To determine the clinical-histological data associated comorbidities and the use of health resources of elderly patients with thyroid cancer.
MethodsAn observational, retrospective study was carried out using data from the electronic medical record (EMR) of the Hospital Universitario Puerta de Hierro Majadahonda (Madrid, Spain). The information was extracted using artificial intelligence techniques and analysed using the Savana Manager 3.0 software. We differentiated between younger people (0–59 years) and older people (60 or more years) and, within this latter group, between people of advanced age (60–74 years) and elderly people (75 or more years).
ResultsOf a total of 509,517 patients, 1781 (0.35%) were diagnosed with thyroid cancer. Compared to younger patients, older patients presented a lower proportion of papillary carcinoma (64.2% vs. 75.3%) as well as a higher proportion of follicular carcinoma (9.3% vs. 5.0%) and other histological types (26.5% vs. 19.7%; p < 0.001). Young people with thyroid cancer exhibited prevalences of risk factors and most of the cardiovascular diseases studied significantly higher than those found in the general population. Elderly patients, compared with those of advanced age, showed greater comorbidity. However, a trend towards a lower consumption of healthcare resources was observed when elderly patients were compared with those of advanced age.
ConclusionThe clinical characteristics, comorbidities and consumption of health resources of patients with thyroid cancer vary markedly with age. Elderly patients are characterized by a high burden of comorbidities that is not accompanied by a notable increase in their consumption of health resources.
Caracterizar los datos clínico-histológicos, comorbilidades asociadas y consumo de recursos sanitarios de los pacientes mayores con cáncer de tiroides.
MétodosEstudio observacional, retrospectivo, empleando datos de la historia clínica electrónica (HCE) del Hospital Universitario Puerta de Hierro Majadahonda. La información se extrajo mediante técnicas de inteligencia artificial y se analizó mediante el software Savana Manager 3.0. Se diferenció entre jóvenes (0–59 años) y mayores (60 o más años) y, dentro de estos, entre personas de edad avanzada (60 a 74 años) y ancianos (75 o más años).
ResultadosDe un total de 509.517 pacientes se encontraron 1.781 (0,35%) con el diagnóstico de cáncer de tiroides. Los pacientes mayores presentaron, con respecto a los jóvenes, una menor proporción de carcinoma papilar (64,2 vs 75,3%) y una mayor proporción de carcinoma folicular (9,3 vs 5,0%) y otros tipos histológicos (26,5 vs 19,7%; p < 0,001). Los jóvenes con cáncer de tiroides presentaron prevalencias significativamente superiores a las halladas en la población general de los factores de riesgo y la mayoría de las enfermedades cardiovasculares estudiadas. Los ancianos, en comparación con los de edad avanzada, mostraron una mayor comorbilidad. Sin embargo, se observó una tendencia a un menor consumo de recursos sanitarios cuando se compararon ancianos con personas de edad avanzada.
ConclusiónLas características clínicas, las comorbilidades y el consumo de recursos sanitarios de los pacientes con cáncer de tiroides varían notablemente con la edad. Los pacientes ancianos se caracterizan por una gran carga de comorbilidad no acompañada de un incremento destacable de recursos sanitarios.
Thyroid cancer is the most common endocrine malignancy. Most of these tumours are differentiated thyroid carcinomas (DTCs), the main varieties of which are papillary thyroid carcinoma (PTC) and follicular thyroid carcinoma (FTC). The incidence of DTC has increased in recent years in all countries, partly due to greater use of diagnostic methods, such as ultrasound and cytology.1 The onset of most DTCs is in middle age, although 2.5%–12% of all DTCs occur in patients older than 65 years.2,3
Some studies have shown that the incidence of DTC increases with age.4 Others have shown that DTCs in the elderly tend to be larger and to present more frequently with aggressive histological types, extrathyroid disease and distant metastases2,3,5–8 and, consequently, a worse prognosis,9 which translates into a higher recurrence rate10 and lower long-term survival.11
At the present time, the introduction of artificial intelligence and big data methods of analysis are changing the way knowledge is generated, and medical science is no stranger to these changes.12 In addition, the introduction of the electronic health record (EHR) in most hospitals has led to the accumulation of huge amounts of information in electronic format that make it possible to extract data through the appropriate techniques that would be impossible to obtain manually.13 Thus, the EHR has become the primary source of big data in the healthcare sector. Our objective in this study was to use these novel big data tools to characterize the clinical-histological data, associated comorbidities, chronic complications of treatment and consumption of healthcare resources of elderly patients with thyroid cancer diagnosed at our centre, as well as to analyse any differences according to age, with special attention on late elderly patients.
