Thyroid cancer may be clinically evident as a tumor mass in the neck or as a histopathological incidental finding after thyroid surgery for an apparent benign condition. Our objective was to assess the differences in clinical signs, surgical management, and course between incidental and clinically diagnosed thyroid tumors.
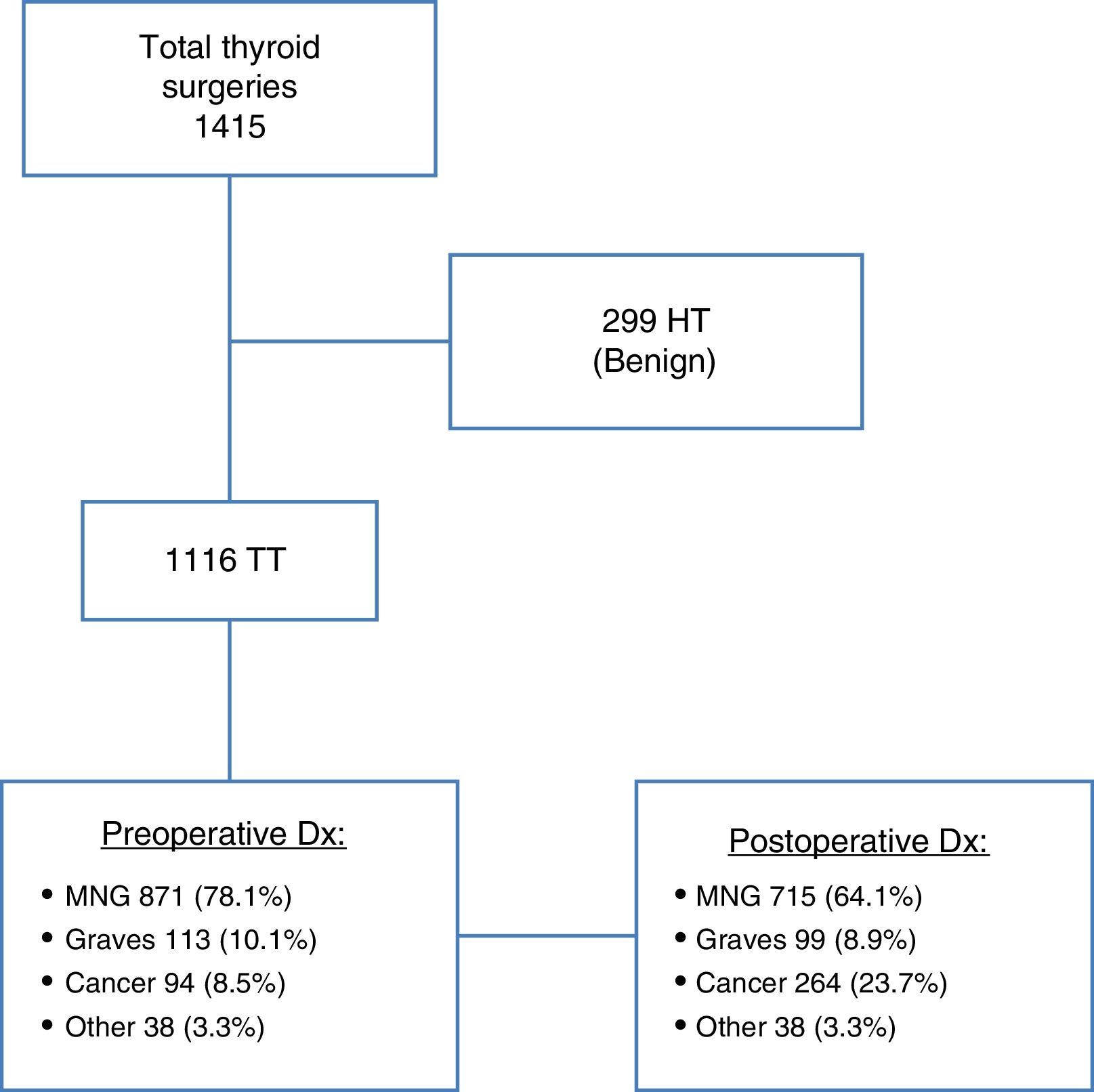
MethodsA retrospective study was conducted on patients operated on for benign or malignant thyroid disease from January 2000 to March 2014. Among the 1415 patients who underwent any thyroid surgery, 264 neoplasms were found, of which 170 were incidental. A comparison was made of incidental versus non-incidental carcinomas. Among incidental carcinomas, cases whose indication for surgery was Graves’ disease were compared to those with multinodular goiter.
