In Spain, data suggest that 13.8% of adults have diabetes. Two important aspects in diabetes management are mild hypoglycemic episodes and poor treatment adherence. This study assesses the impact of missed insulin doses and prevalence of mistimed and reduced insulin doses and mild hypoglycemia in patients with type 2 diabetes treated with basal insulin analogues in Spain, and compares the data collected to pooled data from 8 other European countries (OECs).
Materials and methodsGAPP2 was an international, online, cross-sectional study of diabetic patients aged ≥40 years treated with long-acting insulin analogues and their healthcare professionals. Patients and healthcare professionals were recruited from online research panels. Data reported in Spain are compared to pooled data from 8 OECs.
ResultsIn Spain, 1–3% of patients reported they had reduced, missed, or mistimed at least one insulin does in the previous month. Significantly more OEC patients reported dosing irregularities (15–23%; all P<0.01). In Spain, 77% of patients were worried and 59% felt guilty for missing a dose of basal insulin, while 24% reported that they were very worried about nocturnal hypoglycemia. Significantly fewer OEC patients reported worrying (47%; P<0.01) and feeling guilty (37%; P<0.01) about missing an insulin dose, or worry about nocturnal hypoglycemia (12%; P<0.01).
ConclusionsIn Spain, patients with type 2 diabetes report fewer dosing irregularities and hypoglycemic episodes as compared to patients from OECs. However, Spanish patients appear to have a reduced quality of life related to hypoglycemia as well as worry and guilt related to insulin dosing irregularities.
En España, los datos indican que el 13,8% de los adultos tienen diabetes. Dos aspectos importantes del tratamiento de la diabetes son las hipoglucemias leves y la baja adherencia al tratamiento. En este trabajo se evalúa el impacto de las irregularidades de dosificación de insulina (dosis omitidas, administradas fuera de tiempo, y anormalmente reducidas) y de las hipoglucemias leves en los pacientes con diabetes tipo 2 tratados con análogos de la insulina basal en España, en comparación con los datos agrupados de otros 8 países europeos (OEC).
Materiales y métodosGAPP2 fue diseñado como un estudio transversal, internacional, online, para pacientes con diabetes tipo 2 y edad ≥40 años, en tratamiento con análogos de insulina de acción prolongada, y sus profesionales de la salud. Pacientes y profesionales de la salud fueron reclutados a partir de diversos paneles de investigación online. Los datos reportados en España se comparan con los datos agrupados de otros 8 OEC.
ResultadosEn España, el 1–3% de los pacientes informaron que redujeron, olvidaron o se administraron fuera de tiempo al menos una dosis de la insulina en el mes anterior. En comparación, más pacientes OEC denunciaron significativamente irregularidades de dosificación (15–23%). En España, el 77% de los pacientes manifestaron su preocupación y el 59% se sintieron culpables por olvidar una dosis de insulina basal, mientras que el 24% manifestó estar muy preocupado por las hipoglucemias nocturnas. En relación con los pacientes OEC, menos pacientes manifestaron significativamente preocupación (47%) y sentimiento de culpabilidad (37%) sobre la omisión de una dosis de insulina, o inquietud por las hipoglucemias nocturnas (12%).
ConclusionesEn España, los pacientes con diabetes tipo 2 reportan menos irregularidades de dosificación e hipoglucemias en comparación con los pacientes de la OEC. Sin embargo, los pacientes españoles parecen sufrir una reducción de la calidad de vida relacionada con la hipoglucemia, así como preocupación y culpa en relación con las irregularidades en la dosificación de insulina.
