To ascertain the prevalence of Bethesda category III cytologies and their malignancy rate, and to analyze differences in the second cytology, malignancy rate, type of carcinoma, and TNM stage between the cytological atypia (CA) and architectural atypia (AA) groups.
Patients and methodA retrospective study of 973 biopsies. Bethesda category III cytologies were classified as CA when nuclear atypia was seen but they were not diagnostic or suspicious of malignancy, and as AA when smears had few cells but had a predominantly microfollicular pattern and minimal or absent colloid. The cytological and pathological results were correlated.
ResultsThere were 87 (8.9%) Bethesda category III cytologies (34 CC, 53 AA). Second cytologies were performed in 23 patients (16 with CA, 7 with AA), and a benign result was found in 68.7% of CA and 71.4% of the AA group. Sixty-four patients (23 CA, 41 AA) underwent surgery and 15 of these (23.4%) had a malignant disease: 39.1% CA vs 14.6% AA (p=0.029). There was a false negative result in the CA group. The follicular variant of papillary thyroid carcinoma was the most common malignancy (60%). There were no differences in type of carcinoma or TNM stage between CA and AA patients.
ConclusionsThe reported prevalence of Bethesda category III cytologies was as expected. The malignancy rate was significantly higher in the CA group, but there were no differences in the result of the second cytology, type of carcinoma found, or TNM stage. The division of Bethesda category III cytologies is useful to provide a better stratification of the risk of malignancy.
Conocer la prevalencia de citologías de categoría Bethesda III, su tasa de malignidad y analizar si existen diferencias en la segunda citología, tasa de malignidad, tipo de carcinoma y estadio TNM entre los grupos atipia citológica (AC) y atipia arquitectónica (AA).
Pacientes y métodoEstudio retrospectivo de 973 citologías. Las de categoría Bethesda III se agruparon en AC cuando se apreció atipia nuclear pero no diagnóstica o sospechosa de malignidad, y en AA cuando se trató de extensiones con poca celularidad, pero con un patrón predominantemente microfolicular y con coloide mínimo o ausente. Se correlacionaron los resultados citológicos y anatomopatológicos.
ResultadosHallamos 87 (8,9%) citologías de categoría Bethesda III (34 AC, 53 AA). Se realizó una segunda citología en 23 casos (16 AC, 7 AA) con resultado benigno en el 68,7% de los AC y 71,4% de los AA. Fueron intervenidos quirúrgicamente 64 casos (23 AC, 41 AA) y 15 (23,4%) resultaron malignos: 39,1% AC vs 14,6% AA (p=0,029). Hubo un falso negativo en la segunda citología. El carcinoma papilar variante folicular fue el más frecuente (60%). No hubo diferencias entre AC y AA respecto al tipo de neoplasia ni estadio TNM.
ConclusionesNuestra prevalencia de citologías de categoría Bethesda III está dentro de lo recomendado. La tasa de malignidad es significativamente superior en el grupo AC, pero sin diferencias en el resultado de la segunda citología, tipo de carcinoma hallado ni estadio TNM. La división de la categoría Bethesda III es útil para proporcionar una mejor estratificación del riesgo de malignidad.