ResultsIncidental carcinomas were in earlier stages and required less aggressive surgery. There were no differences in surgical complications between incidental and clinical tumors, but mortality and relapses were markedly higher in non-incidental cancers (4.4% vs 0% and 13.2% vs 4.8% respectively). Carcinomas developing on Graves’ disease showed no differences from all other incidental tumors in terms of complications, mortality, or relapse after surgery.
ConclusionsEarly stage thyroid cancer has better survival and prognosis after surgical treatment.
El cáncer tiroideo puede manifestarse clínicamente por la presencia de un nódulo cervical, o constituir un hallazgo casual en el estudio histológico de la glándula extirpada con diagnóstico, a priori, benigno. El objetivo del presente estudio fue estudiar las diferencias clínicas, de manejo quirúrgico y curso evolutivo entre los tumores tiroideos incidentales y los tumores detectados clínicamente.
Material y métodosEstudio retrospectivo de pacientes intervenidos por enfermedad tiroidea, ya fuese benigna o maligna, en el período comprendido entre enero de 2000 y marzo de 2014. De 1.415 pacientes que se sometieron a algún tipo de cirugía tiroidea se identificaron un total de 264 neoplasias, de las cuales 170 fueron incidentales. Se realizó comparación entre carcinomas incidentales versus no incidentales. Además, entre los incidentales se compararon los casos cuya indicación quirúrgica fue enfermedad de Graves frente a bocio multinodular.
ResultadosLos carcinomas incidentales presentaron estadios más precoces y requirieron cirugía menos agresiva. No se observaron diferencias en las complicaciones quirúrgicas entre ambos grupos, aunque tanto la mortalidad como las tasas de recidiva fueron notablemente mayores en el grupo de no incidentales (4,4% vs 0% y 13,2% vs 4,8% respectivamente). Los carcinomas desarrollados sobre enfermedad de Graves no mostraron diferencias respecto al resto de los tumores incidentales, respecto a complicaciones, mortalidad o recidiva tras la cirugía.
ConclusionesEl cáncer tiroideo en estadios iniciales presenta mayor supervivencia y mejor respuesta al tratamiento quirúrgico.
Incidental thyroid cancer is any malignancy of thyroid origin not detected by clinical examination or in preoperative imaging tests which is found in the pathological study of a surgical specimen excised for an initially benign condition (goiter or hyperthyroidism).1,2 A majority of these lesions are microcarcinomas (papillary tumors less than 1cm in size, according to the definition of the World Health Organization [WHO]), although other types of carcinoma have been reported. The incidence of these lesions ranges from 3% to 16%, with some series reporting incidence rates of up to 25–26%.2,3
Despite the benign course of most microcarcinomas, some studies emphasize the aggressiveness of even some small tumors, which causes the development of metastases, particularly in patients with Graves’ disease and associated cancer.4
The purpose of this study was to determine the differences between incidental and clinically detected tumors in terms of their clinical signs and symptoms, surgical management, and course.
Patients and methodsA retrospective analysis was conducted of patients undergoing surgery for thyroid disease at the general surgery department of our hospital from January 2000 to March 2014. Data were collected from the pathological reports and the clinical history.