European data from 2011 showed that 35 million adults had type 1 or type 2 diabetes and €89 billion were spent in treating and managing diabetes and its complications. This is projected to increase by approximately 23%, to €43 million by 2030.1 In Spain, data suggest that 13.8% of the adult population has diabetes.2 Diabetes, particularly type 2 diabetes, is an increasingly important public health problem,3 from which the estimated costs per patient per year are approximately €1708.4
Type 2 diabetes can cause significant impairment in health-related quality of life.5 Disease complications (e.g. hypoglycaemia, stroke) have been shown to decrease quality of life in patients with type 2 diabetes.6 Finally, there is a strong link between diabetes and depression which is associated with significant morbidity, mortality, and increased healthcare costs.7
Self-treated hypoglycaemia, often referred to as mild hypoglycaemia, remains a key aspect of diabetes management.8,9 Mild hypoglycaemia is common, affecting approximately a third of patients using insulin analogues. They are associated with a reduction in patient well-being and functioning10 and have substantial economic consequences, with lost productivity estimated to cost from $15.26 to $93.47 per episode.10 Mild hypoglycaemic episodes may precede or predispose to severe episodes where patients cannot treat themselves.11,12
There is also growing evidence poor adherence to insulin in type 2 diabetes patients results in inadequate glucose control13,14 and increased mortality.15 Dosing irregularities (including missed, mistimed by >2h and reduced doses) of basal insulin have been shown to be common in type 2 diabetes patients and may negatively impact diabetes management.16
Therefore, the impact of self-treated hypoglycaemia and dosing irregularities in type 2 diabetes patients requires further investigation. The GAPP2 (Global Attitude of Patients and Physicians) survey was designed to improve our understanding of these two issues. This survey was initially conducted in six countries (USA, Canada, Japan, Germany, UK and Denmark),12,16 and was extended to a total of 17 countries in Europe (including Spain), North America, Asia, Africa and Australasia.
MethodsStudy design, setting and data handlingThe GAPP2 survey was a multinational online, cross-sectional study of type 2 diabetes patients using insulin analogues and of healthcare professionals (HCPs) managing type 2 diabetes. The survey was conducted in 17 countries in Europe, North America, Asia, Africa and Australasia. This manuscript reports data from Spain, with comparisons against pooled data from eight other European countries (Czech Republic, Denmark, France, Germany, Israel, Russia, Sweden and UK), which will be referred to as ‘Other European Countries’ (OECs).
The methodology was implemented across all countries. Further details of the global methodology have been previously published.12,16 Questions were generated from multiple data sources: an international steering committee of clinical experts, current literature and key concepts raised from transcripts of nine previously conducted focus groups and interviews with diabetes patients.
Patient and HCP questionnaires were structured to allow between-population comparisons. Questionnaires contain demographics and background information on diabetes management, self-treated hypoglycaemia, patient functioning and well-being. To minimise recall bias on patient responses, reporting was focused on events occurring during the 30 days prior to participation in the survey. Respondents were offered an “I don’t know” answer where applicable to avoid generating inaccurate responses, all data were logic tested to ensure respondents did not provide contradictory answers. Data identified electronically as being incomplete were collected but not processed to be included in the analyses. Response data were stored in compliance with the UK Data Protection Act (1998) on secure servers that could be accessed only by relevant researchers. Each respondent was issued with a unique Uniform Resource Locator (URL) that could be used once to access the questionnaire.
Pilot testPrior to the full launch, both surveys were pilot tested in a two-step process. First, they were cognitively debriefed to ensure comprehension and readability by three HCPs and five patients in each country. A limited number of respondents were also invited to complete each survey (50–100 per country) and after the first 10 completed surveys, the data and survey mechanism logic were tested.
ParticipantsHealthcare professionals and patients were recruited from pre-existing online research panels where members had registered to participate in research surveys. Panels were composed of a representative sample of the online population so as not to bias the sample, and were recruited from a broad array of online and offline approaches that best represented the country's online community.
HCP respondents were initially targeted by specialty, incentives ranging from £25 to £45 were offered. Participants were required to see a minimum number of type 2 diabetes patients in a typical month: in Spain, this was 20 patients per month for general practitioners (GPs) or 40 patients per month for specialists. For OEC, France, Sweden and UK required GPs to see 20 patients/month or 40 patients/month for specialists. Denmark and Germany required GPs to see five patients/month or 40 patients/month for specialists. Israeli GPs were required to see 40 patients/month and specialists 60 patients/month. Czech Republic and Russia specialists were required to see 40 patients/month and GPs were excluded.
Patient respondents were recruited from general population research panels and were initially contacted on the basis of having type 2 diabetes and being aged ≥40 years. Incentives were offered (often non-monetary) in line with terms and conditions of the panels. Participants were required to be on long-acting basal insulin (alone) or a combination of long-acting basal and short-acting bolus insulin taken separately (basal-bolus), with or without oral agents. Those on bolus only, premix or using insulin pumps were excluded.
