Chronic intravenous iron administration is often required after bariatric surgery. Oral sucrosomial iron has a particular form of absorption and may represent an alternative treatment.
ObjectiveTo assess the effect of switching to oral sucrosomial iron in patients receiving intravenous iron supplementation after bariatric surgery.
Patients and methodsA case–control study was conducted on 40 women of childbearing age, of whom 20 were switched to oral sucrosomial iron, while 20 patients continued on intravenous iron sucrose every three months.
ResultsNo significant differences were seen in Hb, ferritin, and TSI levels before and after three months of treatment with sucrosomial iron.
ConclusionOral sucrosomial iron could be an alternative in patients who require parenteral treatment with iron after bariatric surgery.
A menudo es necesaria la administración intravenosa crónica de hierro después de la cirugía bariátrica. El hierro sucrosomado oral tiene una forma especial de absorción y es un posible tratamiento alternativo.
ObjectivoValorar el efecto del cambio al hierro sucrosomado oral en los pacientes que reciben suplementos de hierro por vía intravenosa después de cirugía bariátrica.
Pacientes y métodosSe realizó un estudio de casos y controles que incluyó a 40 mujeres en edad fértil, de la que 20 se cambiaron a hierro sucrosomado oral, mientras que las 20 restantes siguieron recibiendo hierro sacarosa cada tres meses.
ResultadosNo se observaron diferencias importantes en los niveles de Hb, ferritina ni TSI hallados antes y después de tres meses de tratamiento con hierro sucrosomado.
ConclusiónEl hierro sucrosomado oral puede ser una alternativa en los pacientes que necesitan tratamiento parenteral con hierro después de cirugía bariátrica.
Obesity is a major public health problem with a very significant economic cost due to its high prevalence and the number and severity of associated comorbidities. Bariatric surgery, whose main objective is sustained weight loss is the most effective treatment for morbid obesity. In addition, the weight reduction achieved after surgery is associated with beneficial effects on blood pressure, lipid profile, sleep apnoea syndrome and type 2 diabetes mellitus.
Nevertheless, all the techniques of bariatric surgery induce a significant reduction in the intake or absorption of nutrients and can therefore be associated with a risk of nutritional deficiency, which is increasing over the years after surgery. Iron is one of the main nutrients which is significantly affected after bariatric surgery. Women of childbearing age are the most vulnerable population and, consequently, they are more prone to develop iron deficiency anaemia. The incidence of iron deficiency and anaemia after bariatric surgery varies according to the type of surgery, time of follow-up and the use of multivitamins supplementation. Iron deficiency anaemia is diagnosed between 10% and 40% of the patients underwent Roux-en-Y gastric bypass (RYGB).1–6
Many patients, especially women who underwent malabsorptive bariatric surgery, require high doses of oral iron supplementation, which are usually associated with gastrointestinal intolerance. Despite of the high doses of oral iron supplements, about 20–30% will fail to achieve optimal levels of haemoglobin and ferritin and will require parenteral therapy with iron.7 The administration of intravenous sucrose iron in regime of day hospital takes between 2 and 3h of stay at the site, for 2 consecutive days, every 3 months. This regimen represents a significant distortion of work and daily life of the patients.
Sucrosomial oral iron might represent an alternative treatment in these patients. Based on a new technology, heme iron is involved into a liposomal membrane. Therefore, the absorption is independent of the conventional oral iron supplements mechanisms (independent of the gastric pH or the duodenum) and it takes place along the whole gastrointestinal tract.
To our knowledge this is the first study that compares the sucrosomial oral iron with intravenous sucrose iron in patients who underwent bariatric surgery and who developed iron deficiency anaemia.
Material and methodsWe have designed a longitudinal nested case–control interventional study including 40 women of childbearing age selected from 130 patients who previously underwent RYGB, and in whom chronic intravenous iron therapy (iron sucrose 300mg every 3 month) was required in regime of day hospital. The patients were recruited from the Morbid Obesity Unit of the Endocrinology Department of the Vall d’Hebron University Hospital. In all these patients intravenous treatment with iron sucrose was indicated because of gastrointestinal intolerance or therapeutic failure despite of receiving high doses of conventional oral iron supplements.
