Ultrasound-guided fine needle aspiration of thyroid nodules with on-site cytological examination may decrease the number of Bethesda category I cytologies. The study objective was to evaluate our second-year experience with this procedure to analyze diagnostic efficacy, prevalence, and factors predicting for Bethesda category I results.
Patients and methodA retrospective study was conducted of 279 nodules from 233 patients. Ultrasound-guided fine needle aspiration was performed according to the 2015 criteria of the American Thyroid Association. A specimen of each aspiration was air-fixed on site before Diff-Quik staining and microscopic examination to assess its suitability; otherwise, nodule aspiration was repeated up to 5 times. Diagnostic efficacy was assessed based on sensitivity and specificity on the cytological categories Bethesda II and Bethesda VI.
ResultsDiagnostic sensitivity and specificity were both 100%, 5.4% Bethesda category I results were obtained, and variables independently associated were age (4.7% increase per year of life) and nodule volume (2.3% increase per each 1ml of volume).
ConclusionsUltrasound-guided fine needle aspiration of thyroid nodules with on-site cytological examination allows for a high diagnostic efficacy and has been shown to be a highly relevant procedure because it has a very low rate of cytological results of Bethesda category I, whose risk has been higher in older subjects and with larger nodules.
El procedimiento de punción-aspiración con aguja fina ecoguiada de nódulos tiroideos con examen citológico in situ del material extraído puede reducir el número de citologías obtenidas de categoría Bethesda I. El objetivo del estudio ha sido evaluar nuestra experiencia del segundo año en dicha técnica para analizar la eficacia diagnóstica, la prevalencia y los factores predictores de los resultados de categoría Bethesda I.
Pacientes y métodoEstudio retrospectivo sobre 279 nódulos en 233 pacientes. La punción-aspiración se realizó según los criterios de 2015 de la American Thyroid Association. Una muestra de cada punción se fijó al aire y se procesó in situ mediante tinción con Diff-Quik y examen microscópico para valorar su idoneidad; en caso contrario, se repitió la punción hasta un total de 5veces. La eficacia diagnóstica se valoró en base a la sensibilidad y a la especificidad sobre las categorías citológicas Bethesda II y Bethesda VI.
ResultadosLa sensibilidad y la especificidad diagnóstica fueron del 100% en ambos casos. Obtuvimos un 5,4% de resultados de categoría Bethesda I y las variables independientemente asociadas fueron la edad (incremento del 4,7% por cada año de vida) y el volumen del nódulo (incremento del 2,3% por cada 1ml de volumen).
ConclusionesLa punción-aspiración ecoguiada con aguja fina y examen citológico in situ del material extraído permite obtener una elevada eficacia diagnóstica y demuestra ser un procedimiento de gran validez por conseguir una tasa muy baja de resultados citológicos de categoría Bethesda I, cuyo riesgo ha sido superior en sujetos de mayor edad y en nódulos de mayor tamaño.