Statistical analysisData were initially descriptively analysed using paired t-tests and Pearson's Chi square test as appropriate. Where notable numbers of outliers were seen to be affecting the results for a given question, that question was assessed subjectively, and responses outside the statistically acceptable range not deemed plausible in the context of the question were removed.
ResultsParticipantsIn Spain, 39,250 patients were invited to participate, 9685 responded and were screened, producing 305 eligible responders who completed the survey. The response rate was higher in Spain than in the global response rate as previously reported (24.6% vs 9.8%).12,16 For the HCP survey 1515 were invited to participate, 431 responded and were screened, producing 211 eligible respondents who completed the survey. Data are presented for 305 Spanish type 2 diabetes patients taking insulin analogues and 211 Spanish HCPs who prescribe insulin treatment (prescribers) for type 2 diabetes patients.
Where applicable, the Spanish data are compared with a pooled data from OEC (Other European Countries data from Czech Republic, Denmark, France, Germany, Israel, Russia, Sweden and UK). OEC data are based on 1424 completed surveys from type 2 diabetes patients taking insulin analogues and 1261 completed surveys from prescribers.
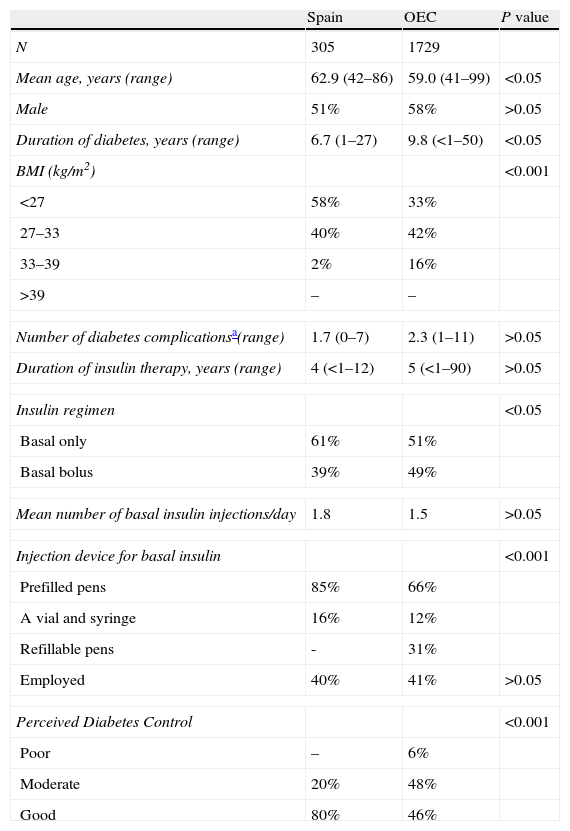
Patient demographicsThe mean age of the Spanish cohort was significantly older compared to OEC (62.9 years vs 59 years; P<0.05; Table 1). Compared to OEC, Spanish respondents had been a shorter duration of diabetes (6.7 vs 9.8 years; P<0.05); significantly lower BMI (P<0.05); most used prefilled pens to deliver their insulin (P<0.001) and felt they had good control of their diabetes (P<0.001). The Spanish cohort was similar in most other respects to the OEC population.
Patient demographics.
