Our aim is to assess the changes in clinical nutrition and dietetics education of the residents in endocrinology and nutrition for the last 10 years.
MethodsDuring the yearly update course in Clinical Nutrition and Dietetics held by SEEN, a survey about medical training is conducted since 2006. Descriptive data for the last 10 years are reported.
ResultsEvery hospital accredited for medical training in endocrinology and nutrition has a unit of nutrition, depending on endocrinology and nutrition departments in 94.5%. While 13.3% of the residents required a different hospital for training in nutrition in 2006, all of them had enough resources in their own hospital in 2018. The training started in their third year of residency in 62.6%. The rotation has been increasing its length and now it lasts 6 months for 66% of the residents. 41.9% of the residents think it should be longer than 6 months. Education in dietetics should be extended the most. The residents take part in study protocols or publications in 72.5%, against only 27.9% in 2009. There is still a percentage of 10.1% to 19% of the residents grading their training in nutrition as insufficient.
ConclusionThe residents consider their global training in nutrition has improved in these last 10 years, although there is still a chance for optimization in areas such as dietetics.
El objetivo de este trabajo es evaluar los cambios en la formación en nutrición clínica y dietética de los residentes de endocrinología y nutrición en los últimos 10 años.
MetodologíaEn el Curso Anual de Actualización en Nutrición Clínica y Dietética que organiza la SEEN se realiza una encuesta de formación a los residentes desde 2006. Se recogen los datos descriptivos de los 10 últimos años.
ResultadosTodos los hospitales con docencia acreditada en endocrinología y nutrición disponen de una unidad de nutrición, con dependencia en el 94,5% de los servicios de endocrinología y nutrición. Mientras que en 2006 un 13,3% de residentes necesitaban hacer su rotación en nutrición en otro hospital, en 2018 todos tenían en su hospital recursos suficientes para su formación. Un 62,6% comienzan su formación en nutrición en su tercer año de residencia. La duración de la rotación se ha ido incrementando y está en 6 meses para el 66% de los residentes. Un 41,9% de los residentes considera que su rotación en nutrición debe ser superior a 6 meses. La formación en dietética es la que más consideran que necesitan ampliar. Un 72,5% de los residentes participan en protocolos de estudios o publicaciones, frente a solo un 27,9% en 2009. Existe aún un porcentaje de residentes entre el 10,1 y el 19% que califican como insuficiente su formación global en nutrición.
ConclusiónLos residentes consideran que la formación global en nutrición ha mejorado en estos 10 años, aunque aún existen posibilidades de optimización en áreas como dietética.
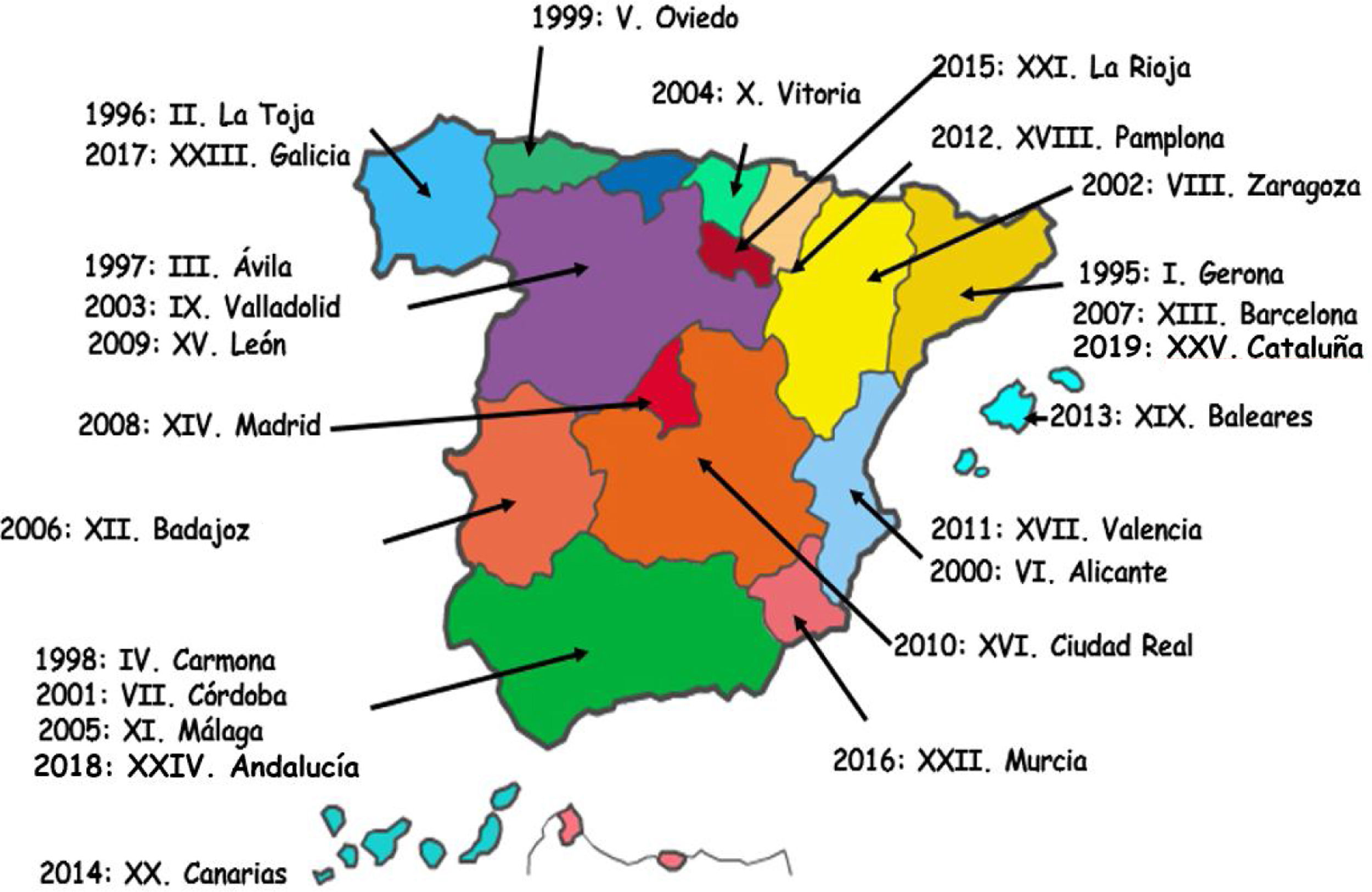