The main objective in patients with nodular goiter is to recognize the potential malignancy of the condition. Although the probability of malignancy is low (5–15%), the high prevalence of nodular goiter in the population (5–68% depending on whether detection is made by palpation or ultrasound) results in a large number of patients with thyroid cancer.1,2 Three approaches are available for establishing the benign or malignant nature of a thyroid nodule: endocrine assessment, ultrasound examination, and cytological study of fine needle aspiration material, the latter technique being particularly relevant in this regard.1–3 These procedures allow for the selection of malignant nodules for surgical treatment and the avoidance of unnecessary surgery and its potential sequelae in the case of benign nodules.4
The Bethesda classification has been adopted in recent years for the cytological diagnosis of thyroid nodules. Sometimes a Bethesda category I result is obtained (sample not suitable for cytological diagnosis). The Bethesda expert panel has recommended that the procedures used to establish a thyroid nodule cytological diagnosis should yield an incidence of Bethesda category I results of no more than 10%.5,6 This percentage is closely related to the ultrasound and histopathological characteristics of the nodule, and to the quality of the cytology procedure performed.2,5,7–12 Therefore, it is advised that each individual center should compile, analyze and assess its cytological and histopathological results of patients with nodular goiter. In the event of a Bethesda category I cytological result, the recommendation is to repeat cytology under ultrasound guidance and, if possible, to perform on-site cytological evaluation of the extracted material, or to obtain a core needle biopsy.1,2,5,6,13–15 Although ultrasound has been incorporated into this procedure in most centers,2 the same cannot be said of on-site cytological assessment of the extracted material, due to a lack of human resources and the high costs involved in certain circumstances.10,16–18
Some studies have sought to establish ultrasound or the cytological features associated with the potential malignancy of nodules with Bethesda category I cytological results.11,19 However, few studies have identified the clinical markers predictive of a Bethesda category I cytological result.7,20,21
The purpose of this study was to assess the results obtained during the second year of our experience using ultrasound-guided fine needle aspiration biopsy of thyroid nodules with on-site cytological evaluation of the extracted material. We present the cytological results of the total nodules and the histopathological findings in patients subjected to surgery, with emphasis on the analysis of the diagnostic efficacy, prevalence and predictors of Bethesda category I results.
Material and methodsA retrospective study was made in a hospital setting, describing standard clinical practice and involving patients seen during the second year of our experience of using ultrasound-guided fine needle aspiration of thyroid nodules with an on-site cytological evaluation (from May 2017 to May 2018, both included) at the thyroid nodule puncture-aspiration clinic. Patients with a history of thyroidectomy due to thyroid cancer and cervical lymph node cytological studies were excluded. The time interval was divided into two consecutive 6-month periods to determine whether the learning curve had been completed. The study was reviewed and approved by the Clinical Research Ethics Committee of the Fundació Asistencial Mútua de Terrassa. Informed consent was obtained from all the patients.
A total of 233 patients were enrolled and 279 nodules were evaluated. The primary endpoint was the result of the cytological examination based on the Bethesda classification.5,6 The secondary endpoints were: patient age, gender, the type of goiter (single or multinodular at ultrasound), the echogenicity of the solid portion of the nodule (very hypoechoic if more hypoechoic than the pre-thyroid muscles, hypoechoic, isoechoic or hyperechoic in relation to the adjacent thyroid parenchyma), the presence of microcalcifications in the nodule (no, yes or doubtful), the nature of the nodule (solid, mixed solid-cystic, or predominantly cystic if the latter component represented >50%), nodule diameters in height, width, length and derived measures (diameter in height greater than or not greater than the diameter in width, major diameter, major diameter >4cm, major diameter <1cm, volume calculated using the ellipsoid formula: height (mm)×width (mm)×length (mm)×0.525/1000), the nodule vascularization pattern (peripheral or central), plasma thyroid-stimulating hormone [TSH] and free thyroxine levels in patients not receiving thyroid replacement or antithyroid therapy, plasma thyroid antibodies (positivity for thyroperoxidase and/or thyroglobulin antibodies), the number of punctures in each nodule (the number of passages), and the histopathological result if the patient underwent surgery. Hyperthyroidism was considered for TSH<0.1mIU/ml, while hypothyroidism was defined as TSH>4.5mIU/ml.