Material and methodsStudy designAn observational, retrospective, non-interventional study was conducted using the data found in the EHR of the Hospital Universitario Puerta de Hierro Majadahonda (HUPHM). The study comprised clinical data collected between 1 January 2008 and 31 December 2018 and included a total of 509,517 patients. These data came from documents generated on inpatient wards, in the Accident and Emergency department and in outpatient consultations. In view of the known peculiarities of thyroid cancer in elderly people, this study focused on comparing data of elderly people (60 years or older) to those of younger people (under 60 years). Furthermore, within the group of elderly patients, the study particularly focused on analysing the differences between the early elderly (60–74 years old) and the late elderly (75 years or older). For the definition of the study groups, we have followed the WHO criteria, which considers people between 60 and 74 years old as early elderly and those between 75 and 90 as old, or late elderly.14
Since artificial intelligence allows a large amount of information to be obtained from the included patients, relevant data were extracted on the clinical and histological characteristics of patients with thyroid cancer, as well as on chronic complications of treatment (hypoparathyroidism, dysphonia), cardiovascular risk factors (hypertension, dyslipidaemia, diabetes, smoking, obesity), cardiovascular diseases (cerebrovascular accident, ischaemic heart disease, peripheral vascular disease), thromboembolic diseases (deep vein thrombosis, pulmonary thromboembolism) and consumption of healthcare resources (Accident and Emergency department visits, computed tomography [CT], positron emission tomography [PET], oral anti-angiogenic agents [OAs]). The study was approved by the HUPHM Independent Ethics Committee (Code PI 114/21).
Extracting information from the EHRBy means of artificial intelligence techniques and, in particular, natural language processing, the information was extracted from the EHR and analysed using the Savana Manager software, v.3.0. Savana Manager is software that interprets and uses the clinical information found in the EHR, converting the data generated in the hospital, including the information contained in the free text, into structured and reusable data for research purposes. Regarding the variables included in the study, the potential number of variables included was limited to the information contained in EHRs during the study period.
Evaluation of the informationThe first phase for building the database visible through Savana Manager was data acquisition. In compliance with the General Data Protection Regulation, this acquisition was the responsibility of the HUPHM IT Department, which worked with Savana technical staff to pseudonymise the data and transfer them to Savana. The data were integrated into an aggregate database to be processed with EHRead® technology. This technology includes natural language processing techniques to extract information from the free text, recognising clinical variables of interest, denials and temporality, among other expressions, and enables a synthetic database of patients to be built. Savana terminology is based on SNOMED CT and includes over 400,000 medical concepts, acronyms and laboratory parameters. Terminological entities detected in EHRs were subsequently classified according to sections (e.g. demographics, medical history, medications, diagnoses, etc.). Finally, the HUPHM authors validated the results of the tool and the performance of the technology.
This evaluation was intended to verify the validity of the EHRead® technology in the identification of the records that mentioned thyroid cancer and related variables. A set of 494 randomly-selected documents were manually verified that guaranteed the reliability of the manual notation/review and constituted the gold standard. Savana's performance was calculated using this gold standard evaluation resource created by the experts, i.e. Savana's accuracy in identifying records in which the disease in question and related variables were detected was measured against the gold standard. The performance was calculated by the standard metrics of precision (P), recall (R) and the F-score, which is the harmonic mean of the previous two.15
Precision indicated the reliability of the information retrieved by the system and was calculated as P = tp/(tp + fp). Recall, an indicator of how much information the system retrieves, was calculated as R = tp/(tp + fn). The F-score was calculated as F = 2 × precision × recall/(precision + recall). This parameter offered an indicator of the overall performance of information retrieval.
In all cases, true positives (tp) were the sum of correctly identified records, false negatives (fn) were the sum of unidentified records, and false positives (fp) were the sum of incorrectly retrieved records.16
The linguistic evaluation of the thyroid cancer variable yielded a precision, a recall and an F-measure of 1.00 for the three metrics mentioned. This indicated that thyroid cancer diagnoses were accurately detected in the study population. The rest of the noted variables (hypertension, dyslipidaemia, diabetes, smoking, obesity, cerebrovascular accident, ischaemic heart disease, deep vein thrombosis, hypoparathyroidism, dysphonia, CT, PET and OAs), except one (peripheral vascular disease), had an F-score greater than 0.75 (Appendix B Supplementary material, Table S1).
Statistical analysisThe statistical approach to the data included a descriptive analysis of all the variables evaluated, in which the qualitative variables are expressed as absolute frequencies and percentages. To measure the association and compare proportions between qualitative variables, the chi-square test (χ2) was used. In all cases, differences with a comparison test-associated p value less than 0.05 were considered significant.