In 2019, the Spanish Society of Endocrinology and Nutrition (Sociedad Española de Endocrinología y Nutrición [SEEN]) is holding the XXV Updating Course in Clinical Nutrition and Dietetics for resident physicians in training (MIR) in Endocrinology and Nutrition. The time interval covered by a generation has traditionally been considered to be the age difference between parents and offspring, with an interval of 25 years being taken to represent an adequate average for a standard generation. Therefore, we can say that a generation has passed since the first course was held in Gerona, in 1995. It seems a good time for a retrospective examination of how training in nutrition has changed in our specialty. Since 2006, a training survey has been completed by all residents in the course of their participation in these courses. The purpose of the present study was to assess the changes in training in clinical nutrition and dietetics among residents in endocrinology and nutrition, based on data collected from these surveys over the last 10 years, and to critically reflect upon such training in our specialty.
Training in clinical nutrition and dietetics in the specialty of endocrinology and nutrition: a historical perspectiveThe responsibilities of specialists in Endocrinology and Nutrition,1 published in 2016, consisit of the study and application of the theoretical bases of feeding and nutrition in healthy and ill subjects, and also the bases, development and application of clinical nutrition (oral, enteral, and parenteral).
The first residents trained in nutrition in that long ago first resident training course in 1995 received a document from the National Commission of the Specialty describing the aspects to be included in their training, which was based on Spanish Royal Decree 127/1984, of 11 January, regulating specialized medical training and the granting of the title of specialist.2 In it, nutrition and dietetics were considered a three-month rotation period in the fourth year of resident training. According to a survey presented at the SEEN congress in 2000,3 82.1% of the residents completed this rotation period. Overall, however, 57.1% of the residents considered that their department did not meet the training objectives in 2000, though without specifying in what areas. Consequently, we do not possess concrete data regarding training in nutrition at this time. The training program for the specialty of endocrinology and nutrition was approved and published in 2006.4 A minimum rotation period of 6 months in a clinical nutrition setting was specified, but no mention was made regarding the year of residency in which the rotation period should take place. The Nutrition Group of the SEEN established the teaching objectives in this area in its constituting document,5 endorsing this rotation period of at least 6 months, though it considered 12 months to be the ideal period.