Puncture-aspiration was performed of the single thyroid nodule, and in cases of multinodular goiter of the dominant nodule (i.e., the largest nodule) and/or of nodule(s) with ultrasound features suggestive of malignancy according to the criteria of the American Thyroid Association 2015.1 The ultrasound-guided puncture-aspiration procedure was performed by a single endocrinologist (LGP). A 6–11MHz linear probe with an Esaote model 2015 MyLab Seven U185F1 system was used for the ultrasound examination. We used 23 or 25G needles fitted to a 10-ml syringe, without anesthesia and with no biopsy guide. Two cytology technicians (MLS and XM) participated in the processing of the extracted sample, which was distributed into pairs of slides that were placed over each other to ensure that they would contain similar material. One of the slides was air-fixed and processed on-site with Diff-Quick staining, followed by microscopic examination to determine whether the criterion of adequate material for cytological diagnosis was met (i.e., the presence of at least 6 groups of 10 follicular cells).5 If the criterion was not met, nodule puncture was repeated up to a total of 5 times. The other material slide was fixed in 96° alcohol and sent to the pathology laboratory for study after Papanicolaou staining. Whenever possible, preparations of the cytological block from the obtained sample were made.
When a Bethesda category I or III result was obtained, it was left to the discretion of the patient and the treating physician to decide whether to repeat the cytology study within 2–3months, to conduct clinical and ultrasound follow-up, or to perform surgical resection of the lesion. Surgery was indicated in patients with compressive multinodular goiter and in all those in whom the cytology findings were suggestive of follicular neoplasm (Bethesda IV), suggestive of malignancy (Bethesda V), indicative of malignancy (Bethesda VI) or indicative of benign disease (Bethesda II) but with ultrasound findings highly suggestive of malignancy.1
The statistical analysis comprised the calculation of the mean±standard deviation (SD) for continuous variables, and the reporting of the number of cases (n) and percentages (%) for qualitative variables. The diagnostic efficacy of the method was evaluated based on the calculation of the sensitivity and specificity of the histopathological results obtained in the patients with Bethesda categories II and VI. The relationship between the qualitative variables was explored using the chi-squared test or Fisher exact test where appropriate, and the differences in the quantitative variables with respect to the qualitative variables of the two groups were analyzed using the Student t-test. In order to analyze the predictors of a Bethesda category I cytological result, we grouped the cases into a binary dependent variable (yes/no), with the application of a stepwise logistic regression model. Statistical significance was considered for p<0.05.
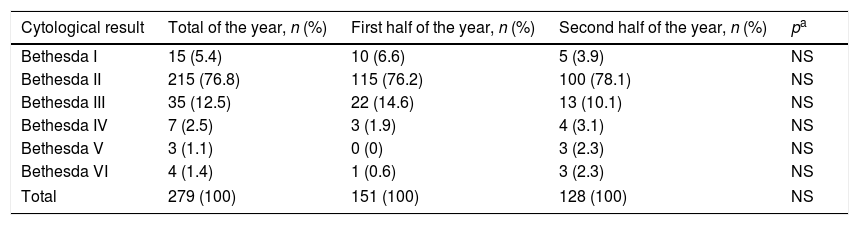
ResultsBetween May 2017 and May 2018, a total of 279 cytological studies were made using fine needle aspiration under ultrasound control with on-site evaluation of the material extracted from the thyroid nodules of 233 patients. Table 1 shows the results and distribution obtained during the first and second half of the year. No statistically significant differences in the results were observed between the two periods. The incidence of Bethesda category I results was 5.4%. A sample suitable for cytological diagnosis was obtained with the first passage in 112 nodules (40.1%). Cytology was only repeated in 10 nodules with an initial Bethesda category III result, obtaining Bethesda category II cytology in 7 cases, and Bethesda category III, IV and VI results in one case each.
Results of the 279 cytological evaluations performed by fine needle aspiration with ultrasound control and on-site cytological examination of the extracted material, distributed into half-year periods for the second year of our experience with the technique.