Category III of the Bethesda classification for the cytological diagnosis of thyroid nodules comprises a heterogeneous group of lesions.1–3 As a result, the distribution of results in each series and the associated malignancy rates reflect the particular characteristics of each center and patient population involved.4–8 It is therefore advisable, if not crucial, for each site to compile, analyze and evaluate the cytological and histopathological results of their patients.4–6,9
In order to clarify the nature of thyroid nodules presenting Bethesda category III cytological features, it is advisable to repeat the cytology study, perform a punch biopsy, conduct a molecular biomarker study or indicate surgery based on the clinical, ultrasound, cytological and molecular data, as well as patient preference.1,3,7,9–11 This recommendation is ambiguous, however, because it has not yet been possible to accurately identify patients with malignant nodules preoperatively among those presenting Bethesda category III cytological criteria. Neither the clinical or immunohistochemical data nor the study of molecular biomarkers have yielded results that are sufficiently discriminatory to allow routine implementation in clinical practice.9,12 Even ultrasound data suggestive of malignancy in non-selected thyroid nodules (microcalcifications, hypoechogenicity, greater height than width and/or irregular margins) are not usually helpful for detecting malignancy in Bethesda category III cases.5,12–14
According to some studies, the division of Bethesda category III into “cytological atypia” (CA) and “architectural atypia” (AA) distinguishes relevant differences in malignancy risk, the latter being significantly higher in the case of CA.5,15–21 In the recent meta-analysis published by Valderrabano et al.,21 the relative risk of malignancy in Bethesda category III nodules with CA was 3.63-fold greater than in the AA group. It was subsequently suggested that the management of these patients should differ depending on whether they belong to the CA or the AA group.2 However, these differences in the malignancy rate have not been confirmed by other authors.5 Furthermore, the 2017 Bethesda consensus3 insists that atypia of undetermined significance (linked to cytological atypia) and follicular proliferation of undetermined significance (linked to architectural atypia) are synonymous terms, and should not be interpreted differently. Therefore, the division of Bethesda category III into groups has not been widely accepted and has not been incorporated into the clinical guides as an independent cancer risk factor.3,10
On the other hand, a malignancy rate that is high (similar to that of other cytological categories in which surgery is recommended) and clearly higher in the CA group compared with the AA group in Bethesda category III patients may have practical implications, such as the notion that a second cytological study and/or the use of molecular biomarkers (both procedures currently advised for all Bethesda category III cases) is only useful in the AA group, since the high malignancy rate associated with CA nodules would cause them to be preferentially referred for surgical removal.9,20
The purpose of this study was to define the prevalence of Bethesda category III thyroid nodules in patients with nodular goiter and the associated malignancy rate, and to determine whether there are differences between the CA and AA groups in terms of the results of second cytology, the malignancy rate, the type of carcinoma found, and the TNM stage.
Material and methodsA retrospective descriptive study of routine clinical practice was carried out, involving the 973 thyroid nodule cytological studies made between April 2011 (which is when the Bethesda classification was introduced in our hospital) and November 2017. Surgery for some of these patients was delayed until April 2018. In order to avoid bias, patients with a history of thyroidectomy due to thyroid cancer were excluded. The study was reviewed and approved by the Research Ethics Committee of the Fundació Assistencial Mútua Terrassa. Informed consent was obtained from all patients.
Puncture-aspiration of thyroid nodules for cytological study was performed guided by palpation from April 2011 to May 2016 (n=658), and under ultrasound guidance with evaluation of the extracted material in situ from May 2016 to November 2017 (n=315). All procedures were performed by the same operator (L.G.P.). The Bethesda III category nodules were classified as AA when differentiation between follicular neoplasia and hypercellular hyperplastic nodules was not possible, as occurs in scantly cellular smear preparations, though presenting a predominantly microfollicular pattern with minimum or no colloid component. On the other hand, the nodules were classified as CA when nuclear atypia were identified but did not prove diagnostic or suggestive of malignancy, as occurs when occasional nuclear clefts or nuclear pseudoinclusions, an abnormal chromatin pattern, or nuclear and cellular overlap are observed.19,20,22
The decision to repeat cytology within 2–3 months, perform clinical and ultrasound monitoring, or perform surgical resection of the lesion was left to the discretion of the patient and the supervising physician. Surgery was indicated in patients with compressive multinodular goiter or in cases where the second cytological result again corresponded to Bethesda category III; cases with suspected follicular neoplasia (Bethesda IV category); cases with suspected malignancy (Bethesda category V); or cases in which a benign lesion was suspected (Bethesda II category) but the ultrasound findings were strongly suggestive of malignancy.10
In patients undergoing surgery, Bethesda category III nodules were correlated to the corresponding histopathological diagnosis. Incidental carcinomas (including microcarcinomas) other than Bethesda category III nodules were analyzed separately. Noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP) was only compiled between March 2017 (which is when the diagnosis of this variant started in our center) and April 2018 (which is when the last patients included in the study were subjected to surgery).