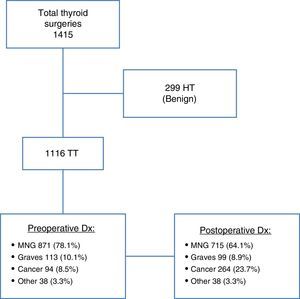
A total of 1415 patients undergoing some type of thyroid surgery were initially identified. Patients who underwent hemithyroidectomy in whom a histological study diagnosed a benign condition (299 patients) were excluded from the analysis. Patients who had undergone total thyroidectomy with a diagnosis of multinodular goiter (MNG), hyperthyroidism, or thyroid cancer were enrolled into the study. In patients with MNG, surgery was indicated based on the size or intrathoracic growth of the goiter, the compression of adjacent structures, or hyperthyroidism. Patients with hyperthyroidism due to Graves’ disease (GD) underwent surgery because of their poor response to treatment with antithyroid drugs, the need for high doses of these drugs, or a recurrence upon treatment discontinuation.5 In non-incidental tumors, a diagnosis of thyroid cancer was based on clinical signs and symptoms, ultrasonography, and cytology after fine needle aspiration (FNA). FNA was performed in nodules greater than 2cm in size, or in smaller tumors if suspected based on ultrasonography, and allowed for preoperative diagnosis in seven cases of microcarcinoma. Patients with a preoperative diagnosis of papillary cancer underwent central lymphadenectomy (due to the clinical or ultrasonographic presence of adenopathies at level VI, or stage T3 and T4 tumors) with/without laterocervical lymphadenectomy based on evidence of metastatic adenopathies. Laryngoscopic examination was performed in all patients before and after surgery by the ORL department. In patients with any recurrent lesion, endoscopic monitoring continued either until the resolution of the problem or until one year after surgery.
A total of 264 neoplasms were identified based on pathological examination of the surgical specimen. Five of these (1.9%) were thyroid tumors not included in the diagnosis of differentiated thyroid carcinoma (4 patients with a diagnosis of medullary cancer and one with anaplastic cancer), and were therefore excluded from the comparative study. The data collected from the patients enrolled into the study included demographic characteristics, pre- and postoperative diagnosis, the initial type of surgery, the stage, the presence of adenopathies at diagnosis, the administration of 131I after initial surgery, postoperative complications (hypoparathyroidism, recurrent nerve injury), related and unrelated mortality, recurrence/persistence, follow-up, and disease-free survival.
The postoperative complications recorded included hypocalcemia and recurrent lesion. Hypocalcemia was defined as ionic calcium levels less than 4.0mg/dL, and was managed according to standard clinical practice at our hospital.6,7 Permanent hypoparathyroidism was defined as that persisting longer than six months. Unilateral or bilateral recurrent nerve injury was assessed clinically and using laryngoscopy, and permanent palsy was defined as that persisting more than one year after surgery.
Statistical analysisQuantitative variables are given as mean±standard deviation or as median (first and third quartile). Qualitative variables are given as absolute and relative frequencies. Comparison between groups was performed using a Chi-square test or a Fisher exact test. All comparisons were two-sided, and a value of p<0.05 was considered statistically significant. Statistical analysis was performed using software SPSS, version 23.0.
ResultsOf the 1415 patients undergoing surgery for thyroid disease, 299 patients in whom hemithyroidectomy was performed with a final benign diagnosis were excluded from the study. All other patients (1166) underwent total thyroidectomy as a one or two-stage procedure. Of these, 871 patients (78.1%) had an initial diagnosis of MNG, while 113 (10.1%) had hyperthyroidism due to GD, and 94 (8.5%) had thyroid cancer. An examination of surgical specimens revealed 170 new cases of carcinoma not previously detected (incidental carcinomas), with 156 tumors found in the 871 patients with preoperative diagnosis of MNG (17.9%), and 14 neoplasms in the 113 patients diagnosed with GD (12.4%). Thyroid cancer was, therefore, found in 264 patients (Fig. 1).