ResultsStudy populationOf the 509,517 subjects registered in the Savana tool, 53.56% were women and 48.91% were men. In total, 2.47% of the population was classified at some point during their clinical course as male or female, probably due to administrative errors. The mean age of the subjects was 41 years (95% confidence interval: 40.89–41.02). There were 394,282 young people (from 0 to 59 years old) and 115,235 elderly people (60 years of age or older). In this last group there were 59,876 early elderly people (60–74 years old) and 55,359 late elderly (75 years of age or over).
Patients with thyroid cancerA total of 1,781 patients with thyroid cancer (0.35% of the total population) were found. There were 1,233 patients in the young group (0.31%) and 548 patients in the elderly group (0.48%; p < 0.001 vs young). In the elderly group, the proportion of patients with thyroid cancer in the late elderly subgroup (186 [0.34%]) was significantly lower than that observed in the early elderly subgroup (362 [0.60%]; p < 0.001).
The clinical characteristics of the patients with thyroid cancer classified by age groups are summarised in Table 1. Compared to the younger patients, the elderly patients exhibited a lower proportion of PTC and a higher proportion of FTC and other histotypes. They also had lower proportions of family history of thyroid cancer and hypoparathyroidism. We found no significant differences in any of the characteristics analysed when comparing the late elderly with the early elderly.
Histological and clinical characteristics of the patients with thyroid cancer studied and distribution by age group.
| All (n = 1781) | Age (broad groups) | Age groups in elderly patients | |||||
|---|---|---|---|---|---|---|---|
| 0–59 years (n = 1233) | 60 years or older (n = 548) | p | 60–74 years old (n = 362) | 75 years or older (n = 186) | p | ||
| Female | 1120 (63.9) | 768 (62.3) | 352 (64.2) | 0.738 | 231 (63.8) | 121 (65.0) | 0.774 |
| Family history of thyroid cancer | 177 (9.9) | 142 (11.5) | 35 (6.4) | <0.001 | 22 (6.1) | 13 (7.0) | 0.679 |
| Thyroid dysfunction prior to cancer | 86 (4.8) | 53 (4.3) | 33 (6.0) | 0.117 | 19 (5.2) | 14 (7.5) | 0.288 |
| Radiotherapy in childhood | 6 (0.3) | 6 (0.5) | 0 (0) | 0.102 | 0 (0) | 0 (0) | – |
| Histology | <0.001 | 0.481 | |||||
| Papillary | 1280 (71.9) | 928 (75.3) | 352 (64.2) | 237 (65.5) | 115 (61.8) | ||
| Follicular | 113 (6.3) | 62 (5.0) | 51 (9.3) | 30 (8.3) | 21 (11.3) | ||
| Other | 388 (21.8) | 243 (19.7) | 145 (26.5) | 95 (26.2) | 50 (26.9) | ||
| Hypoparathyroidism | 279 (15.67) | 219 (17.76) | 60 (10.95) | <0.001 | 43 (11.88) | 17 (9.14) | 0.331 |
| Dysphonia | 156 (8.76) | 104 (8.43) | 52 (9.49) | 0.468 | 33 (9.12) | 19 (10.22) | 0.678 |
Data represent the number and, in parentheses, the percentage of each group or subgroup.
Table 2 compares the prevalence of cardiovascular risk factors and disease in patients with and without thyroid cancer. Patients with thyroid cancer had significantly higher prevalences than those in the control group for all cardiovascular risk factors studied. The same findings were observed when analysing cardiovascular diseases, with the exception of cerebrovascular accident.
Cardiovascular risk factors and diseases registered in patients with and without thyroid cancer and their distribution by broad age groups.