Going back to 1995, the then Nutrition Working Group of the SEEN, created two years previously, had among its priorities the aim of ensuring compliance with the established teaching agreements on the part of all hospitals accredited for resident training in the specialty. Accordingly, in 1995 it was suggested that the three month training period in nutrition then in effect was quite insufficient. In addition, training in nutrition was clearly heterogeneous among the different teaching units at the time, because clinical nutrition was not supervised by specialists in endocrinology and nutrition in all departments. This made it necessary for many residents to undergo external rotations at other hospital centers. It was in this context that the Updating Course in Clinical Nutrition and Dietetics of the SEEN was held for the first time, the XXV edition of which is scheduled for 2019. This course is considered mandatory for all third year residents in the specialty, though up until 2009 it was targeted to fourth year residents. The course was initially held in a different Spanish city every year, but since 2010 the site has always been Madrid, though the local coordinator is rotated among the different Autonomous Communities, as can be seen in Fig. 1.
From the perspective of the Nutrition Area of the SEEN, it is considered that this course has improved the training of our residents in clinical nutrition and dietetics, overcoming the inevitable variability of the departments of origin, and establishing the theoretical and practical bases of the rotations in the teaching units with a view to promoting more homogeneous nutrition care in Spain. Furthermore, this more homogeneous training in nutrition has led to a greater standardization in the clinical practice of those specialists trained over the last 25 years.
In addition, a training survey has been conducted during the course since 2006, allowing us to assess how nutrition care and training have evolved in these years in the various Departments of Endocrinology and Nutrition.
Methodology: training survey of residents in endocrinology and nutritionEvery year, the SEEN invites its residents to participate in the Updating Course in Clinical Nutrition and Dietetics. During the first years, the fourth year residents (R4) were invited to participate in the course. However, after 10 years it was considered preferable to advance the course to the third year of residency (R3) in order to allow for improved benefits from the subsequent rotations in nutrition, the course serving as a basis in this regard. The transition was carried out during 2008 and 2009, with mixed participation by R3 and R4 residents in that period. Beginning in 2009, the R3 residents were invited to the course, with the exceptional participation of those R4 residents who had been unable to participate in the course as third year residents. The number of participants since 2009 has ranged from 54 to 74, with a median of 68 residents a year.
On the first day of the course, the residents complete a training survey (see Annex. Supplementary material). The first time this training survey was carried out was in 2006, but major changes were introduced in 2009. In addition, since 2009, the participants in the course have been mostly R3 residents and not fourth year residents as before. We therefore consider the data obtained since 2009 to be more comparable. Consequently, descriptive reference will only be made to the data corresponding to the last 10 years. The data are compiled as percentages of answers to each item in each of the years of the survey, with medians and percentage ranges during that period.