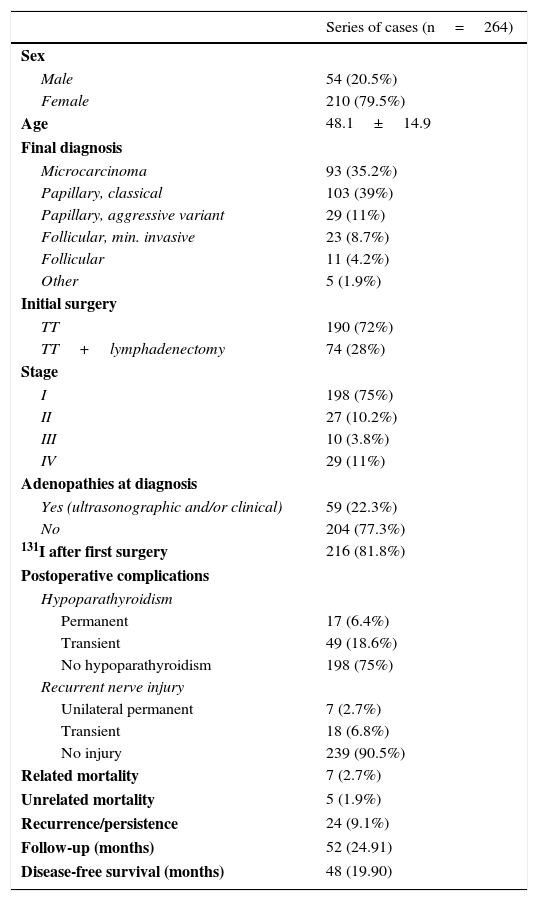
The total sample of 264 patients with a final diagnosis of thyroid cancer consisted of 54 males (20.5%) and 210 females (79.5%) with a mean age of 48.1±14.9 years. The majority of the tumors were microcarcinomas (35.2%) and the classical variant of papillary carcinoma (39%). Twenty-nine patients (11%) were diagnosed with tall-cell carcinoma, a variant more aggressive than classical papillary cancer. Seventy-five percent of patients had stage I cancer, and some type of lymphadenectomy associated with thyroidectomy was performed in 28% of patients. Surgery was associated with the postoperative administration of 131I in 216 patients (81.8%). As regards complications, permanent and transient hypoparathyroidism was found in 6.4% and 18.6% of patients respectively. With regard to recurrent nerve injury, definitive unilateral palsy was found in seven patients (2.7%). No cases of bilateral palsy were recorded. There were seven deaths related to thyroid disease (2.7%), and disease recurrence or persistence occurred in 24 patients (9.1%). Median follow-up was 52 (24.91) months, with a median disease-free survival of 48 (19.90) months (Table 1).
Results of patients enrolled.
| Series of cases (n=264) | |
|---|---|
| Sex | |
| Male | 54 (20.5%) |
| Female | 210 (79.5%) |
| Age | 48.1±14.9 |
| Final diagnosis | |
| Microcarcinoma | 93 (35.2%) |
| Papillary, classical | 103 (39%) |
| Papillary, aggressive variant | 29 (11%) |
| Follicular, min. invasive | 23 (8.7%) |
| Follicular | 11 (4.2%) |
| Other | 5 (1.9%) |
| Initial surgery | |
| TT | 190 (72%) |
| TT+lymphadenectomy | 74 (28%) |
| Stage | |
| I | 198 (75%) |
| II | 27 (10.2%) |
| III | 10 (3.8%) |
| IV | 29 (11%) |
| Adenopathies at diagnosis | |
| Yes (ultrasonographic and/or clinical) | 59 (22.3%) |
| No | 204 (77.3%) |
| 131I after first surgery | 216 (81.8%) |
| Postoperative complications | |
| Hypoparathyroidism | |
| Permanent | 17 (6.4%) |
| Transient | 49 (18.6%) |
| No hypoparathyroidism | 198 (75%) |
| Recurrent nerve injury | |
| Unilateral permanent | 7 (2.7%) |
| Transient | 18 (6.8%) |
| No injury | 239 (90.5%) |
| Related mortality | 7 (2.7%) |
| Unrelated mortality | 5 (1.9%) |
| Recurrence/persistence | 24 (9.1%) |
| Follow-up (months) | 52 (24.91) |
| Disease-free survival (months) | 48 (19.90) |
TT: total thyroidectomy.