| All patients | Age: 0–59 years old | Age: 60 years old or over | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Thyroid cancer | Thyroid cancer | Thyroid cancer | |||||||
| Present (n = 1781) | Absent (n = 507,736) | p | Present (n = 1233) | Absent (n = 393,049) | p | Present (n = 548) | Absent (n = 114,687) | p | |
| Cardiovascular risk factors | |||||||||
| Arterial hypertension | 920 (55.66) | 211,156 (41.59) | <0.001 | 464 (37.63) | 117,215 (29.82) | <0.001 | 456 (83.21) | 93,941 (81.91) | 0.430 |
| Dyslipidaemia | 442 (24.82) | 60,209 (11.86) | <0.001 | 218 (17.68) | 24,832 (6.32) | <0.001 | 224 (40.88) | 35,377 (30.85) | <0.001 |
| Diabetes | 259 (14.54) | 41,632 (8.20) | <0.001 | 104 (8.43) | 16,016 (4.07) | <0.001 | 155 (28.28) | 25,616 (22.33) | <0.001 |
| Smoking | 135 (7.58) | 27,772 (5.47) | <0.001 | 91 (7.38) | 21,283 (5.41) | 0.002 | 44 (8.03) | 6489 (5.66) | 0.017 |
| Obesity | 94 (5.28) | 12,712 (2.50) | <0.001 | 43 (3.49) | 6255 (1.91) | <0.001 | 51 (9.31) | 6457 (5.63) | <0.001 |
| Cardiovascular disease | |||||||||
| Cerebrovascular accident | 44 (2.47) | 12,297 (2.42) | 0.894 | 8 (0.65) | 1934 (0.49) | 0.432 | 36 (6.57) | 10,363 (9.04) | 0.044 |
| Ischaemic heart disease | 133 (7.47) | 24,242 (4.77) | <0.001 | 42 (3.41) | 6721 (1.71) | <0.001 | 91 (16.61) | 17,521 (15.28) | 0.385 |
| Peripheral vascular disease | 167 (9.38) | 25,305 (4.98) | <0.001 | 62 (5.03) | 6844 (1.74) | <0.001 | 105 (19.16) | 18,461 (16.10) | 0.056 |
| Thromboembolic disease | |||||||||
| Deep vein thrombosis | 39 (2.19) | 5252 (1.03) | <0.001 | 13 (1.05) | 1731 (0.44) | 0.001 | 26 (4.74) | 3521 (3.07) | 0.024 |
| Pulmonary thromboembolism | 28 (1.58) | 4343 (0.85) | 0.001 | 9 (0.73) | 1304 (0.33) | 0.015 | 19 (3.47) | 3039 (2.64) | 0.235 |
Data represent the number and, in parentheses, the percentage of each group or subgroup.
Similar results were found when analysing the group of young patients. However, elderly people with thyroid cancer showed a higher prevalence of dyslipidaemia, diabetes, smoking, and obesity, but not hypertension. In addition, they had a lower frequency of cerebrovascular accident, a higher frequency of deep vein thrombosis and the same frequency of the rest of the diseases analysed compared to people without thyroid cancer (Table 2).
Although early elderly people with thyroid cancer showed a higher frequency of dyslipidaemia, diabetes (p < 0.001) and obesity (p = 0.003), the prevalences for cardiovascular and thromboembolic diseases were the same as those found in the control group (Table 3). The late elderly patients with thyroid cancer only had a higher frequency of dyslipidaemia (p = 0.001) compared to the non-thyroid cancer population of their age. However, this subgroup showed higher rates of ischaemic heart disease (p = 0.014), peripheral vascular disease (p = 0.009) and deep vein thrombosis (p = 0.005) (Table 3).
Cardiovascular risk factors and diseases registered in patients with and without thyroid cancer in the age groups 60 to 74 years old and 75 years old or over.
| Age: 60–74 years old | Age: 75 years old or over | |||||
|---|---|---|---|---|---|---|
| Thyroid cancer | Thyroid cancer | |||||
| Present (n = 362) | Absent (n = 59,514) | p | Present (n = 186) | Absent (n = 55,173) | p | |
| Cardiovascular risk factors | ||||||
| Arterial hypertension | 294 (81.21) | 45,928 (77.17) | 0.068 | 162 (87.10) | 48,013 (87.02) | 0.976 |
| Dyslipidaemia | 144 (39.78) | 17,802 (29.91) | <0.001 | 80 (43.01) | 17,575 (31.85) | 0.001 |
| Diabetes | 101 (27.90) | 11,535 (19.38) | <0.001 | 54 (29.03) | 14,081 (25.52) | 0.273 |
| Smoking | 35 (9.67) | 4717 (7.93) | 0.221 | 9 (4.84) | 1772 (3.71) | 0.209 |
| Obesity | 36 (9.94) | 3644 (6.12) | 0.003 | 15 (8.06) | 2813 (5.10) | 0.067 |
| Cardiovascular disease | ||||||
| Cerebrovascular accident | 17 (4.70) | 3090 (5.19) | 0.672 | 19 (10.22) | 7273 (13.18) | 0.232 |
| Ischaemic heart disease | 46 (12.70) | 7941 (13.34) | 0.723 | 45 (24.19) | 9580 (17.36) | 0.014 |
| Peripheral vascular disease | 51 (14.09) | 6776 (11.39) | 0.107 | 54 (29.03) | 11,685 (21.18) | 0.009 |
| Thromboembolic disease | ||||||
| Deep vein thrombosis | 11 (3.04) | 1298 (2.18) | 0.266 | 15 (8.06) | 2223 (4.03) | 0.005 |
| Pulmonary thromboembolism | 10 (2.76) | 1084 (1.82) | 0.183 | 9 (4.84) | 1955 (3.54) | 0.340 |
Data represent the number and, in parentheses, the percentage of each group or subgroup.