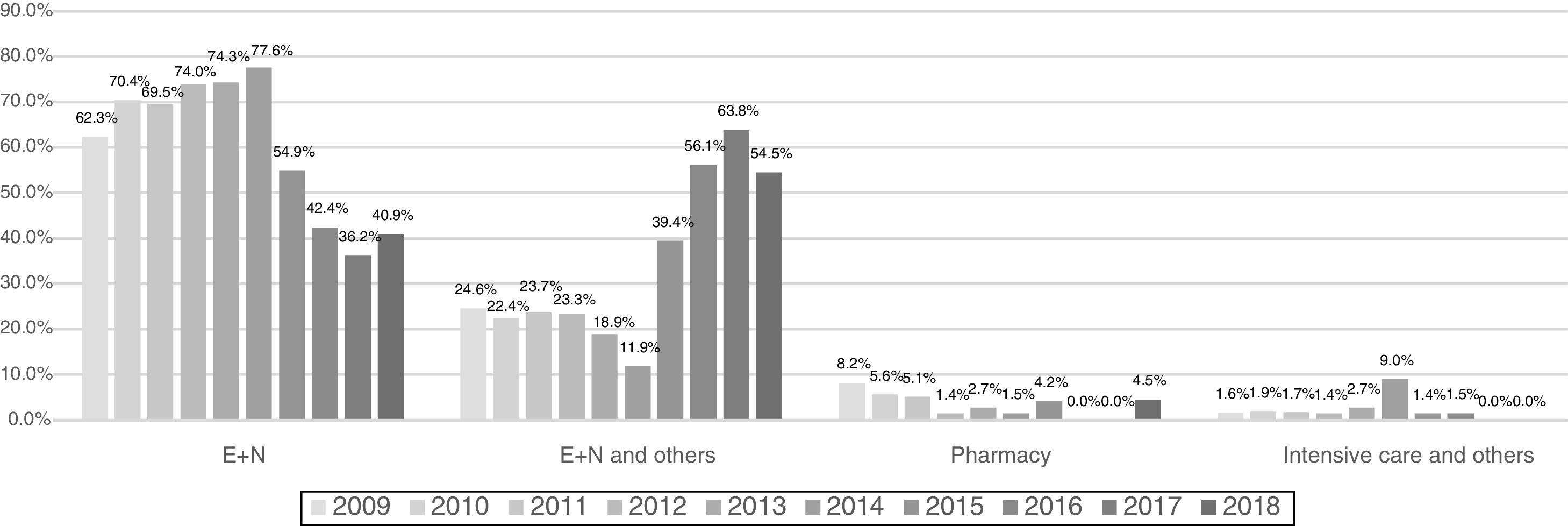
ResultsThe first questions of the survey for residents are about how nutrition is organized in their hospitals of origin. The percentage of hospitals with a nutrition unit and accredited for teaching endocrinology and nutrition has increased from 88.5% in 2009 to 100% in 2017 and 2018. These nutrition units are mostly dependent on endocrinology and nutrition departments or sections (increasing from 77.5% in 2009 to 94.5% in 2018), but an important proportion also include professionals from other specialties, thus demonstrating the multidisciplinary nature of these units (Fig. 2). At present, the specialists in charge of teaching clinical nutrition are practically all endocrinologists, and belong to units that are predominantly led by specialists in endocrinology and nutrition at the teaching hospitals. The residents also reported whether specialists in endocrinology and nutrition were involved in the meal preparation services of their hospitals, the median proportion being in 31.5% of the hospitals, with a range of 19.4–47.5%, a figure that has not changed much over the 10 years of the study. Of note, however, is the fact that a median of 28% of the R3 residents did not know who supervised the meal preparation services of their hospitals. Fortunately, this percentage lack of awareness has gradually decreased, from 37.7% in 2009 to only 10.9% in 2018.
The second set of questions in the survey specifically refers to the characteristics of the rotation of the residents in clinical nutrition. The data available from the first surveys in 2006 showed that in 13.3% of the cases the residents were obliged to perform their rotation in another hospital, due to the lack of a sufficiently consolidated unit at their own center. In 2009, a total of 8.2% of the residents still had to leave their hospital, but fortunately this number has gradually decreased, and in 2018 all R3 residents had adequate resources for training in nutrition at their own hospital. The percentage of residents who only rotate within their own hospital has remained stable, with a median of 65.5%, and the percentage of those who, while rotating in their hospital, complete their training at another center has increased from 24.6% in 2009 to 31.2% in 2018.