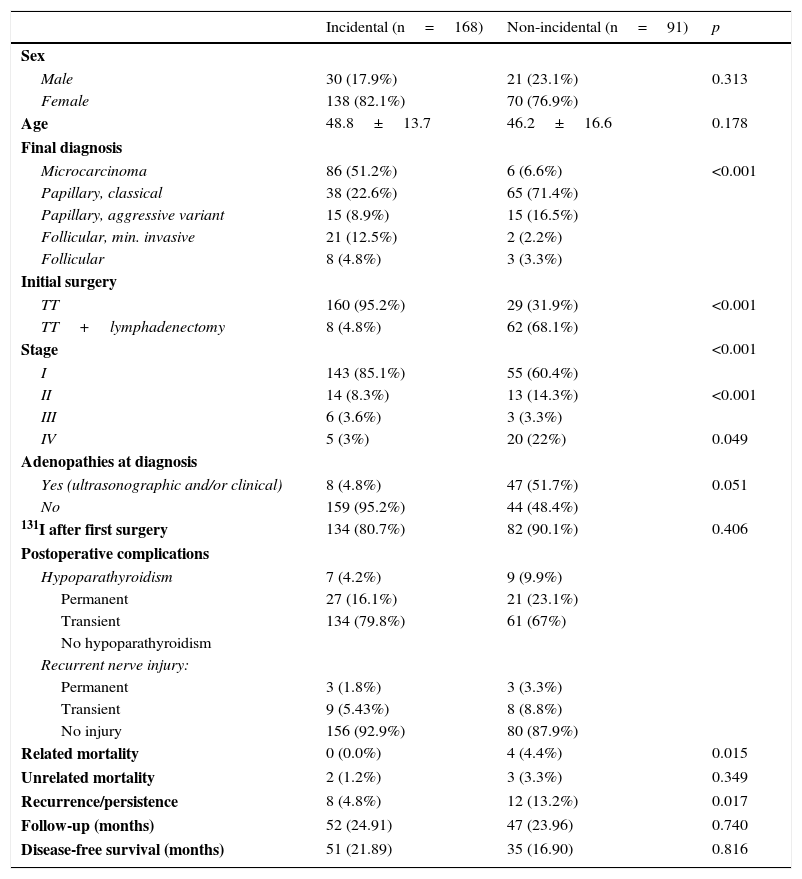
After excluding patients diagnosed with medullary or anaplastic cancer, a comparative study was carried out of patients with incidental (n=168) and non-incidental (n=91) differentiated thyroid cancer. Significant differences were seen in both the final diagnosis (histological type) and stage, with a higher microcarcinoma rate in the group of incidental tumors, 86 (51.2%) vs 6 (6.6%) (p<0.001), and a greater number of stage I tumors, 143 (85.1%) vs 55 (60.4%) (p<0.001). As a consequence, more lymphadenectomies were performed in the group with non-incidental tumors, 8 (4.8%) vs 62 (68.1%) (p<0.001). The distribution of the types of tumor between the two groups also showed a higher rate of follicular (especially minimally invasive) tumors among the incidental tumors. No significant differences were seen between the groups regarding postoperative complications. However, it should be noted that a greater percentage of permanent hypoparathyroidism was found in the group of non-incidental tumors, although the difference was not statistically significant (4.2% vs 9.9%). Recurrence and mortality rates were higher in patients with non-incidental tumors, but the differences did not reach statistical significance (4.8% vs 13.2%, p<0.017; 0% vs 4.4%, p<0.015 respectively) (Table 2).