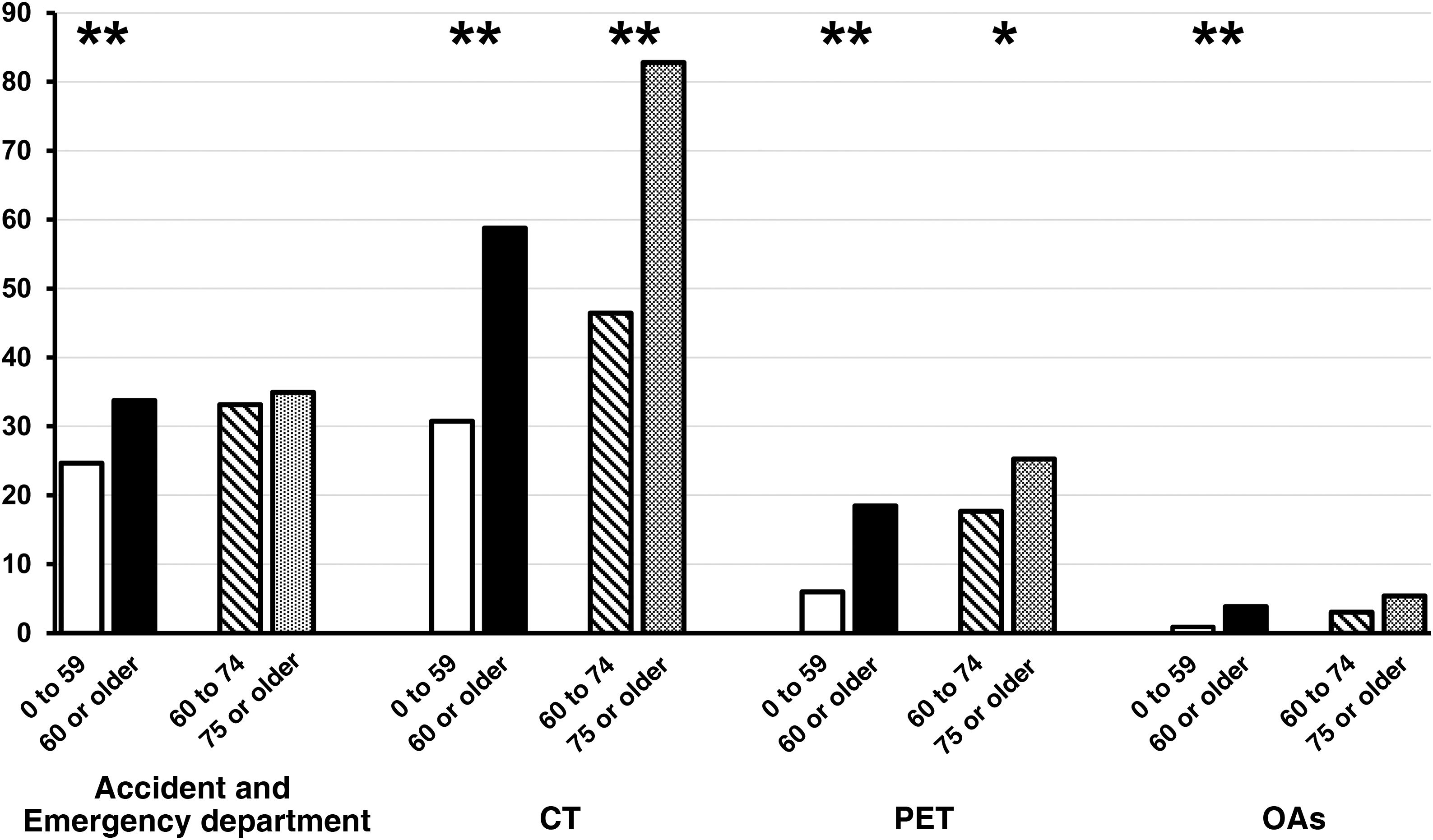
The consumption of healthcare resources by patients with thyroid cancer was analysed according to age and the presence or absence of a second neoplasm. When young patients were compared with elderly patients, it was observed that the latter showed a significantly (p < 0.001) higher consumption of the four healthcare resources studied (Fig. 1). However, when the late elderly were compared with the early elderly, it was found that the late elderly were only higher users of CT (p < 0.001) and PET (p < 0.05), but not Accident and Emergency department visits or OAs (Fig. 1).
Comparison of thyroid cancer patients' healthcare resource consumption between young (0 to 59 years old; white columns) and elderly patients (60 years old or over; black columns); and between early elderly (60 to 74 years old; striped columns) and late elderly patients (75 years old or over; grey columns). The columns represent the percentage of patients who have used each of the resources that are specified on the x-axis.
CT: computerised axial tomography; OAs: oral anti-angiogenics; PET: positron emission tomography.
*p < 0.05; **p < 0.001.