The inclusion criteria were: (a) women who underwent RYGB as treatment for morbid obesity, (b) older than 18 years and childbearing age, (c) stable weight in the previous 6 months, and (d) currently receiving intravenous 300mg sucrose iron every 3 month for iron deficiency anaemia following RYGB. Informed (e) informed consent was obtained from all individual participants included in the study.
The exclusion criteria were: (a) males, (b) physical inactivity, (c) associated pathology (heart failure, chronic obstructive pulmonary disease, ictus squeals, uncontrolled psychiatric disease or eating disorder), (d) surgical techniques for the treatment of obesity, other than RYGB, and (e) other causes of iron deficiency.
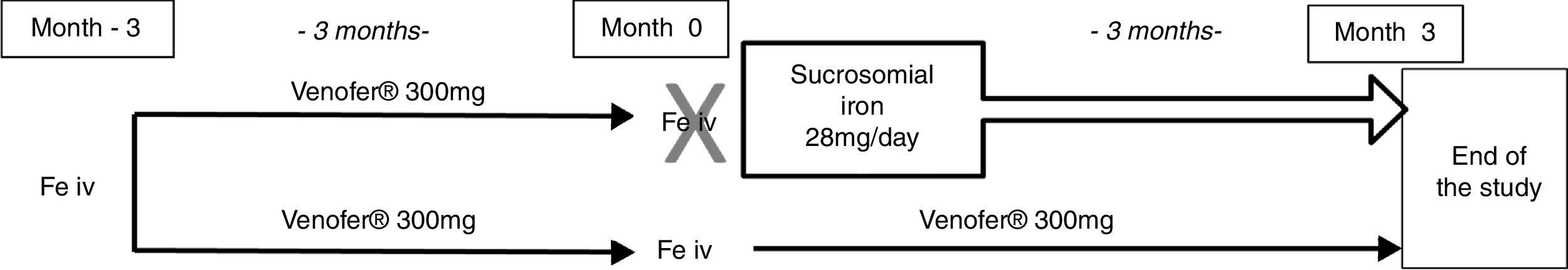
The 40 subjects were allocated to two parallel groups: 20 cases and 20 controls matched by age, previous haemoglobin (Hb) levels, elapsed time after surgery and % of excess weight loss (%EWL). The 20 cases were discontinued from the intravenous iron treatment just before the next scheduled dose and were prescribed sucrosomial oral iron, 28mg/day, for three months. The 20 controls continued with 300mg iron sucrose intravenously every three month, as scheduled. All the patients that were previously prescribed other supplements continued with the same regimen during the study. Total haemoglobin (Hb), ferritin and transferrin saturation index (TSI) were determined before and after three months of treatment in both groups, as well as subjective tolerability (Fig. 1).
The objective of the present study was to evaluate the effect of sucrosomial oral iron to maintain haemoglobin levels after intravenous iron therapy, and to establish a proof of concept. For this purpose, a comparison of total Hb levels and serum parameters related to iron metabolism (ferritin and transferrin saturation index [TSI]) were performed at −3, 0, and 3 months after the treatment. The statistical analysis has performed using SPSS for Windows 20.0.
All procedures in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was registered in ClinicalTrial.gov: NCT 02390921 and in the EU Clinical Trial Register: EudraCT 2015-000297-35.