Comparison of incidental and non-incidental differentiated thyroid tumors.
| Incidental (n=168) | Non-incidental (n=91) | p | |
|---|---|---|---|
| Sex | |||
| Male | 30 (17.9%) | 21 (23.1%) | 0.313 |
| Female | 138 (82.1%) | 70 (76.9%) | |
| Age | 48.8±13.7 | 46.2±16.6 | 0.178 |
| Final diagnosis | |||
| Microcarcinoma | 86 (51.2%) | 6 (6.6%) | <0.001 |
| Papillary, classical | 38 (22.6%) | 65 (71.4%) | |
| Papillary, aggressive variant | 15 (8.9%) | 15 (16.5%) | |
| Follicular, min. invasive | 21 (12.5%) | 2 (2.2%) | |
| Follicular | 8 (4.8%) | 3 (3.3%) | |
| Initial surgery | |||
| TT | 160 (95.2%) | 29 (31.9%) | <0.001 |
| TT+lymphadenectomy | 8 (4.8%) | 62 (68.1%) | |
| Stage | <0.001 | ||
| I | 143 (85.1%) | 55 (60.4%) | |
| II | 14 (8.3%) | 13 (14.3%) | <0.001 |
| III | 6 (3.6%) | 3 (3.3%) | |
| IV | 5 (3%) | 20 (22%) | 0.049 |
| Adenopathies at diagnosis | |||
| Yes (ultrasonographic and/or clinical) | 8 (4.8%) | 47 (51.7%) | 0.051 |
| No | 159 (95.2%) | 44 (48.4%) | |
| 131I after first surgery | 134 (80.7%) | 82 (90.1%) | 0.406 |
| Postoperative complications | |||
| Hypoparathyroidism | 7 (4.2%) | 9 (9.9%) | |
| Permanent | 27 (16.1%) | 21 (23.1%) | |
| Transient | 134 (79.8%) | 61 (67%) | |
| No hypoparathyroidism | |||
| Recurrent nerve injury: | |||
| Permanent | 3 (1.8%) | 3 (3.3%) | |
| Transient | 9 (5.43%) | 8 (8.8%) | |
| No injury | 156 (92.9%) | 80 (87.9%) | |
| Related mortality | 0 (0.0%) | 4 (4.4%) | 0.015 |
| Unrelated mortality | 2 (1.2%) | 3 (3.3%) | 0.349 |
| Recurrence/persistence | 8 (4.8%) | 12 (13.2%) | 0.017 |
| Follow-up (months) | 52 (24.91) | 47 (23.96) | 0.740 |
| Disease-free survival (months) | 51 (21.89) | 35 (16.90) | 0.816 |
TT: total thyroidectomy.
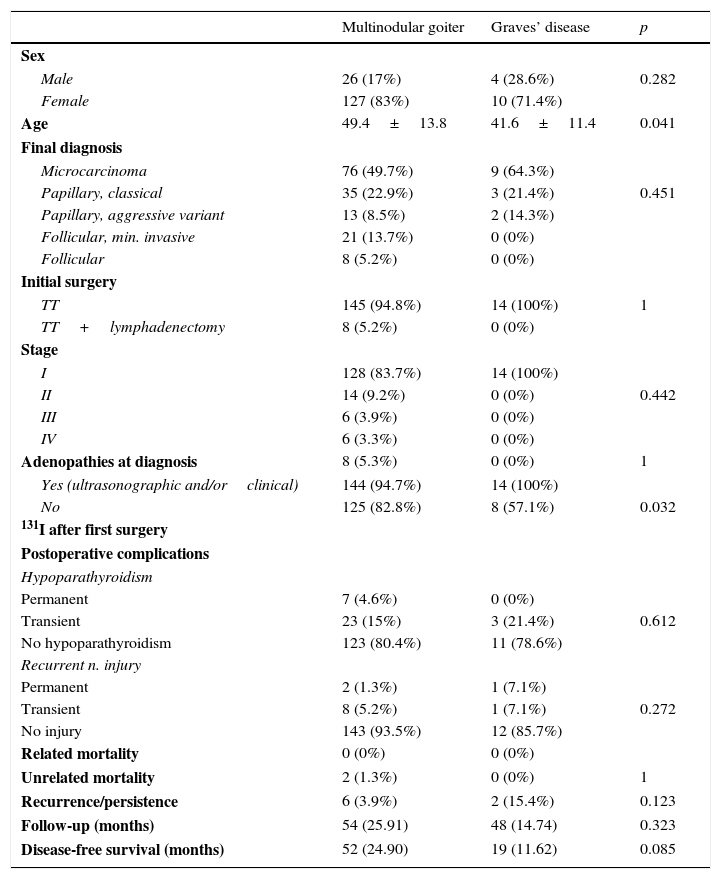
Comparison of the two groups of incidental tumors showed no significant differences as regards the distribution of histological types, complication rates and the number of recurrences, or disease-free survival (Table 3).