The number of Accident and Emergency department visits, CT, PET and OAs was significantly lower in patients with thyroid cancer who did not have a second neoplasm compared to those with another tumour (p < 0.001 for all areas of resource consumption). This higher proportion of resource consumption was similar when the young and elderly age groups were independently analysed (Table 4).
Consumption of healthcare resources in patients with thyroid cancer classified according to the presence or absence of a second neoplasm.
| All patients | Age: 0–59 years old | Age: 60 years old or over | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Second neoplasm | Second neoplasm | Second neoplasm | |||||||
| Present (n = 250) | Absent (n = 1531) | p | Present (n = 93) | Absent (n = 1140) | p | Present (n = 157) | Absent (n = 391) | p | |
| Accident and emergency department visit | 208 (83.20) | 281 (18.35) | <0.001 | 86 (92.47) | 218 (19.12) | <0.001 | 122 (77.71) | 63 (16.11) | <0.001 |
| CT | 194 (77.60) | 507 (33.12) | <0.001 | 64 (68.82) | 315 (27.63) | <0.001 | 120 (76.43) | 202 (51.66) | <0.001 |
| PET | 81 (32.4) | 94 (6.14) | <0.001 | 30 (32.26) | 44 (3.86) | <0.001 | 51 (32.48) | 50 (12.79) | <0.001 |
| Oral anti-angiogenics | 15 (6.00) | 17 (1.11) | <0.001 | 4 (4.30) | 7 (0.61) | 0.002 | 11 (7.01) | 10 (2.56) | 0.014 |
Data represent the number and, in parentheses, the percentage of each group or subgroup.
CT: computerised axial tomography; PET: positron emission tomography.
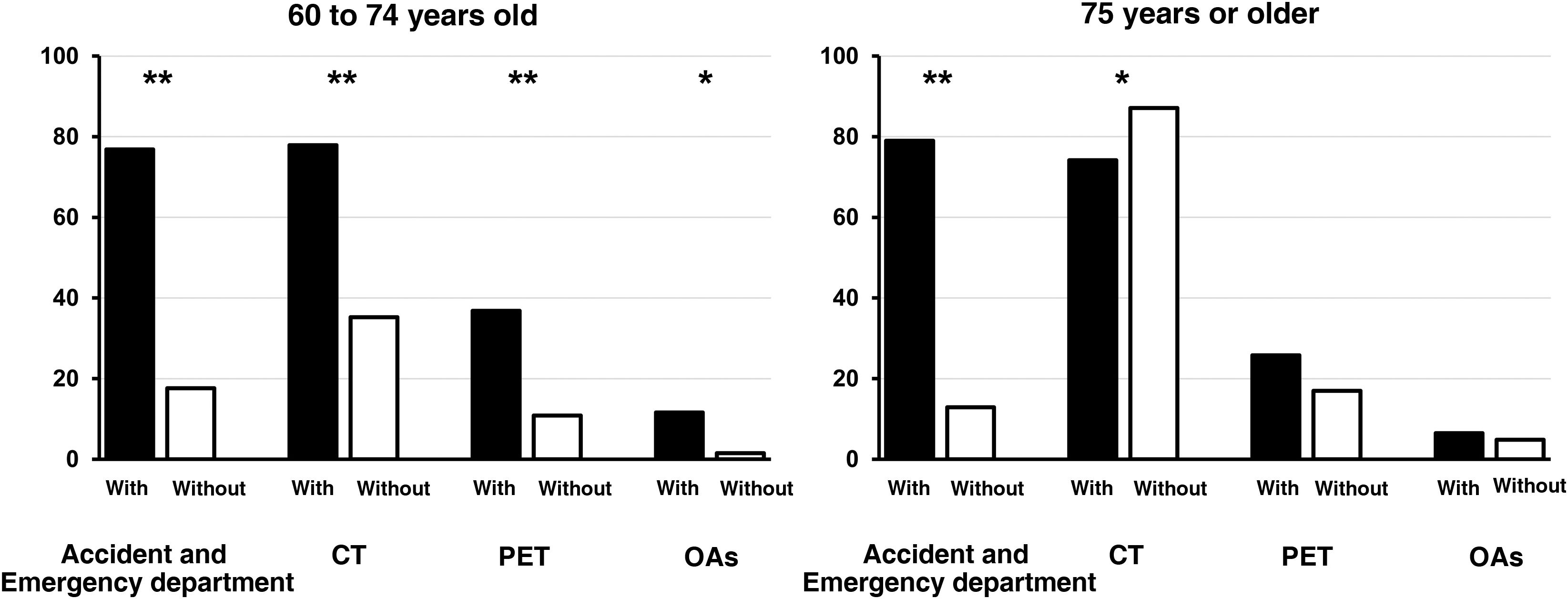
Analysis of the subgroup of early elderly patients also revealed a higher consumption of all resources analysed in patients with a second neoplasm (p < 0.001 for Accident and Emergency department visits, CT and PET; p < 0.05 for OAs). However, late elderly patients without a second neoplasm showed similar PET and OA consumption, higher CT consumption (p < 0.05) and fewer Accident and Emergency department visits (p < 0.001) (Fig. 2).