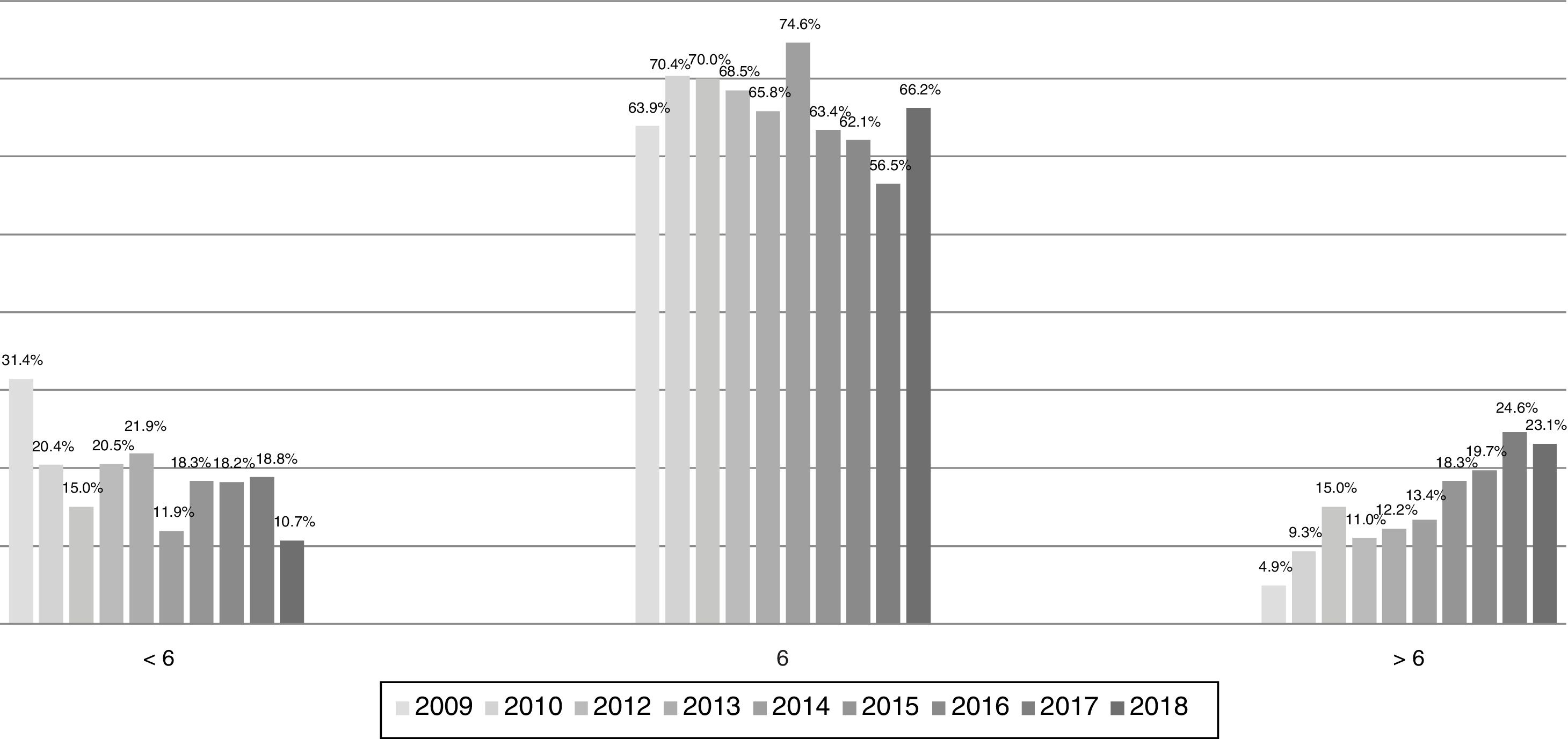
The residents mainly start training in nutrition in their third year, with a median proportion of 62.6% and a range of 41–71% during the years of follow-up. However, a progressive increase is observed in the percentage of residents that start training in the first and second years of residency (8% and 20.6% in 2018, respectively). The duration of the rotation period has gradually increased, as shown in Fig. 3. Although the median remains stable at 6 months for 66% of the residents, in 2009 a total of 31% rotated for less than 6 months and only 8.8% for a longer period. However, these figures have gradually become inverted, and in 2018 they were found to be 10.7% and 23.1%, respectively. This inversion in figures corresponds to the answer to the question about how long the residents feel the rotation period should be. While in 2009 only 19.7% wanted to rotate for more than 6 months, at present 41.9% of the residents think that their rotation period in nutrition should be longer than 6 months.