Estimates of the malignancy rate in thyroid nodules are affected by several sources of bias, since not all the nodules are subjected to surgical resection. We therefore determined the conceivable malignancy rate interval. The lower limit estimate was calculated by dividing the number of confirmed malignant nodules by the total number of Bethesda category III nodules. The assumption that all observed (non-operated) nodules were benign is subject to verification bias, and the prevalence of malignancy is therefore underestimated. The upper limit estimate was calculated by dividing the number of confirmed malignant nodules by the number of nodules subjected to surgery. Since nodules selected for surgery may have other clinical features or ultrasound characteristics that increase the suspicion, this number is subject to selection bias, with overestimation of the prevalence of malignancy. We assume that the true prevalence lies somewhere between the lower and upper limit.
Data were collected referring to the patients (age and gender), their cytological group (CA or AA), possible second cytological study and its result according to the Bethesda classification,1 and the histological type of cancer and TNM stage (8th edition)23 at the time of diagnosis (if any).
The statistical analysis reported the mean±standard deviation (SD) for continuous variables, and the number of cases (n) and percentage (%) for qualitative variables. The relationship between qualitative variables was explored using the chi-squared test, with application of the Fisher exact test where indicated. The Student t-test was used to analyze differences in quantitative variables versus qualitative variables involving two groups. Statistical significance was considered for p<0.05.
ResultsOf the 973 thyroid nodule cytological studies made during the study period, 87 (8.9%) corresponded to Bethesda category III (74 women and 13 men, with a mean age of 52.9±14.9 years). Of these cases, 34 were classified as corresponding to CA (39.1%), while 53 corresponded to AA (60.9%).
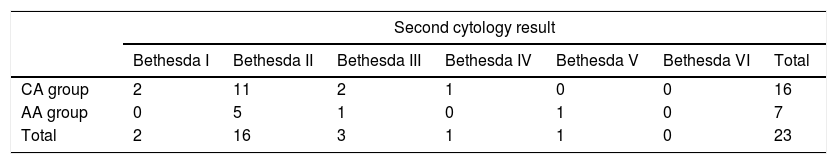
Second cytology was performed in 23 cases (26.4%): 16 in the CA group and 7 in the AA group, and a cytological diagnosis other than Bethesda category I or III was obtained in 75% of the CA cases and in 85.7% of the AA patients (p=ns) (Table 1). In most cases where cytology was repeated, a benign result was obtained in both the CA group (68.7%) and the AA group (71.4%) (p=ns).
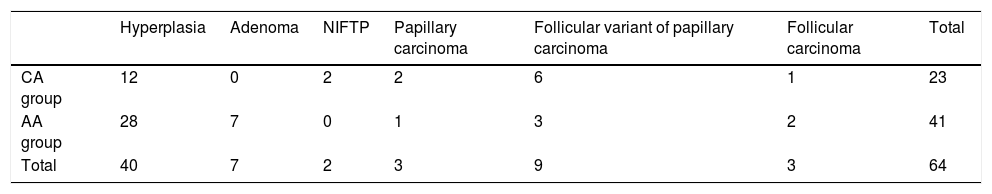
A total of 64 patients underwent surgery (73.6%). The histopathological study established malignancy in 15 cases, representing a malignancy rate of 17.2% for all 87 patients globally and of 23.4% for the 64 patients subjected to surgery. In the CA group the rate ranged from 26.5% to 39.1%, while in the AA group it ranged from 11.3% to 14.6% (p=0.029 for the operated cases and p=0.06 for the operated and non-operated cases, on comparing the CA and AA groups). Table 2 shows the distribution of the cases according to the CA and AA cytological groups. Of note is the predominance of the follicular variant of papillary carcinoma (60% of all cancers).
Results of the histopathological study of the 64 cases subjected to surgery according to cytological group (p=ns).
| Hyperplasia | Adenoma | NIFTP | Papillary carcinoma | Follicular variant of papillary carcinoma | Follicular carcinoma | Total | |
|---|---|---|---|---|---|---|---|
| CA group | 12 | 0 | 2 | 2 | 6 | 1 | 23 |
| AA group | 28 | 7 | 0 | 1 | 3 | 2 | 41 |
| Total | 40 | 7 | 2 | 3 | 9 | 3 | 64 |
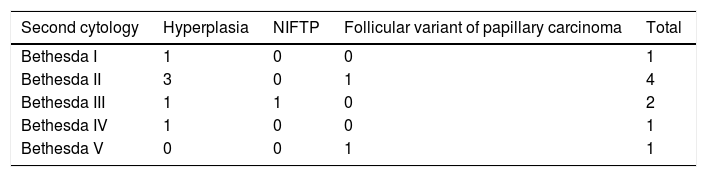
Of the 64 patients subjected to surgery, 9 underwent second cytology (14%) (Table 3). Mention should be made of the presence of a false negative result in the CA group. This was a case with a benign cytological result, but which actually corresponded to the follicular variant of papillary carcinoma.