Comparison of the consumption of healthcare resources by early elderly (60 to 74 years old) and late elderly (75 years old or over) patients with thyroid cancer, depending on the presence (black columns) or absence (white columns) of a second neoplasm. The columns represent the percentage of patients who have used each of the resources that are specified on the x-axis.
CT: computerised axial tomography; OAs: oral anti-angiogenics; PET: positron emission tomography.
*p < 0.05; **p < 0.001.
These results have allowed us to characterize some clinical, histological and health characteristics in patients with thyroid cancer and to compare them by age groups. To our knowledge, this is the first study that uses the novel artificial intelligence methodology to obtain data from an unbiased sample of all patients with thyroid cancer who have been treated in a referral hospital like ours. Our results can be summarised into three groups of findings: prevalence and types of cancer, complications and associated comorbidities, and consumption of healthcare resources.
The first noteworthy finding is that, in the studied population, the prevalence of thyroid cancer was significantly higher in the group of elderly people (60 years old or older) than in young people (up to 59 years old). The elderly also had a higher proportion of cancers other than PTC. Thyroid cancer in people over 60 years of age has traditionally been considered more aggressive, accompanied by greater morbidity and associated with a worse prognosis compared to in patients under this age.17,18 Our results confirm the finding of several authors of more aggressive histological types in those over the age of 60.2,3,5–8 However, our data provide a comparison that has barely been studied in previous publications. In fact, when the late elderly (75 years of age or over) were compared with the early elderly (60–74 years of age), it was observed that they had a lower prevalence of thyroid cancer in general and similar clinical and histological characteristics.
Our finding of a lower rate of hypoparathyroidism in those over 60 years of age compared to young patients is inconsistent with the findings of some other authors.17,18 In addition, in the analysis of subgroups, our study also shows the absence of differences in the frequency of permanent hypoparathyroidism and dysphonia between the late elderly and the early elderly, similar to that found in similar age groups by other authors.3
Our second finding shows that young patients with thyroid cancer have a significant increase in the prevalence of risk factors, cardiovascular diseases (with the exception of stroke) and thromboembolic diseases. However, in the elderly there was no increase in the prevalence of hypertension, ischaemic heart disease, peripheral vascular disease or pulmonary thromboembolism, and a lower frequency of cerebrovascular accident was found. In addition, within the elderly group, early elderly patients only showed increased prevalences of dyslipidaemia, diabetes and obesity, but not of the other cardiovascular risk factors or diseases. In summary, these data suggest that in elderly patients, especially those aged between 60 and 74 years old, the risk of cardiovascular disease and some of its risk factors are eliminated, but this risk increases again after the age of 75 for some of these diseases.
The relationship between cardiovascular comorbidity and thyroid disease has been extensively studied in terms of thyroid dysfunction. Hyperthyroidism is associated with hypertension, arrhythmia, heart disease and thromboembolic disease.19,20 Thyroid hypofunction increases the risk of hypertension, diabetes, dyslipidaemia and ischaemic heart disease.21–23 However, the prevalence of these comorbidities has not been analysed in detail in patients with thyroid cancer. In fact, cancer registries often do not report comorbidities in patients with tumours.24 Only a few authors have indirectly mentioned concomitant diseases in the description of patients with thyroid cancer. A retrospective cohort study demonstrated that the prevalence of hypertension and dyslipidaemia, but not diabetes, in patients with thyroid cancer aged 75 years of age or over was higher than that of a group of patients aged 65–75 years old.11 The mechanisms that may account for the increased frequency of diabetes and dyslipidaemia found in our patients aged 60 years old or over are not easy to explain, although they may be related, at least in part, with the higher prevalence of obesity and a possible increase in insulin resistance in these patients. In this regard, a recent meta-analysis demonstrated that there is an increased risk of thyroid cancer in patients with insulin resistance and diabetes. However, this association was not found with cholesterol or triglyceride levels.25 In contrast to what was found in our patients, a recent cohort study did not find an increased risk of dyslipidaemia in patients with thyroid cancer compared to the general population.26 However, the authors recognise that proper characterization of the risk of dyslipidaemia would require analysis of the influence of the treatments received, levothyroxine dosage and the patients' thyroid-stimulating hormone levels both in the early stages of the disease and in the long term.26
Our data could explain the finding by several authors of a lower overall survival of late elderly patients with thyroid cancer compared to early elderly patients9, which has recently been corroborated in a Spanish multicentre study27. In many of these studies, this higher mortality is attributed to a worse general condition of late elderly patients or to the presence of comorbidities that most of these studies have not analysed. In fact, a recent study of the American SEER database showed that, with the exception of anaplastic thyroid cancer, patients are more likely to die from other causes, including cardiovascular disease, than from thyroid cancer itself.24
Our third finding shows that the late elderly do not appear to be large consumers of healthcare resources when compared to the early elderly. We only observed a significant increase in CT and a slight increase in PET consumption. Furthermore, as one might expect, thyroid cancer patients with a second neoplasm consume more healthcare resources than those without a second tumour, and this was evident in our study in both the young and the elderly. However, when we analysed the elderly subgroups, we observed different behaviour between early elderly and late elderly patients. In the latter, there was only a greater consumption of healthcare resources in terms of Accident and Emergency department visits, but not in the performance of PET or OA consumption. Even use of CT was higher in the late elderly without a second neoplasm. In other words, the late elderly with thyroid cancer and a second cancer are no more resource-consuming than those with thyroid cancer alone.
