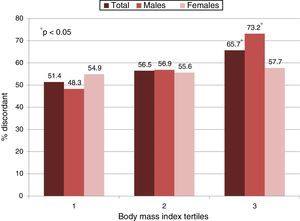
The proportion of patients with lipid discordance was significantly greater in the upper BMI tertile (mean 38.2±2.9kg/m2) than in the lower tertile (mean 30.9±0.6kg/m2), in both the global population and among the males. A statistically non-significant trend was observed in females (Fig. 2).
Carotid atherosclerotic plaque was identified in 38.6% of the patients (males 37.8%, females 39.6%). This proportion was greater among the individuals with lipid discordance than in those without it (44.4% vs. 30.7%; p=0.01).
In the univariate analysis, the presence of lipid discordance was associated with an average 80% greater probability of CAP (OR: 1.80; 95%CI: 1.14–2.87; p=0.01). In the multivariate analysis (adjusted for age, gender, the BMI and the Framingham score), obese patients with lipid discordance doubled the probability of having CAP in the ultrasound study compared with the individuals without CAP (OR: 2.07; 95%CI: 1.22–3.54; p=0.007).
DiscussionThe prevalence of obesity has doubled in the last 35 years in many parts of the world. Two-thirds of all deaths related to obesity are attributable to cardiovascular disease.14
The present study shows the presence of lipid discordance in obese patients in the context of primary prevention to be associated with an increased probability of CAP.
Carotid atherosclerotic plaque is a surrogate of cardiovascular disease, and its presence is associated with all the cardiovascular risk factors.15 The plasma total cholesterol and triglyceride concentrations are independently associated with the presence of CAP.16 Likewise, non-HDL-cholesterol and HDL-cholesterol are related to an increased atherosclerotic “burden”.17 Megias-Rangil et al. showed dyslipidemia to be the main variable associated with carotid intima-media thickening in a group of patients with morbid obesity.18
The analysis of discordance is a technique in which biologically related variables are explored according to groups exhibiting concordance or discordance between their relative distributions.19 In our study “lipid discordance” has been defined on an arbitrary but original basis. The lipid profile was classified as discordant for each patient when the non-HDL-cholesterol concentration exceeded the LDL-cholesterol level by 30mg/dl. The clinical value of this analysis is therefore more closely related to the number of atherogenic particles than to the total cholesterol mass. In a group of primary prevention patients, our group previously demonstrated the association between lipid discordance and remnant cholesterol and the presence of CAP.20 In the present study we specifically examined a group of obese patients, excluding individuals with diabetes and patients receiving lipid-lowering treatment.
Lipid discordance was documented in 57.9% of the subjects. The idea that not all obese individuals present metabolic changes—including atherogenic dyslipidemia—is not new. Up to one-third of the studied obese subjects do not show the metabolic changes commonly seen in obese individuals.21 The term ‘healthy obese’ is used in reference to these subjects and to distinguish them from the larger and more common population of obese individuals, although its true prognostic value is unclear.
Our results indicate that lipid discordance is more prevalent among individuals with higher BMI values. The novel and simplified form of identifying the atherogenic pattern of dyslipidemia in our study coincides with previous studies associating different lipid markers (apolipoprotein B, non-HDL-cholesterol, small and dense particles) to increased body weight.4
Insulin resistance is frequently seen in obese individuals and is characterized by a decrease in insulin biological function, a high plasma concentration of this hormone being needed to maintain carbohydrate, protein and lipid metabolism. The triglyceride/HDL-cholesterol ratio is regarded as a surrogate marker of insulin resistance.22,23 In our study, the triglyceride/HDL-cholesterol ratio was significantly higher in the patients with lipid discordance, thus suggesting a greater presence of insulin resistance in such individuals.
Our data indicate a greater prevalence of CAP in obese subjects with lipid discordance. This association persisted after adjusting for other potential confounding variables. These findings underscore the importance of measuring non-HDL-cholesterol beyond the LDL-cholesterol value, especially in certain populations such as obese individuals. In routine practice, many patients at high cardiovascular risk show a persistent atherogenic dyslipidemic profile despite having reached the recommended LDL-cholesterol target.24 This is clinically relevant, since failure to detect these patients implies that no action will be taken to correct the residual cardiovascular risk.
Our study has some limitations. Firstly, the study design did not allow us to rule out possible bias (mainly selection bias). The obese individuals visiting cardiovascular prevention clinics were not necessarily representative of the general population. Secondly, the waist circumference could not be documented in most of the patients; as a result, the presence of metabolic syndrome according to the classical definition could not be analyzed. On the other hand, we used the Friedewald formula to calculate LDL-cholesterol in our study. This calculation has limits when the triglyceride concentration exceeds 400mg/dl. However, only 3% of the obese subjects in our population showed triglyceride levels above this threshold. Another limitation is the fact that while the classical risk factors (age, gender, arterial hypertension, dyslipidemia, smoking) were taken into consideration in our study, other risk factors were left out of the analysis. Lastly, the triglyceride/HDL-cholesterol ratio was used as an insulin resistance marker, and insulinemia determinations were not available in all cases.
In conclusion, the prevalence of lipid discordance in our population of obese patients was considerable. This simple way to estimate atherogenic dyslipidemia was associated with an increased prevalence of CAP. Since the detection of CAP implies increased cardiovascular risk, the characterization of obese patients from this perspective could allow us to identify obese subjects with a greater residual cardiovascular risk.
Conflicts of interestNone.
Please cite this article as: Masson W, Siniawski D, Lobo M, Molinero G. Discordancia lipídica y placa carotídea en pacientes obesos en prevención primaria. Endocrinol Diabetes Nutr. 2018;65:39–44.