| Cytological result | Total of the year, n (%) | First half of the year, n (%) | Second half of the year, n (%) | pa |
|---|---|---|---|---|
| Bethesda I | 15 (5.4) | 10 (6.6) | 5 (3.9) | NS |
| Bethesda II | 215 (76.8) | 115 (76.2) | 100 (78.1) | NS |
| Bethesda III | 35 (12.5) | 22 (14.6) | 13 (10.1) | NS |
| Bethesda IV | 7 (2.5) | 3 (1.9) | 4 (3.1) | NS |
| Bethesda V | 3 (1.1) | 0 (0) | 3 (2.3) | NS |
| Bethesda VI | 4 (1.4) | 1 (0.6) | 3 (2.3) | NS |
| Total | 279 (100) | 151 (100) | 128 (100) | NS |
NS: nonsignificant
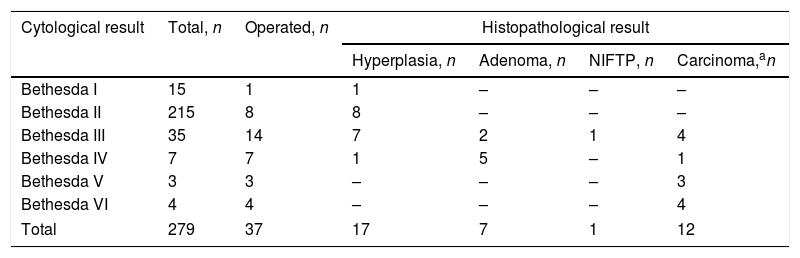
Table 2 shows the histopathological results of the patients operated on according to the previous cytology findings. As there were no false negative or false positive cases in Bethesda categories II and VI, the diagnostic sensitivity and specificity were 100% in both cases.
Histopathological diagnosis in patients operated on according to the prior cytological result.
| Cytological result | Total, n | Operated, n | Histopathological result | |||
|---|---|---|---|---|---|---|
| Hyperplasia, n | Adenoma, n | NIFTP, n | Carcinoma,an | |||
| Bethesda I | 15 | 1 | 1 | – | – | – |
| Bethesda II | 215 | 8 | 8 | – | – | – |
| Bethesda III | 35 | 14 | 7 | 2 | 1 | 4 |
| Bethesda IV | 7 | 7 | 1 | 5 | – | 1 |
| Bethesda V | 3 | 3 | – | – | – | 3 |
| Bethesda VI | 4 | 4 | – | – | – | 4 |
| Total | 279 | 37 | 17 | 7 | 1 | 12 |
NIFTP: noninvasive follicular thyroid neoplasm with papillary-like nuclear features.
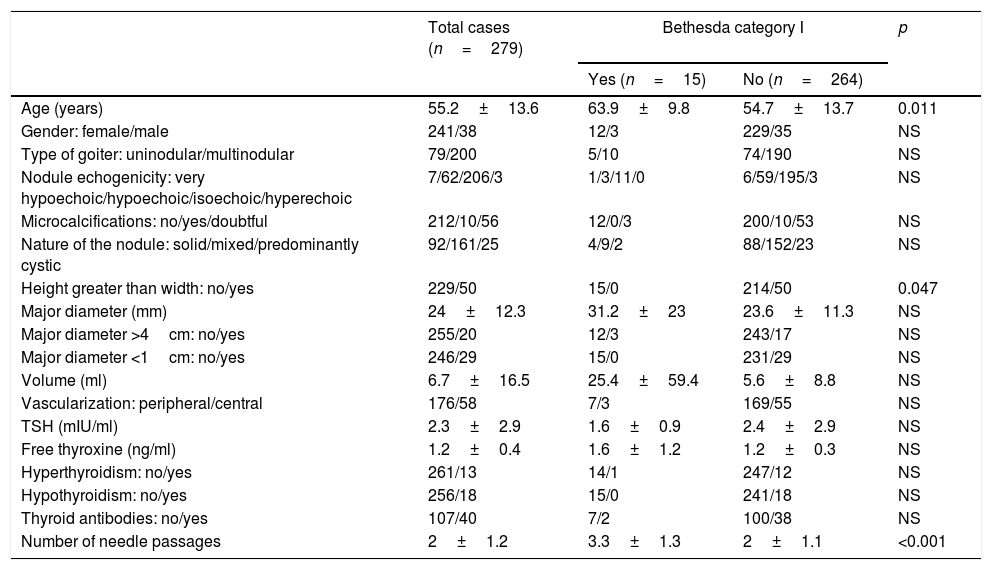
The univariate analysis of the predictors of a Bethesda category I cytological result is shown in Table 3. Retrospective data compilation resulted in missing data for some variables of some of the patients. In this regard, thyroid antibody data were available in 52.7% of the patients, free plasma thyroxine results in 77.4%, and data on the type of nodule vascularization in 83.9%.