| Spain | OEC | P value | |
| N | 305 | 1729 | |
| Mean age, years (range) | 62.9 (42–86) | 59.0 (41–99) | <0.05 |
| Male | 51% | 58% | >0.05 |
| Duration of diabetes, years (range) | 6.7 (1–27) | 9.8 (<1–50) | <0.05 |
| BMI (kg/m2) | <0.001 | ||
| <27 | 58% | 33% | |
| 27–33 | 40% | 42% | |
| 33–39 | 2% | 16% | |
| >39 | – | – | |
| Number of diabetes complicationsa(range) | 1.7 (0–7) | 2.3 (1–11) | >0.05 |
| Duration of insulin therapy, years (range) | 4 (<1–12) | 5 (<1–90) | >0.05 |
| Insulin regimen | <0.05 | ||
| Basal only | 61% | 51% | |
| Basal bolus | 39% | 49% | |
| Mean number of basal insulin injections/day | 1.8 | 1.5 | >0.05 |
| Injection device for basal insulin | <0.001 | ||
| Prefilled pens | 85% | 66% | |
| A vial and syringe | 16% | 12% | |
| Refillable pens | - | 31% | |
| Employed | 40% | 41% | >0.05 |
| Perceived Diabetes Control | <0.001 | ||
| Poor | – | 6% | |
| Moderate | 20% | 48% | |
| Good | 80% | 46% | |
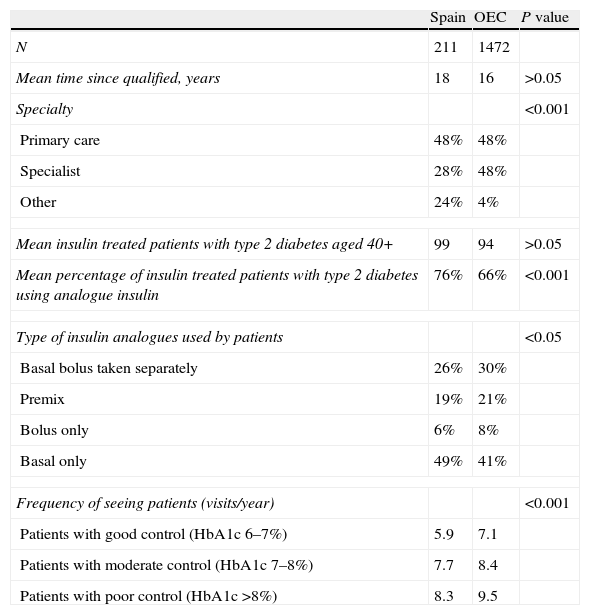
There were significantly fewer Spanish specialists compared to OEC (P<0.001; Table 2) and but Spanish prescribers saw significantly more patients with type 2 diabetes per month (76% vs 66%; P<0.001). Compared to OEC, Spanish prescribers also saw patients on fewer occasions per year (P<0.001). The Spanish cohort was similar in most other respects to the OEC population.
Prescriber demographics.
| Spain | OEC | P value | |
| N | 211 | 1472 | |
| Mean time since qualified, years | 18 | 16 | >0.05 |
| Specialty | <0.001 | ||
| Primary care | 48% | 48% | |
| Specialist | 28% | 48% | |
| Other | 24% | 4% | |
| Mean insulin treated patients with type 2 diabetes aged 40+ | 99 | 94 | >0.05 |
| Mean percentage of insulin treated patients with type 2 diabetes using analogue insulin | 76% | 66% | <0.001 |
| Type of insulin analogues used by patients | <0.05 | ||
| Basal bolus taken separately | 26% | 30% | |
| Premix | 19% | 21% | |
| Bolus only | 6% | 8% | |
| Basal only | 49% | 41% | |
| Frequency of seeing patients (visits/year) | <0.001 | ||
| Patients with good control (HbA1c 6–7%) | 5.9 | 7.1 | |
| Patients with moderate control (HbA1c 7–8%) | 7.7 | 8.4 | |
| Patients with poor control (HbA1c >8%) | 8.3 | 9.5 | |
When asked about the last time they dosed their insulin irregularly, the percentage of Spanish patients who missed, mistimed and reduced doses in the past 30 days was 1% (mean occasions 1.0), 3% (mean 2.3) and 1% (mean 1.0) respectively. Of those who had dosed irregularly the percentage of intentional dosing irregularities were reported as 31% missed, 40% mistimed and 64% reduced. The last time they intentionally missed, mistimed or reduced a dose the main reasons were reducing risk of hypoglycaemia (91%, 67% and 60% respectively) or because their blood sugar was too low (80%, 67% and 60% respectively). Seventy one per cent recognised that missing basal doses would negatively impact their health and 73% discussed dosing irregularities with their doctors.
The frequency of insulin dosing irregularities with clinical impact was reported by Spanish prescribers as 4.3, 6.2 and 5.5 for missed, mistimed and reduced doses.