There were no significant differences in the TNM stage (8th edition) of the malignant tumors according to cytological group (CA group: stage I: 7/9 cases and stage II: 2/9 cases; AA group: stage I: 5/6 cases and stage II: 1/6 cases).
DiscussionThe present study found 8.9% of all the cytological studies to correspond to Bethesda category III, with 39.1% belonging to the CA group and 60.9% to the AA group. The overall malignancy rate was between 17.2% and 23.4%, and was higher in the CA group (26.5–39.1%) than in the AA group (11.3–14.6%). No significant differences were found between the CA and AA groups at second cytology or in the type of carcinoma found after surgery or its TNM stage. Bethesda category III was seen to be useful for stratifying malignancy risk and for establishing a differentiated prognosis in terms of the histological result.
Bethesda category III is heterogeneous, since it includes thyroid gland aspirates that do not suffice to indicate malignancy or neoplasm, but which exhibit atypical nuclear and architectural features that limit their definition as benign lesions.1,3 In most thyroid nodule cytology series the prevalence of Bethesda category III ranges from 6% to 20.5%.5,6,20,24 The 2017 Bethesda consensus3 considers this category to be a last resort, and should not comprise more than 10% of all nodule cytology results. In our study the prevalence of Bethesda category III was within the recommended range.
Originally, the estimated malignancy risk in Bethesda category III was between 5% and 15% for all subjects, and between 20% and 25% for those undergoing surgery.1 Later series reported higher and more variable malignancy rates.25 In patients referred to surgery, the malignancy rate ranged from 14% to 48%, and it was therefore assumed that the rate would be lower in the global Bethesda category III patients, between 5% and 43%.1,2,4–6,10,19–21,25 Such variability may be related to the different representation of the CA cytological group in the Bethesda category III nodes analyzed.21 In our series, the malignancy rate for Bethesda category III was between 17% and 23%, which is a relatively low value, and this agrees with the lesser proportion of cases in the CA group (39%) versus the AA group (61%).
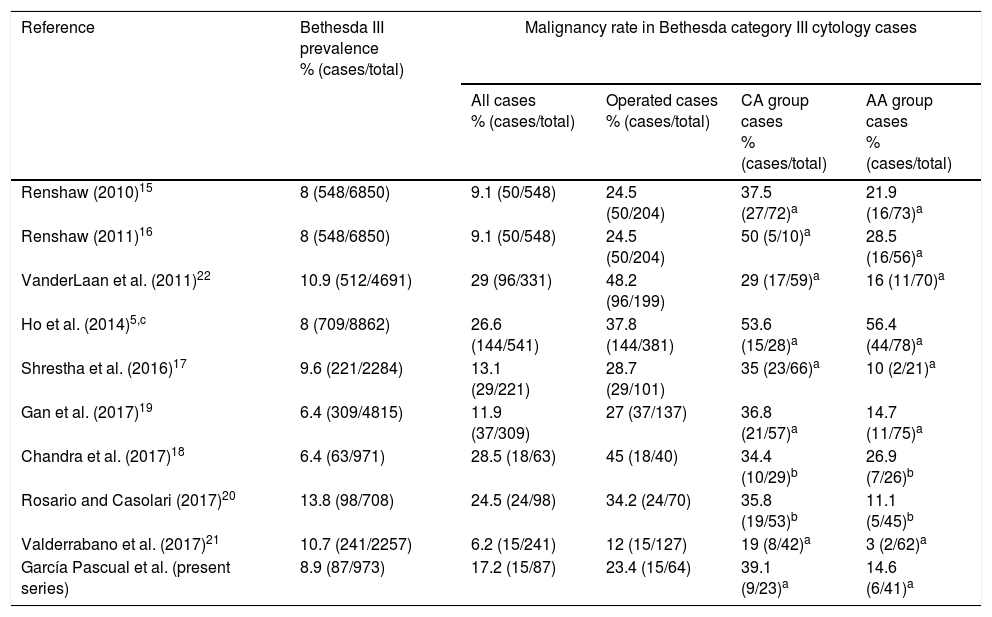
Stratification of Bethesda category III may be useful for reducing heterogeneity and ensuring a more precise prediction of malignancy. Some studies have found clearly higher malignancy rates among Bethesda category III nodules corresponding to the CA group versus the AA group, suggesting that patients should be considered differentially in both cases. Malignancy rates of between 24% and 76% have been reported for nodules with CA cytology, versus between 7% and 32% for nodules with AA.2,15,17,19,20,22,24,26–29 The meta-analysis conducted by Ahn et al.30 comprised 15 studies comparing the malignancy risk between the Bethesda category III groups: the mean malignancy risk in the CA group was found to be 44.5% versus 19.5% in the AA group. The malignancy risk ratio between CA and AA was 2.64, with substantial heterogeneity in both groups. The meta-analysis published by Valderrabano et al.21 comprised 12 studies with 1452 Bethesda category III nodules, of which 47% corresponded to CA. The malignancy risk in nodules corresponding to Bethesda category III and with CA cytological