Results of the variables studied in the total study subjects and a comparison of patients with Bethesda category I nodules with the other Bethesda cytological categories.
| Total cases (n=279) | Bethesda category I | p | ||
|---|---|---|---|---|
| Yes (n=15) | No (n=264) | |||
| Age (years) | 55.2±13.6 | 63.9±9.8 | 54.7±13.7 | 0.011 |
| Gender: female/male | 241/38 | 12/3 | 229/35 | NS |
| Type of goiter: uninodular/multinodular | 79/200 | 5/10 | 74/190 | NS |
| Nodule echogenicity: very hypoechoic/hypoechoic/isoechoic/hyperechoic | 7/62/206/3 | 1/3/11/0 | 6/59/195/3 | NS |
| Microcalcifications: no/yes/doubtful | 212/10/56 | 12/0/3 | 200/10/53 | NS |
| Nature of the nodule: solid/mixed/predominantly cystic | 92/161/25 | 4/9/2 | 88/152/23 | NS |
| Height greater than width: no/yes | 229/50 | 15/0 | 214/50 | 0.047 |
| Major diameter (mm) | 24±12.3 | 31.2±23 | 23.6±11.3 | NS |
| Major diameter >4cm: no/yes | 255/20 | 12/3 | 243/17 | NS |
| Major diameter <1cm: no/yes | 246/29 | 15/0 | 231/29 | NS |
| Volume (ml) | 6.7±16.5 | 25.4±59.4 | 5.6±8.8 | NS |
| Vascularization: peripheral/central | 176/58 | 7/3 | 169/55 | NS |
| TSH (mIU/ml) | 2.3±2.9 | 1.6±0.9 | 2.4±2.9 | NS |
| Free thyroxine (ng/ml) | 1.2±0.4 | 1.6±1.2 | 1.2±0.3 | NS |
| Hyperthyroidism: no/yes | 261/13 | 14/1 | 247/12 | NS |
| Hypothyroidism: no/yes | 256/18 | 15/0 | 241/18 | NS |
| Thyroid antibodies: no/yes | 107/40 | 7/2 | 100/38 | NS |
| Number of needle passages | 2±1.2 | 3.3±1.3 | 2±1.1 | <0.001 |
NS: nonsignificant.
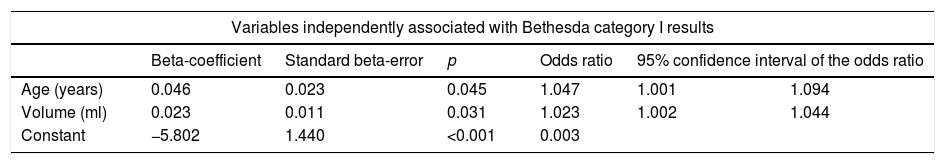
The multivariate binary logistic regression analysis found the variables independently associated with a Bethesda category I result to be patient age and nodule volume (Table 4).