OEC dosing irregularitiesCompared to Spanish patients a higher proportion of OEC patients reported dosing irregularities in the past 30 days missed (16% (P<0.001); mean 2.3 (P<0.001); mistimed 24% (P<0.001); mean 3.6; reduced 15% (P<0.001); mean 3.6 (P<0.001)). A smaller proportion reported intentional missed (10%; P<0.001) and mistimed (26%; P<0.001) doses and a similar proportion reported intentional reduced doses (67%) compared to Spanish patients. A smaller proportion also reported intentionally missing or mistiming a dose to reduce their risk of hypoglycaemia (missing 37% P<0.001; mistimed 26% P<0.001) or because their blood sugar was too low (missed 28% P<0.001; mis-timed 24%; P<0.001) compared to Spanish patients. A smaller proportion of OEC patients both recognised missing basal doses would negatively impact their health (65%; P<0.05) and discussed dosing irregularities with their doctors (66%; P<0.05) compared to Spanish patients.
OEC prescribers reported the frequency of insulin dosing irregularities with clinical impact at a similar level (missed 4.1; mis-timed 5.8; reduced 5.2).
Self-treated hypoglycaemiaSpanish self-treated hypoglycaemiaIn the past 30 days, 10% of Spanish patients reported self-treated hypoglycaemia, of which 12% were nocturnal episodes and none reporting five or more episodes in that time. In response to a self-treated hypoglycaemic episode, 26% missed, 22% mistimed and 22% reduced a dose. Thirteen per cent reported they intentionally let their blood sugar go high to avoid a self-treated hypoglycaemic episode.
Nineteen per cent of Spanish prescribers reported discussing hypoglycaemia most or all of the time with patients, and 13% reported patients do not see hypoglycaemia as an important issue.
OEC self-treated hypoglycaemiaIn the past 30 days, a higher proportion of OEC patients (33%; P<0.001) reported self-treated hypoglycaemia and a similar proportion (11%) were nocturnal episodes, 14% (P<0.001) reported having five or more episodes in that time. A smaller proportion reported after the last time they had a self-treated hypoglycaemic episode they missed (5%; P<0.001), mistimed (6%; P<0.001) and reduced a dose (8%; P<0.001). A higher proportion (21%; P<0.05) reported they intentionally let their blood sugar go high to avoid a self-treated hypoglycaemic episode.
A similar proportion of OEC prescribers reported discussing hypoglycaemia most or all of the time (23%), but a higher proportion reported patients do not see hypoglycaemia as an important issue (25%; P<0.05).