features was 3.63-fold higher than in those without CA. There was a direct correlation between the prevalence of malignancy in Bethesda category III cases of the different centers and the proportion of nodules classified as belonging to the CA group. This may explain the inter-institutional variability in the prevalence of malignancy. However, other studies such as that carried out by Ho et al.,5 with 541 patients presenting Bethesda category III cytology, of which 381 underwent surgery, found no significant differences in the malignancy rate when the cases were classified into these cytological groups (53.6% versus 56.4%). In our study, the surgical cases in the CA group had a malignancy rate approximately 2.6 times higher than the cases in the AA group, a situation considered to be clinically relevant by series reporting similar results (Table 4).
Case series analyzing the malignancy rate of Bethesda category III nodules with CA and AA.
| Reference | Bethesda III prevalence % (cases/total) | Malignancy rate in Bethesda category III cytology cases | |||
|---|---|---|---|---|---|
| All cases % (cases/total) | Operated cases % (cases/total) | CA group cases % (cases/total) | AA group cases % (cases/total) | ||
| Renshaw (2010)15 | 8 (548/6850) | 9.1 (50/548) | 24.5 (50/204) | 37.5 (27/72)a | 21.9 (16/73)a |
| Renshaw (2011)16 | 8 (548/6850) | 9.1 (50/548) | 24.5 (50/204) | 50 (5/10)a | 28.5 (16/56)a |
| VanderLaan et al. (2011)22 | 10.9 (512/4691) | 29 (96/331) | 48.2 (96/199) | 29 (17/59)a | 16 (11/70)a |
| Ho et al. (2014)5,c | 8 (709/8862) | 26.6 (144/541) | 37.8 (144/381) | 53.6 (15/28)a | 56.4 (44/78)a |
| Shrestha et al. (2016)17 | 9.6 (221/2284) | 13.1 (29/221) | 28.7 (29/101) | 35 (23/66)a | 10 (2/21)a |
| Gan et al. (2017)19 | 6.4 (309/4815) | 11.9 (37/309) | 27 (37/137) | 36.8 (21/57)a | 14.7 (11/75)a |
| Chandra et al. (2017)18 | 6.4 (63/971) | 28.5 (18/63) | 45 (18/40) | 34.4 (10/29)b | 26.9 (7/26)b |
| Rosario and Casolari (2017)20 | 13.8 (98/708) | 24.5 (24/98) | 34.2 (24/70) | 35.8 (19/53)b | 11.1 (5/45)b |
| Valderrabano et al. (2017)21 | 10.7 (241/2257) | 6.2 (15/241) | 12 (15/127) | 19 (8/42)a | 3 (2/62)a |
| García Pascual et al. (present series) | 8.9 (87/973) | 17.2 (15/87) | 23.4 (15/64) | 39.1 (9/23)a | 14.6 (6/41)a |
Second cytology of Bethesda category III nodules in most cases resulted in a cytological diagnosis other than Bethesda category I or III (from 55% to 80%), and a benign result (Bethesda category II) was found in approximately 60% of these cases. The latter result in turn may be somewhat more common in the AA group than in CA nodules.19 This explains the few patients subjected to surgery after second cytology. In our study, cytology was repeated in only a few cases (26.4%), because most of the patients were referred to surgery, in the same way as in other series reflecting standard practice.5,6 Nevertheless, our results agree with the above profile, since second cytology yielded a diagnosis other than Bethesda category I or III in 78.2% of the cases, with 69.5% of these nodules being benign, though without significant differences between the CA and AA groups. We only recorded one false negative cytological result, belonging to the CA group. However, due to the small number of patients with benign second cytology findings subjected to surgery (4 cases), no conclusions should be drawn from this finding.