Binary logistic regression findings referring to the prediction of Bethesda category I cytological results in thyroid nodules.
| Variables independently associated with Bethesda category I results | ||||||
|---|---|---|---|---|---|---|
| Beta-coefficient | Standard beta-error | p | Odds ratio | 95% confidence interval of the odds ratio | ||
| Age (years) | 0.046 | 0.023 | 0.045 | 1.047 | 1.001 | 1.094 |
| Volume (ml) | 0.023 | 0.011 | 0.031 | 1.023 | 1.002 | 1.044 |
| Constant | −5.802 | 1.440 | <0.001 | 0.003 | ||
During the second year of our experience with ultrasound-guided fine needle aspiration of thyroid nodules with on-site cytological assessment of the extracted material, we evaluated 279 nodules, with a diagnostic sensitivity and specificity of 100% and a 5.4% incidence of Bethesda category I cytological results, thus demonstrating both high diagnostic efficacy and a high validity of the procedure. Patient age (4.7% increase per added year of age) and nodule volume (2.3% increase per added 1ml of volume) were identified as predictors of Bethesda category I results.
The Bethesda cytological diagnostic categories II and VI are considered definitive, because they represent the maximum expression of benign and malignant lesions, respectively. All other Bethesda categories represent intermediate grades of malignancy.22 According to the Bethesda consensus, a false negative rate of between 0% and 3% in Bethesda category II (benign lesion) and a false positive rate of between 1% and 3% in Bethesda category VI (malignant lesion) is regarded as acceptable.5,6 In our series, the diagnostic procedure based on ultrasound-guided fine needle aspiration with on-site cytological examination of the extracted material yielded very good results in terms of diagnostic sensitivity and specificity in the definitive Bethesda categories, since there were no false negative cases among the patients operated on (all Bethesda category II results were effectively benign nodules in the histopathological study) and no false positive cases (all Bethesda category VI results were confirmed to be malignant nodules in the histopathological study). However, in the future these results will need to be compared with a larger number of patients undergoing surgery.
The incidence of thyroid nodules with a cytological diagnosis corresponding to Bethesda category I ranges from 0.6% to 47%, though most series report figures of 8–20%,1,2,11 and the series published in our setting offered figures of 2.3–27.2%.23–27 At our center, the incidence of Bethesda category I results was 19.8% before the introduction of the ultrasound-guided technique with on-site evaluation of the extracted material.28 The consequences of obtaining a Bethesda category I cytological result include repetition of the cytological study, patient anxiety, and sometimes needless surgery.14,17,26
The collection of adequate material for cytological diagnosis in thyroid nodule puncture-aspiration is conditioned by prior experience with the procedure, the technique used, and the characteristics of the target nodule.1,8,14–17,19,23 In recent years, ultrasound-guided puncture has been incorporated thanks to its superior results, and as a result of the increased availability of ultrasound systems, the technique has been adopted by Departments of Endocrinology and Head and Neck Surgery, thereby facilitating the diagnostic process.10,13 At the same time, it has been regarded as necessary to establish quality measures to ensure that the procedure is performed correctly. As a quality measure, some studies have analyzed the learning curve of the technique, based on the number of inadequate sample results (Bethesda category I) obtained over time.10,12 According to the most demanding authors, learning is achieved when the adequate samples rate obtained is 90–95%,10 while others consider that experienced units (i.e., those performing >100 punctures/year) ideally should record an incidence of Bethesda category I results of under 10–15%.2,5,6,9,11 In our series, the 5.4% incidence recorded in our second year of experience demonstrates the adequate quality of ultrasound-guided fine needle aspiration with on-site cytological assessment of the extracted material, and the fact that no significant differences were observed between the first and second half of the year suggests that stability has been achieved in the learning curve.