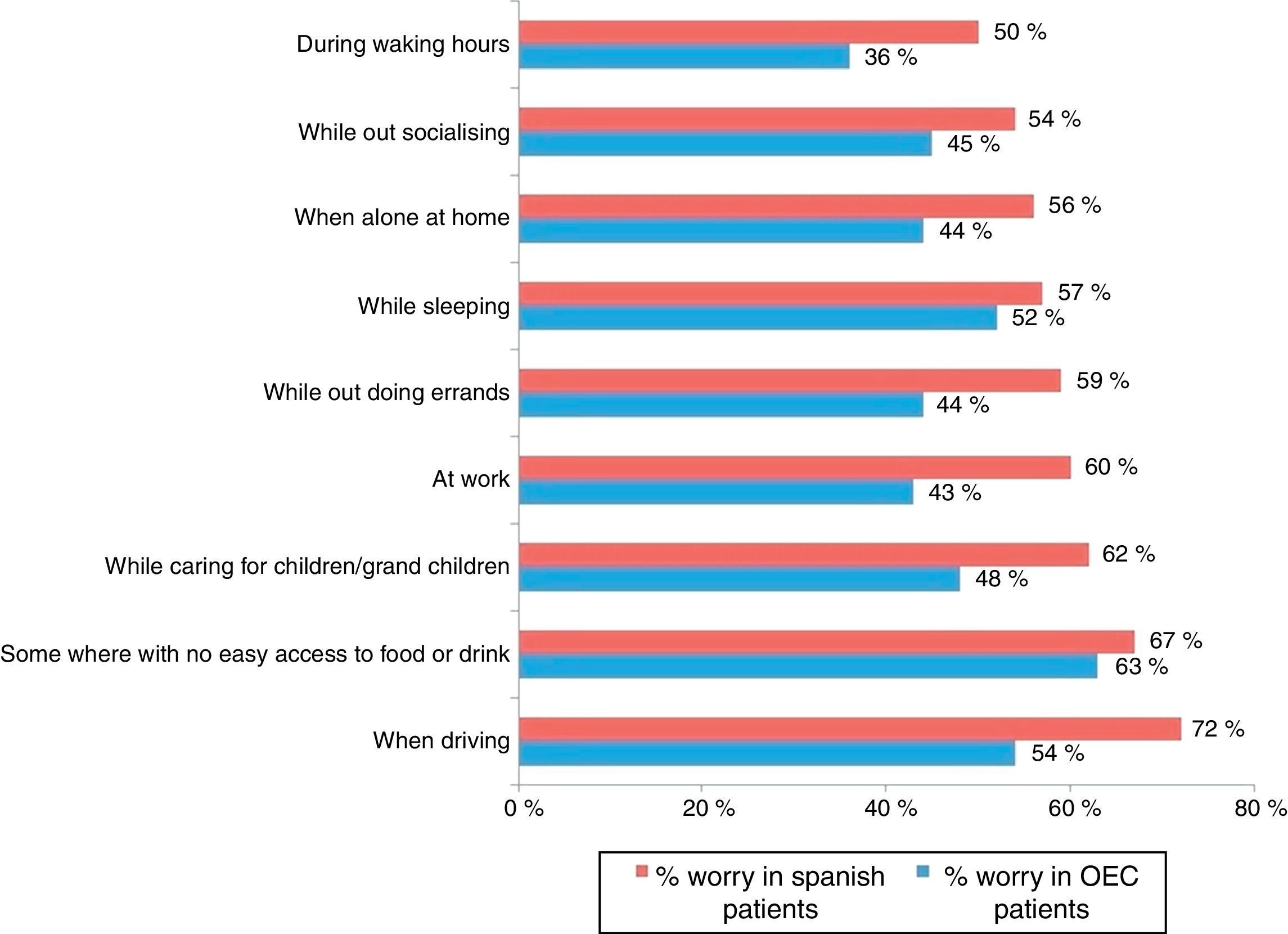
Patient guilt and worrySpanish guilt and worrySeventy-seven per cent of Spanish patients would worry and 59% would feel guilty about missing a dose of basal insulin. Twenty four per cent reported being very worried about nocturnal self-treated hypoglycaemia. In everyday situations, Spanish patients reported worry about self-treated hypoglycaemia (Fig. 1).
When asked about the convenience of their insulin regime, 48% of Spanish patients find it convenient to take their insulin at the same time every day. Patients reported taking their basal insulin at the same time inconvenient because they ‘can’t remember to take it with them’ (13%).
OEC guilt and worryA smaller proportion of OEC patients reported being worried (47%; P<0.001) and feeling guilty (37%; P<0.001) about missing a dose of basal insulin and being worried about nocturnal self-treated hypoglycaemia (12%; P<0.05). In everyday situations, OEC patients also reported less worry about self-treated hypoglycaemia (Fig. 1).
A larger proportion finds it convenient to take their insulin at the same time every day (60%; P<0.05). A larger proportion report they find taking their basal insulin at the same time inconvenient because they ‘can’t remember to take it with them’ (43%; P<0.001).
DiscussionDosing irregularitiesSpanish patients reported significantly lower proportion of dosing irregularities (missed, mistimed, reduced) compared to OEC patients in the previous 30 days. The low numbers of dosing irregularities by Spanish patients is encouraging and an important finding for diabetes management in Spain as insulin non-adherence is a significant predictor of elevated HbA1c14 and an independent risk factor for mortality.15 One possible reason may be that Spanish patients had significantly shorter disease duration (6.7 years vs. 9.8 years OEC; P<0.05, Table 1) indicating less advanced disease and a greater desire for tighter control.
While fewer dosing irregularities were reported in Spain, reports of intentional missed and mistimed doses are significantly higher. The consistent reporting of reasons for intentional dosing irregularities (reducing hypoglycaemia risk or blood sugar being too low) indicates room for improvement. Patients reporting missing or mistiming a dose largely because of concerns about blood sugar suggest that glycaemic control may be suboptimal. Reports of dosing irregularities occurring to reduce the risk of hypoglycaemia indicate a possible fear of hypoglycaemia.