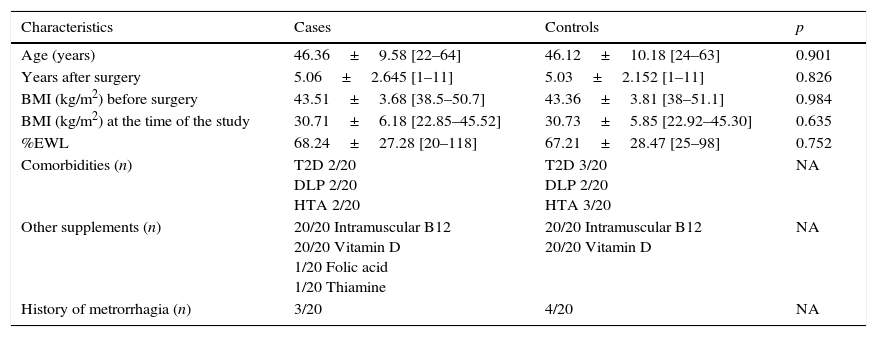
ResultsThe baseline characteristics of the two groups are summarizes in Table 1. The patients in the two groups were matched by age, previous BMI, previous Hb level, %EWL and years after bariatric surgery. It should be noted both at baseline and during the study period there were no significant differences in the menstrual behaviour of the patients.
Baseline characteristics of the patients included in the study.
| Characteristics | Cases | Controls | p |
|---|---|---|---|
| Age (years) | 46.36±9.58 [22–64] | 46.12±10.18 [24–63] | 0.901 |
| Years after surgery | 5.06±2.645 [1–11] | 5.03±2.152 [1–11] | 0.826 |
| BMI (kg/m2) before surgery | 43.51±3.68 [38.5–50.7] | 43.36±3.81 [38–51.1] | 0.984 |
| BMI (kg/m2) at the time of the study | 30.71±6.18 [22.85–45.52] | 30.73±5.85 [22.92–45.30] | 0.635 |
| %EWL | 68.24±27.28 [20–118] | 67.21±28.47 [25–98] | 0.752 |
| Comorbidities (n) | T2D 2/20 DLP 2/20 HTA 2/20 | T2D 3/20 DLP 2/20 HTA 3/20 | NA |
| Other supplements (n) | 20/20 Intramuscular B12 20/20 Vitamin D 1/20 Folic acid 1/20 Thiamine | 20/20 Intramuscular B12 20/20 Vitamin D | NA |
| History of metrorrhagia (n) | 3/20 | 4/20 | NA |
T2D: type 2 diabetes, DLP: dyslipidemia, HTA: arterial hypertension, BMI: body mass index, EWL: excess weight loss.
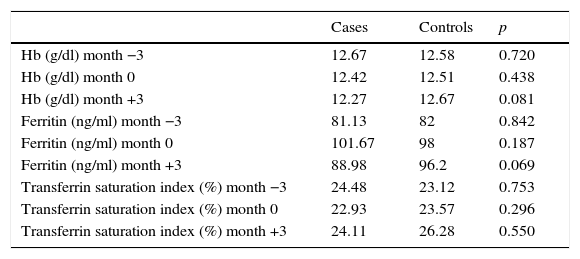
In the group treated with sucrosomial oral iron, no significant differences were seen between the levels of Hb (12.67g/dl±1.06g/dl vs 12,267g/dl±1.35g/dl, p=0.081), ferritin (10,167ng/dl vs 88.89ng/dl, p=0.069) and TSI (24.11% vs 26.28%, p=0.55) before and after the 3 month of treatment. We did not found any adverse effect during this period of time in both groups. Additionally, no differences were seen between the patients treated with sucrosomial iron and the control group at baseline and after 3 month of treatment, as reflected in Table 1.
DiscussionA significant percentage of patients who undergo bariatric surgery, in particular malabsorptive techniques, develop chronic iron deficiency. Most of these patients require intravenous iron supplementation because of gastrointestinal intolerance or therapeutic failure of conventional oral iron supplements.
In our study we have demonstrated that female patients switched from intravenous iron supplementation (300mg sucrose iron every three month) to sucrosomial oral iron (28mg/day), were able to maintain Hb, ferritin and TSI levels after 3 month, with a good tolerability. In addition, no differences were found in the parameters related to iron metabolism between patients treated with intravenous or oral sucrosomial iron (Table 2).