In the event of a Bethesda category I result, the American Thyroid Association recommends the repetition of the cytological study under ultrasound control and, if possible, with on-site cytological examination of the extracted material, in view of its superior diagnostic performance.13,14 On-site cytological assessment of the material obtained from the puncture of thyroid nodules by a cytology technician or pathologist for the purpose of confirming sample quality is not always possible, and is consequently not performed at many centers.16,17 Moreover, the cost-effectiveness of the procedure has been questioned.17,18 When on-site cytological assessment is not performed, there is no clear criterion for defining the number of nodule passages to be made in order to secure an adequate sample. Some studies have focused on finding alternatives in order to obtain results comparable to those afforded by on-site cytological assessment of the extracted material. In one of them, performing four needle passages in each nodule reduced the number of Bethesda category I results to 11%,16 while in another study three passages in each nodule resulted in a 13.7% incidence of Bethesda category I results.17 Both situations may be excessive for many patients, because in our series the mean number of passages was two, with a 5.4% incidence of Bethesda category I results. This finding is similar to that reported by Castells et al.26 (5.3%) using a similar methodology. On the other hand, not knowing immediately after puncture whether the material obtained is adequate does not make it easy for the operator to assess the performance of technical variants referring to needle gauge, aspiration technique, etc., or to recognize the usefulness of changes made in needle passage after a first unsuccessful passage. In addition, on-site evaluation of the material allows for real-time diagnostic assessment.
Regarding the possible predictors of a Bethesda category I cytological diagnosis, the most commonly cited factors refer to the characteristics of the nodule. It is well known that small nodules (<10mm), a large cystic, necrotic or fibrous component, or important vascularization, are associated with an increased frequency of samples not adequate for cytological diagnosis.7–9,19,23,29 However, few studies have focused on establishing clinical factors other than purely ultrasound variables or parameters inherent to the puncture-aspiration technique capable of predicting Bethesda category I cytological results in thyroid nodules. Moon et al.20 and Alexander et al.7 identified no clinical predictors. By contrast, Baier et al.21 found a patient age of over 75 years to double the risk of a Bethesda category I result, and they interpreted this in terms of patient neck stiffness that complicated the working position. In our series, a small nodule size, a cystic component, or the vascularization pattern were not predictive of a Bethesda category I result, probably because the ultrasound-guided technique with on-site cytological assessment of the extracted material obviated the difficulties posed by these conditioning factors. However, an older patient age and increased nodule volume were seen to be independently associated with a Bethesda category I result. Since goiter prevalence increases with age30 and the passing of time is accompanied by a gradual increase in nodule size,31 we believe that an older patient age and also a larger nodule volume reflect the presence of an older lesion, and this in turn favors bleeding and necrotic phenomena that finally lead to fibrosis of the nodule, the latter being an acknowledged risk factor for obtaining samples of inadequate quality for cytological diagnosis.8
Our study has some limitations. Its retrospective nature resulted in missing data referring to some variables in some of the patients, and this may have reduced the chances of identifying statistically significant differences. The characteristics of the thyroid treatments and antecedents of neck radiotherapy were not documented. Likewise, interobserver variability in the ultrasound findings or cytological diagnosis was not assessed. The number of patients who underwent surgery was small, as the study only covered a 1-year time period.
In conclusion, ultrasound-guided fine needle aspiration of thyroid nodules with on-site cytological assessment of the extracted material affords both high diagnostic efficacy and a high quality by achieving a very low incidence of Bethesda category I results. It therefore constitutes an alternative to other techniques when the results obtained by the latter are not satisfactory. The issue that needs to be resolved is the collection of samples adequate for cytological diagnosis in older patients and in nodules of greater volume.
Financial supportThe present study received no specific financial support from public agencies, the commercial sector or from non-profit entities.
Authors’ contributionsEach author materially contributed to the investigation and preparation of the manuscript. Specifically: study conception and design, data acquisition and analysis, the interpretation of the results, the drafting of the manuscript and approval of the final version.
Conflicts of interestNone declared.
Please cite this article as: García Pascual L, Surralles ML, Morlius X, González Mínguez C, Viscasillas G, Lao X. Punción-aspiración con aguja fina ecoguiada de nódulos tiroideos con valoración citológica in situ: eficacia diagnóstica, prevalencia y factores predictores de los resultados de categoría Bethesda I. Endocrinol Diabetes Nutr. 2019;66:495–501.