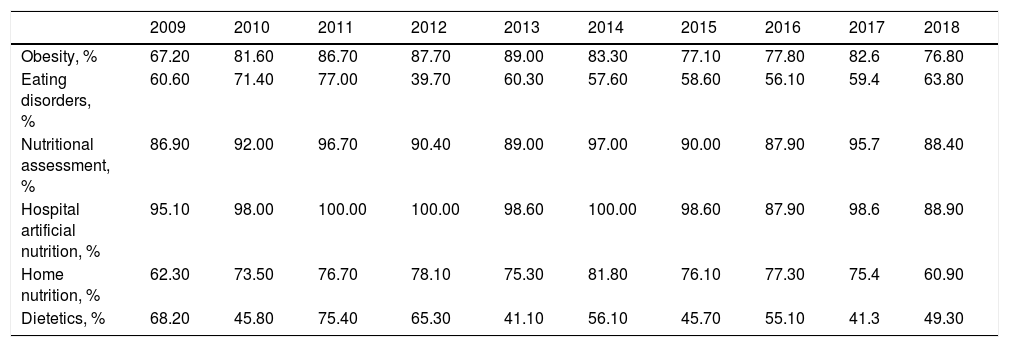
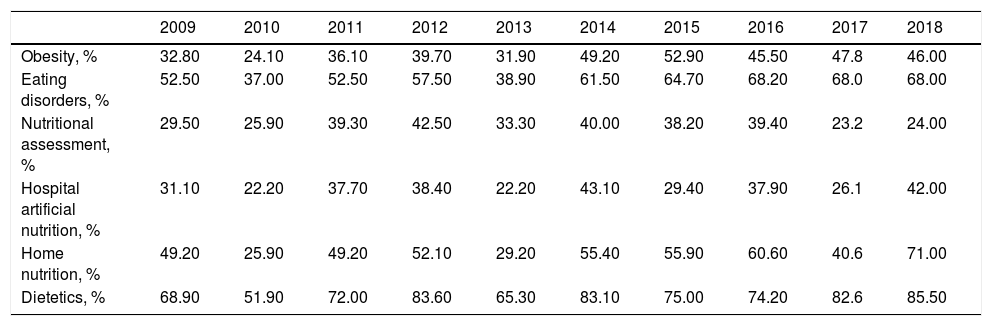
The rotation training contents have remained quite stable over these 10 years, as is seen in Table 1, and the limited amount of training received in dietetics continues to stand out. This observation is consistent with the fact that training in dietetics is precisely the area which the residents feel should be prolonged (Table 2) (the opinion of 85.5% of all residents in 2018).
Contents included in nutrition rotation, evolution during the period 2009–2018.
| 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Obesity, % | 67.20 | 81.60 | 86.70 | 87.70 | 89.00 | 83.30 | 77.10 | 77.80 | 82.6 | 76.80 |
| Eating disorders, % | 60.60 | 71.40 | 77.00 | 39.70 | 60.30 | 57.60 | 58.60 | 56.10 | 59.4 | 63.80 |
| Nutritional assessment, % | 86.90 | 92.00 | 96.70 | 90.40 | 89.00 | 97.00 | 90.00 | 87.90 | 95.7 | 88.40 |
| Hospital artificial nutrition, % | 95.10 | 98.00 | 100.00 | 100.00 | 98.60 | 100.00 | 98.60 | 87.90 | 98.6 | 88.90 |
| Home nutrition, % | 62.30 | 73.50 | 76.70 | 78.10 | 75.30 | 81.80 | 76.10 | 77.30 | 75.4 | 60.90 |
| Dietetics, % | 68.20 | 45.80 | 75.40 | 65.30 | 41.10 | 56.10 | 45.70 | 55.10 | 41.3 | 49.30 |
Percentage of residents wishing to extend their training in specific areas, evolution during the period 2009–2018.