Iron metabolism parameters during the follow-up.
| Cases | Controls | p | |
|---|---|---|---|
| Hb (g/dl) month −3 | 12.67 | 12.58 | 0.720 |
| Hb (g/dl) month 0 | 12.42 | 12.51 | 0.438 |
| Hb (g/dl) month +3 | 12.27 | 12.67 | 0.081 |
| Ferritin (ng/ml) month −3 | 81.13 | 82 | 0.842 |
| Ferritin (ng/ml) month 0 | 101.67 | 98 | 0.187 |
| Ferritin (ng/ml) month +3 | 88.98 | 96.2 | 0.069 |
| Transferrin saturation index (%) month −3 | 24.48 | 23.12 | 0.753 |
| Transferrin saturation index (%) month 0 | 22.93 | 23.57 | 0.296 |
| Transferrin saturation index (%) month +3 | 24.11 | 26.28 | 0.550 |
Although there was a statistically non-significant tendency to lower levels of ferritin in the group treated with sucrosomial iron, the levels were maintained within the normal range for sex and age, and the transferring saturation index was similar between the groups.
This significant incidence of iron deficiency after bariatric surgery is due to the specific modifications of the digestive tract that favour the deficit of iron. The resection of main part of the stomach, with the consequent relative deficit of parietal cells and decreased gastric acid secretion is a primary reason accounting for the impairment of iron absorption. In addition, surgical procedures comprising the exclusion of the duodenum, which is the main place of molecular iron and heme iron absorption, aggravates the situation because the rest of the absorptive surface of the small intestine is not able to compensate the duodenal exclusion. Apart from the impairment of iron absorption due to anatomical modifications, changes in dietary habits such as the intolerance to red meat, which lead to a decrease in its intake, also participate in iron deficiency anaemia after bariatric surgery.8,9
In addition to the causes related to surgery, a significant percentage of obese patients, especially women of childbearing age, present with lower pre-surgery iron deposits. This phenomenon also translates to a great variability in the time of occurrence of the iron deficiency anaemia, from months to years, after the surgery.8 Another factor which contributes to the iron deficiency anaemia following bariatric surgery is the menstrual cycle recovery in the post-operative period. After a 5% loss of total body weight, menstrual irregularities are reduced by almost 40.4%, thus leading to a progressive reduction of iron deposits.10
Sucrosomial oral iron is new method of oral iron supplementation which is independent of the gastric pH or the duodenum, and it takes place along the whole gastrointestinal tract. The bioavailability of sucrosomial oral iron rises to 3.5 times compared with the same dose of conventional oral iron.
The administration of intravenous sucrose iron in regime of day hospital takes between 2 and 3h of stay at the site, depending on the dose, sometimes for 2 consecutive days, periodically. This regimen represents a significant distortion of work and daily life of the patients. By contrast, with sucrosomial oral iron the hospital admission is unnecessary and it represents a less cumbersome and time-consuming treatment which would improve the quality of life of patients with iron deficiency anaemia following bariatric surgery. In addition, it could reduce healthcare costs but specific cost-effective analyses are needed.
To our knowledge, this is the only study that compares the sucrosomial oral iron with intravenous sucrose iron in patients who underwent bariatric surgery. Nevertheless, our study has limitations, such as being an open, non-randomized study, comparing an intravenous therapy with an oral iron supplement. The absence of randomization is justified by the relatively small size of the sample and the need for the two groups to be well matched by age, the % EWL, time after the surgery, and previous Hb levels.
In conclusion, this is a pilot study in which we provide for the first time the usefulness of sucrosomial oral iron supplementation as alternative to iron intravenous administration after bariatric surgery. Our results pave the way to future studies with a larger cohort of patients and with a more prolonged follow-up. In addition, the positive outcomes might serve to design new projects addressed to analyze the pharmacodynamics and pharmacokinetics of sucrosomial oral iron in patients underwent bariatric surgery.
Conflict of interestThe authors declare no conflicts of interest.