Comparison of incidental and non-incidental differentiated thyroid tumors (MNG vs Graves’ disease).
| Multinodular goiter | Graves’ disease | p | |
|---|---|---|---|
| Sex | |||
| Male | 26 (17%) | 4 (28.6%) | 0.282 |
| Female | 127 (83%) | 10 (71.4%) | |
| Age | 49.4±13.8 | 41.6±11.4 | 0.041 |
| Final diagnosis | |||
| Microcarcinoma | 76 (49.7%) | 9 (64.3%) | |
| Papillary, classical | 35 (22.9%) | 3 (21.4%) | 0.451 |
| Papillary, aggressive variant | 13 (8.5%) | 2 (14.3%) | |
| Follicular, min. invasive | 21 (13.7%) | 0 (0%) | |
| Follicular | 8 (5.2%) | 0 (0%) | |
| Initial surgery | |||
| TT | 145 (94.8%) | 14 (100%) | 1 |
| TT+lymphadenectomy | 8 (5.2%) | 0 (0%) | |
| Stage | |||
| I | 128 (83.7%) | 14 (100%) | |
| II | 14 (9.2%) | 0 (0%) | 0.442 |
| III | 6 (3.9%) | 0 (0%) | |
| IV | 6 (3.3%) | 0 (0%) | |
| Adenopathies at diagnosis | 8 (5.3%) | 0 (0%) | 1 |
| Yes (ultrasonographic and/orclinical) | 144 (94.7%) | 14 (100%) | |
| No | 125 (82.8%) | 8 (57.1%) | 0.032 |
| 131I after first surgery | |||
| Postoperative complications | |||
| Hypoparathyroidism | |||
| Permanent | 7 (4.6%) | 0 (0%) | |
| Transient | 23 (15%) | 3 (21.4%) | 0.612 |
| No hypoparathyroidism | 123 (80.4%) | 11 (78.6%) | |
| Recurrent n. injury | |||
| Permanent | 2 (1.3%) | 1 (7.1%) | |
| Transient | 8 (5.2%) | 1 (7.1%) | 0.272 |
| No injury | 143 (93.5%) | 12 (85.7%) | |
| Related mortality | 0 (0%) | 0 (0%) | |
| Unrelated mortality | 2 (1.3%) | 0 (0%) | 1 |
| Recurrence/persistence | 6 (3.9%) | 2 (15.4%) | 0.123 |
| Follow-up (months) | 54 (25.91) | 48 (14.74) | 0.323 |
| Disease-free survival (months) | 52 (24.90) | 19 (11.62) | 0.085 |
TT: total thyroidectomy.
Incidental thyroid cancers are defined as malignant thyroid gland tumors detected in the pathological examination of glands resected based on an initial benign diagnosis. In most of these cases, surgery has been indicated for hyperthyroidism or MNG. The significance of these tumors lies on the one hand in their frequency, and on the other hand in their biological behavior, which is sometimes aggressive.