| 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Obesity, % | 32.80 | 24.10 | 36.10 | 39.70 | 31.90 | 49.20 | 52.90 | 45.50 | 47.8 | 46.00 |
| Eating disorders, % | 52.50 | 37.00 | 52.50 | 57.50 | 38.90 | 61.50 | 64.70 | 68.20 | 68.0 | 68.00 |
| Nutritional assessment, % | 29.50 | 25.90 | 39.30 | 42.50 | 33.30 | 40.00 | 38.20 | 39.40 | 23.2 | 24.00 |
| Hospital artificial nutrition, % | 31.10 | 22.20 | 37.70 | 38.40 | 22.20 | 43.10 | 29.40 | 37.90 | 26.1 | 42.00 |
| Home nutrition, % | 49.20 | 25.90 | 49.20 | 52.10 | 29.20 | 55.40 | 55.90 | 60.60 | 40.6 | 71.00 |
| Dietetics, % | 68.90 | 51.90 | 72.00 | 83.60 | 65.30 | 83.10 | 75.00 | 74.20 | 82.6 | 85.50 |
In addition to the clinical aspects, the training survey also examines the training received in the form of clinical sessions. In general, the number of clinical sessions referring to nutrition in teaching departments is very heterogeneous, ranging from 0 to 6 a month. The current median is only one session a month, and residents think that this should be increased to two, though here the range is also broad (0–8). The evolution experienced over these years has reduced the percentage of departments in which no nutrition sessions are held (from 39.3% in 2009 to 13.6% in 2018). The most common periodicity of these sessions is 1–2 per month (in 36.6% of the departments). However, in 2018, a total of 73.2% of the residents considered that the periodicity should be 1–2 sessions a month.
With regard to other training activities, the percentage of residents attending nutrition congresses or meetings (apart from the National Congress of the SEEN) has gradually increased since 2009 from 39.3% to 60.9%. In addition, 72.5% of the residents participate in study protocols or publications, as compared to only 27.9% in 2009.
Overall, the residents have generally had a good opinion of the Updating Course in Clinical Nutrition and Dietetics, and this favorable opinion has moreover become strengthened over the years. Indeed, in 2009 a total of 60.7% of the surveyed residents considered the course to be very interesting and 37.7% interesting, while in 2018 these figures improved to 81% and 16%, respectively. Since 2015, the residents have also been asked about their global opinion regarding their training in nutrition. Although in this period 2015–2018 a total of 10.10–18.2% considered their training to be excellent, 36.4–60.9% very good and 18.8–32.3% good, there is still an important proportion (10.1–19%) of residents who rated it as insufficient.
DiscussionClinical nutrition and dietary care in Spanish hospitals has changed greatly over the last 25 years. The recent RECALSEEN survey, whose preliminary results have just been published,6 has shown that 83% of all Departments of Endocrinology and Nutrition now have a Clinical Nutrition Unit (CNU). This percentage reaches 98% in hospitals with 500 or more beds. The teaching of the specialty has changed similarly, and the training survey conducted among the residents annually during the Updating Course in Clinical Nutrition and Dietetics reflects this.
It should be taken into account that the percentage of departments in which the residents in endocrinology and nutrition considered that the training objectives were not met has gradually decreased in the course of these 25 years. The analysis of the results of the survey shows that 57.1% of the residents considered that their department did not meet the training objectives in 2000,3 versus 40% in 20047 and – pleasingly – only 17.5% in 2009,8 though without specifying in what areas. We therefore do not have concrete data referring to training in nutrition. Nevertheless, training in nutrition has improved, as is reflected by the data obtained, and this improvement has contributed to the further achievement of the training objectives.
The training survey is a good tool for evaluating the changes made in recent years in both the healthcare and teaching contexts, since practically all the residents of the accredited teaching units have been on the course. We have focused on the data corresponding to the last 10 years, because this is the period in which the survey has been most consolidated, after several changes in the survey, and because in 2008–2009 the decision was made to invite R3 residents instead of R4 residents. The survey reflects the reality of nutritional care in teaching hospitals, and the data from the nutrition units available in virtually all teaching departments – most of which are dependent upon a Department of Endocrinology and Nutrition – are similar to those reported in the RECALSEEN survey.6
One of the areas of improvement reflected in our survey concerns hospital meal preparation services. In recent years, with the publication of the PREDYCES study,9 a serious problem of disease-related malnutrition has been found at our hospitals. Almost 10% of all patients suffer worsened nutritional status during their hospital stay, and the care of these patients is 50% more expensive. Improving the meal preparation services of our hospitals to adapt them to the needs of the patients should therefore be a priority in our healthcare system. However, in only one out of every three hospitals are specialists in endocrinology and nutrition involved in supervising these services. Unfortunately, we have not been able to convey to our residents the importance of such supervision, since a large percentage of them do not know who supervises the meal preparation services at their hospitals. Fortunately, this percentage lack of awareness has gradually decreased, from 37.7% in 2009 to only 10.9% in 2018. Our involvement in hospital meal preparation services, directly related to our indications1 on the study and application of the theoretical bases of dietetics and nutrition in healthy and ill subjects, should lead to a decrease in the high incidence of disease-related malnutrition.