Although the benign lesion rate after second cytology was high in our study in both the CA and AA groups, the fact that there was a high malignancy rate in the CA group (of a magnitude similar to that reported in Bethesda category IV, and considered sufficient to warrant surgery),1,3 does not permit us to conclude that second cytology is appropriate in Bethesda category III cases presenting CA cytological features. By contrast, the malignancy rate in the AA group was even lower than that reported by the Bethesda consensus document for Bethesda category III cases,1,3 where there is no such explicit recommendation for surgery, and given the high percentage of benign lesions identified at second cytology in this group (71.4%), we agree with other authors in reserving second cytology for Bethesda category III cases presenting AA cytological features.19
As in our own study, where the most common malignancy among Bethesda category III nodules was the follicular variant of papillary carcinoma (with a prevalence of 60%), most studies that analyze these nodules report an important presence of this neoplasm, albeit with a heterogeneous prevalence concordant with the type of lesion involved (Valderrabano et al.21: 54%; Walts et al.31: 42%; Chandra et al.18: 44%; Gan et al.19: 20%, of which 23.8% corresponded to CA and 11.1% to AA; VanderLaan et al.22: 76%; Rosario et al.20: 34.5%, of which 27.2% corresponded to CA and 57.1% to AA). Before 2017, considering noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP) the follicular variant of papillary carcinoma may have contributed to this high prevalence. On extrapolating our results from the period between March 2017 and April 2018 to the total series, we could have identified 5 cases of NIFTP. As a result, the prevalence of the follicular variant of papillary carcinoma would have decreased to 50%. No studies have reported differences in terms of tumor TNM stage between the CA and AA groups, coinciding with the observations of our own series.
There are some limitations to our study. Firstly, this was a retrospective trial with a relatively small number of cases, a fact that may have influenced our failure to detect statistically significant differences in the comparison of variables. Secondly, inter-observer differences and intra-observer variability in the cytological or histopathological diagnoses were not specifically evaluated. Nevertheless, all the samples were interpreted by experienced pathologists from the same department.
The Bethesda category III diagnostic category, as currently defined, is heterogeneous in relation to the inclusion criteria and the estimated malignancy risk for different lesions. Our study supports the notion that the CA group has a significantly higher malignancy risk than the AA group. Although the practice of using Bethesda category III diagnostic classifiers is not recommended by the Bethesda consensus, our results support their application in groups for the purpose of affording a better stratification of malignancy risk and improved clinical management of patients with these aspirate findings.
AuthorshipEach author has materially contributed to the investigation and preparation of the manuscript. Specifically:
- -
Luis García Pascual: study conception and design, data acquisition and processing, interpretation of the results, drafting of the manuscript and approval of the final version.
- -
Maria Lluïsa Suralles: data acquisition and analysis, critical review of the draft and approval of the final version.
- -
Xavier Morluis: data acquisition and analysis, critical review of the draft and approval of the final version.
- -
Laia Garcia Cano: data acquisition and analysis, critical review of the draft and approval of the final version.
- -
Clarisa González Mínguez: data acquisition and analysis, critical review of the draft and approval of the final version.
None.
Please cite this article as: García Pascual L, Surralles ML, Morlius X, Garcia Cano L, González Mínguez C. Prevalencia y malignidad asociada de las citologías de categoría Bethesda III de nódulos tiroideos según el grupo «atipia citológica» o «atipia arquitectónica». Endocrinol Diabetes Nutr. 2018;65:577–583.