Hyperthyroidism secondary to GD has traditionally been regarded as a factor protecting against thyroid cancer.8,9 However, an increasing number of studies have reported a non-negligible incidence of occult neoplasms in specimens from thyroidectomy performed for this reason. In this regard, some studies have even speculated about the potential stimulating effect regarding tumor growth of the high levels of anti-TSH receptor antibodies found in these patients.10 For MNG, this incidence is estimated at between 14% and 25% depending on the study. In our series, cancer incidence in pathological specimens was 17.9% for MNG and 12.4% for GD, which agrees with the rates reported in the literature.1,8,9
On the other hand, although some authors have stressed the relatively benign behavior of papillary tumors, regardless of presentation,11 other studies have emphasized the aggressiveness of even small tumors (lymph node metastases), especially in patients with GD and associated cancer.12 We, therefore, decided to conduct this retrospective study to analyze the cases of incidental cancer in our series, to study their incidence, characteristics, and clinical course, and to compare them with patients undergoing surgery with a diagnosis of thyroid carcinoma.
The most common histological diagnosis in incidental thyroid cancer is papillary microcarcinoma, defined by the World Health Organization as papillary thyroid cancer less than 10mm in size. No significant differences exist apparently in this regard between patients who undergo surgery for MNG or for hyperthyroidism.13–17 In our series, no significant difference was found in cancer incidence between patients undergoing surgery for MNG and for hyperthyroidism secondary to GD (17% vs 12.4% respectively). Similarly, there were no differences between the groups regarding histological type, with papillary carcinoma being the most common in both (49% in MNG and 64.3% in GD). Our data agree with those reported in the literature regarding both of these aspects.16 The higher rate of aggressive variants of papillary cancer in patients undergoing surgery for hyperthyroidism should be noted.
As regards the extension of initial surgery, total thyroidectomy was the procedure performed for all incidentalomas, and in 10 patients operated on for MNG, some type of lymphadenectomy was performed for adenopathies found in ultrasonography or during surgery. This finding has already been reported by other authors.13,16 At this point, we would like to stress the importance of selecting an adequate surgical procedure to treat patients with MNG and GD. We agree with other authors that total thyroidectomy is the procedure of choice.18–20 Thyroidectomy may be performed with a low complication rate, decreases recurrence, and facilitates patient follow-up with both radioactive iodine scans and thyroglobulin measurements.2,5,21,22 As regards other prognostic factors (final pathological stage, tumor disease recurrence/persistence rates), no significant differences were found between incidentalomas from the two groups. A small difference was however found in the male:female ratio between tumors related to MNG (1:4) and hyperthyroidism (1:3). The difference was not statistically significant, but should perhaps be borne in mind when male patients with GD are being assessed.
When assessing the clinical significance of incidental cancer, it is important to compare its course with that of cancer diagnosed before surgery. We noted in our series that while papillary cancer was the most common among clinical tumors, the microcarcinoma/carcinoma ratio was reversed for incidentaloma. This implies a greater extent of initial surgery, with a greater lymphadenectomy rate, a more advanced stage, and a higher recurrence rate in non-incidental cancer, with statistically significant figures. It would have been interesting to detail the differences between microcarcinomas diagnosed before surgery and those found incidentally. However, due to the low number of non-incidental microcarcinomas in this series, we decided to consider them globally with all other carcinomas. We also considered it important to compare the rates of specific complications in patients undergoing surgery for benign disease and for cancer. An analysis of the complications occurring in our series showed that the overall rate of permanent recurrent lesion agreed with that reported in the literature.23,24 In addition, no differences in complications were seen between incidental and clinical tumors, or between patients who underwent surgery based on a diagnosis of MNG and GD.
These findings underscore the importance of early diagnosis in thyroid cancer. Clinical tumors and, of course, those showing regional adenopathies at diagnosis, require more radical surgery. Although this study showed no significant differences in surgical complications between patients with incidental and non-incidental tumors, there were differences in the rates of recurrence and disease-related mortality.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: González-Sánchez-Migallón E, Flores-Pastor B, Pérez-Guarinos CV, Miguel-Perelló J, Chaves-Benito A, Illán-Gómez F, et al. Carcinoma de tiroides incidental versus no incidental: presentación clínica, tratamiento quirúrgico y pronóstico. Endocrinol Nutr. 2016;63:475–481.