It is positive that more Spanish patients discussed dosing irregularities with their doctor compared to OEC and that more Spanish patients recognised that missing doses would negatively impact their health. Physician communication and awareness of the negative effects of dosing irregularities by Spanish patients suggest a possible link between communication and dosing irregularities, and physicians should be aware of this aspect of treatment.
Self-treated hypoglycaemiaAs with dosing irregularities a significantly lower proportion of Spanish patients reported self-treated hypoglycaemia in the past 30 days compared to OEC, with similar levels of dosing irregularities being nocturnal. Interestingly, no Spanish patients reported having five or more events in the past 30 days, which was significantly lower than OEC patients, indicating that insulin titration may be more progressive in Spanish patients. However, of those Spanish patients who suffered a hypoglycaemic event, approximately a quarter reported a subsequent dosing irregularity, indicating that while self-treated hypoglycaemia is less frequent it may have higher negative effects on Spanish patients.
As discussed above, the intentional dosing irregularities were often to reduce the risk of hypoglycaemia indicating a persistent fear of hypoglycaemia. Fear of hypoglycaemia can limit the ability of diabetes medications to achieve and maintain optimal glycaemic control.17 Patients should therefore be encouraged to discuss hypoglycaemia with their prescriber.
Patient guilt and worryThe proportion of dosing irregularities reported by Spanish patients are consistent with the levels of worry and guilt reported, indicating they are concerned with potential dosing irregularities. A higher proportion of Spanish patients also worry about self-treated hypoglycaemia in daily situations, particularly nocturnal hypoglycaemia. These data demonstrate while it is positive that dosing irregularities are low in Spanish patients, they may be paying a high cost for them. Prescribers should seek to alleviate patient concerns by increasing communication as well as discussing the worries patients have about all aspects of their disease.
LimitationsThis survey focused on insulin analogue users rather than NPH insulin, therefore removing a significant proportion of patients from consideration. However, among the healthcare professionals surveyed in GAPP2, when asked about their views on these two different types of insulin there was general consensus on the benefits of insulin analogues particularly in terms of reduction of hypoglycaemia risk. Participants (both healthcare professionals and patients) were recruited from pre-existing online research panels where members had registered to participate in research surveys. This is a potential bias to the survey as it selects only those who are currently registered with the panels. However, the panels are designed to be a representative sample to limit any potential bias, and were recruited from a broad array of online and offline approaches that best represented the country's online community. While the response rate may initially be perceived as low and may be a limiting factor in the survey they are higher than the global GAPP2 response rates which have previously been reported.12,16
GAPP2 was a web-based survey and hence selected for respondents with internet access. Although the internet is widely available in Spain, this may have led to over-representation of younger patients, those in employment and those living in non-isolated situations. The study was based on self-reports of relevant dosing irregularities and self-treated hypoglycaemic events. Hence, recall bias and between-country differences in under- or over-reporting cannot be ruled out.
ConclusionsSpanish patients appear to have fewer dosing irregularities and hypoglycaemia episodes compared to patients from OEC explained at least in part by their shorter disease duration. However, Spanish patients report increased worry and guilt related to dosing irregularities. While prescribers must keep up basic diabetes education and discuss the importance of insulin adherence for reducing adverse outcomes, they must also help alleviate the worry and guilt of their patients when insulin is initiated, including the fear of hypoglycaemia, which may be significant. Patients must be encouraged to freely discuss their fears and concerns with their prescribers. Finally, prescribers should help patients in reducing insulin dosing irregularities that may result in improving glycaemic control while avoiding excessive hypoglycaemia episodes.
Conflicts of interestF. Javier Ampudia-Blasco is a member of a Novo Nordisk national advisory board. Manual Galan is an employee of Novo Nordisk who funded this study. Meryl Brod has consulted for Forest, Genetech, Bayer, Novo Nordisk and Abbvie.
The GAPP2 study was funded by Novo Nordisk A/S. The sponsor's role was to appoint an independent medical communications company (FTI Consulting) and research company (Bryter Research).