Improvement in the nutrition units is also shown by the fact that there are no longer residents who need to undergo training in nutrition outside their own hospital, since the nutrition units of the teaching hospitals offer the necessary teaching means. Two out of three residents only rotate within their own hospital, although the percentage of those who, even while rotating in their hospital, complete their training at another center has increased. However, the residents were not questioned about whether such dual rotation was because their own hospital was unable to offer minimally sufficient training or because they personally wished to widen their training experience in clinical nutrition by visiting certain reference centers.
A greater interest in training in nutrition also appears to be shown by the fact that the start of training has gradually been introduced earlier, and especially because the duration of the rotation in nutrition has been prolonged. Furthermore, 41.9% of the residents are of the opinion that their rotation in nutrition should last longer than 6 months. This would facilitate an increase in training in several fields, but particularly in dietetics, as requested by almost all residents. This necessary increase in training time in nutrition must be compatible with the increase in global training time in the speciality of Endocrinology and Nutrition, whose teaching objectives have also increased in recent years. As a result, the current duration of the resident training program now seems too short; this points to the need for an additional year of specialty training, as we have already suggested to the National Commission of the Specialty.
It is true that clear improvements have been seen in other training activities, such as participation in nutrition congresses or meetings, and in study protocols or publications. However, the number of clinical sessions dedicated to nutrition should be improved in our teaching units, because they are still too few, and most residents demand more frequent sessions than are available at present.
The objectives of this study were two-fold: to assess the importance of the course in the training of residents, and to evaluate the training received during the residency period based on the training survey. Overall, the residents have a high opinion of the Updating Course in Clinical Nutrition and Dietetics, and this favorable opinion has strengthened over the years, to the point where most of them consider the course to be very interesting. Global training in nutrition may still be open to improvement, however, because a significant proportion of residents (10.1–19%) still consider it to be insufficient. As commented above, a longer duration of rotation – at least 9 months and preferably one full year, as was already stated in the document constituting the field of Nutrition5 – could help meet the training expectations of our residents and thereby ensure better nutritional care in our hospitals.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Thanks are due to all the past and present members of the Steering Committee of the Area of Nutrition of the SEEN, particularly Gabriel Olveira-Fuster, for his statistical support in the analysis of the first years of the training survey; Dolores del Olmo-García, Alejandro Sanz-París, Julia Ocón-Bretón, Juan José López-Gómez and Luis Miguel Luengo-Pérez, for their invaluable help with the questionnaires; and to Francisco Botella-Romero, Miguel Ángel Martínez-Olmos, Pilar Gómez-Enterría, Miguel León-Sanz, Pilar García-Peris, Diego Bellido-Guerrero, Daniel de Luis-Román, Pedro Pablo García-Luna, Nuria Virgili, Clotilde Vázquez, Lucio Cabrerizo-García and Aniceto Charro-Salgado.
Thanks are also due to Nutricia Advanced Clinical Nutrition and Abbott Nutrition for their sponsorship of the Updating Course in Clinical Nutrition and Dietetics for residents of the SEEN.
Please cite this article as: Ballesteros Pomar MD, Álvarez Hernández J, Bretón Lesmes I, en nombre del Comité Gestor del Área de Nutrición de la SEEN. Formación en nutrición en los médicos residentes en endocrinología y nutrición: ¿cómo hemos cambiado? Endocrinol Diabetes Nutr. 2019;66:346–352.