Although in the literature several authors have analysed the rate of recurrence of thyroid cancer in elderly patients compared with young people,7,8 we have not found any information on the consumption of healthcare resources. We believe that the use of big data tools has allowed us to obtain, for the first time in our country, useful information on the consumption of healthcare resources in these patients, especially in age groups that are generally associated with higher health expenditure. However, our findings are consistent with some studies that have found a higher recurrence rate in elderly patients compared to younger patients with thyroid cancer28 and, therefore, a greater consumption of healthcare resources in the former is plausible. Our results are also consistent with those of a recent Spanish multicentre study,27 which demonstrated that although late elderly people with differentiated thyroid cancer have a lower overall survival than early elderly patients, they did not show an increased risk of developing structural disease.
Taking our results together with those of the aforementioned multicentre study, contrary to what some researchers have described,10 they suggest that in patients with thyroid cancer, being older than 75 years does not entail a greater probability of developing structural disease and, presumably, a greater consumption of healthcare resources. In fact, very recent studies of PTC patients who were actively monitored without surgery have shown that older age is associated with a reduced risk of tumour growth compared with younger subjects.29
The extraction of real-life data and the large sample size constitute the main strengths of our study. The use of new big data techniques and the EHRead® technology developed by Savana has allowed us to evaluate an enormous amount of information, as well as to read, process and sort the free text from the EHRs and convert it into structured data. All diagnoses of more than half a million patients were included in the analysed data, in a verifiable manner and without bias, so conclusions can be drawn from actual clinical practice. The main limitations are those inherent to the use of artificial intelligence tools in large databases, in which detailed individual analysis of the subjects studied is not possible. Therefore, we have not been able to analyse differences according to the histological type and extent of thyroid cancer or the use of radioactive iodine in the treatment of the cancer. Neither have we been able to analyse other cardiovascular problems, such as cardiac arrhythmias. We are also unaware of the severity and duration of the comorbidities. Although the information was obtained in a verifiable manner and without bias, we cannot rule out diagnostic errors or omissions in the EHRs. The cohort studied was patients treated at our hospital, so it may not be representative of the general population.
Our results may have implications for clinical practice. The big data tools used have allowed us to demonstrate that, although elderly patients, compared to younger ones, have worse prognosis data and are generally higher consumers of healthcare resources, they do not present a greater burden of cardiovascular comorbidity. However, when the late elderly are compared with the early elderly, the late elderly show a higher burden of cardiovascular disease, but not as high a consumption of healthcare resources as would be expected for this greater comorbidity. These data support the idea, previously expressed in another study,27 that late elderly patients should be treated with the same therapeutic effort as other elderly patients. We believe that these results are compatible with the current trend in international organisations for the prevention of ageism, as advocated by the WHO30; that is, to avoid stereotypes and existing prejudices in relation to age and therefore avoid discrimination on the grounds of age.
In conclusion, the use of big data tools has allowed us to obtain clinically useful information on the behaviour of thyroid cancer in the elderly. Given that this tumour is a disease with increasing incidence but that maintains a low specific mortality, and that the ageing of the population is an evident fact in recent decades, it is expected that clinicians will increasingly see elderly people with thyroid cancer.31 Elderly people, and especially the late elderly, represent a heterogeneous group of patients with different risks and comorbidities that should be taken into account when making individualised decisions about their clinical approach. Our data, along with those of previous studies,24,25 suggest that planning personalised healthcare for elderly people with thyroid cancer must take into account not only the characteristics of the tumour, but also the particular comorbidities of the patient, but age per se should not be a single limiting factor.
FundingThis research did not receive any financial support from public sector agencies, the commercial sector or non-profit entities.
Conflicts of interestMB, GL, GA and AP are Savana employees and declare that they have no additional conflicts of interest.