Diabetic ketoacidosis (DKA) is the most severe acute metabolic complication of type 1 diabetes mellitus. Insulin treatment is commonly guided by plasma glucose levels and changes in venous blood gases, while β-hydroxybutyrate (BHB) levels are rarely measured. The study objective was to evaluate the value of capillary BHB monitoring in the course and resolution of DKA.
Patients and methodsThirty patients with type 1 diabetes admitted for DKA were enrolled. A standard protocol including monitoring of blood glucose, venous blood gases, semiquantitative ketonuria, and capillary BHB was used. Patients were divided into three groups by time to DKA resolution (group 1: <24h, group 2: 24–48h, group 3: >48h), and BHB results were compared to all other biochemical measurements.
ResultsMean laboratory results upon admission were: blood glucose 415 (standard deviation [SD] 106)mg/dl; bicarbonate 9.6 (SD 1.5)mmol/l; pH 7.13 (SD 0.04); BHB 4.33 (SD 0.48)mmol/l, and ketonuria 3+ in 22 patients and 4+ in 6. BHB correlated well with bicarbonate (r=−0.24139; P=0.0161) and pH (r=−0.56419; P<0.0001). BHB normalized earlier than ketonuria in all cases (group 1: 15.5 vs 18.8h, P<0.05; group 2: 18.2 vs 23.5h, P<0.01; group 3: 37.3 vs 41.7h, P<0.01). Ten percent of the patients still had ketonuria when blood ketone levels were already normal (<0.5mmol/l).
ConclusionBHB measurement is an easy, practical, and reliable monitoring method in DKA and may be used as a parameter to adjust insulin treatment.
La cetoacidosis diabética (CAD) es la complicación aguda más grave de la diabetes mellitus tipo 1. Su tratamiento con insulina viene guiado por los valores obtenidos en las determinaciones de glucemia y los cambios gasométricos, mientras que los niveles de beta-hidroxibutirato (BHB) raramente son determinados. El objetivo del estudio fue evaluar la utilidad de la monitorización de BHB capilar en el curso y resolución de una CAD.
Pacientes y métodosSe estudiaron 30 pacientes diabéticos tipo 1 con CAD a los que se les aplicó un protocolo estándar, con monitorización de glucosa y gasometría venosas, cetonuria semicuantitativa y BHB capilar. Para el seguimiento se establecieron a priori tres grupos de acuerdo con el tiempo de recuperación según criterios bioquímicos (grupo 1: < 24h; grupo 2: 24–48h; grupo 3: > 48h) y se correlacionaron las mediciones de BHB con el resto de determinaciones.
ResultadosInicialmente la media de la glucemia fue de 415 (desviación estándar [DE]: 106)mg/dl; bicarbonato 9,6 mmol/l (DE: 1,5); pH 7,13 (DE: 0,04); β-OHB 4,33 mmol/l (DE: 0,48) y la cetonuria fue de 3+ en 22 y 4+ en 6 casos. Los valores de BHB se correlacionaron con los de bicarbonato (r=-0,24139; p=0,0161) y con el pH (r=-0,56419; p<0,0001). El BHB alcanzó valores normales en todos los grupos antes que los de la cetonuria (grupo 1: 15,5 frente a 18,8 horas, p<0,05; grupo 2: 18,2 frente a 23,5 horas, p<0,01; grupo 3: 37,3 frente a 41,7 horas, p<0,01). El 10% de los pacientes presentaban cetonurias positivas cuando la cetonemia ya se había normalizado (< 0,5 mmol/l).
ConclusiónLa determinación de BHB es un método sencillo, práctico y fiable para la monitorización de la CAD y puede ser utilizado como parámetro para el ajuste del tratamiento con insulina.
Diabetic ketoacidosis (DKA) is an acute and highly life-threatening complication, with a persistent annual incidence of about 12 episodes per 100,000 inhabitants and year.1 A delay in the diagnosis and treatment of DKA is associated with a significant increase in patient morbidity and mortality, which in the industrialized world is estimated to represent 3–4% of the global episodes. DKA is secondary to an absolute or relative insulin deficit, giving rise to intense lipolysis with the release of large amounts of free fatty acids and hepatic overproduction of acetyl coenzyme A, acting as substrate for the liver production of ketone bodies.2 Beta-hydroxybutyrate (BHB) is the main ketone body produced in DKA, and the BHB/acetoacetate ratio may reach 10:1.3 Conventional ketone body testing based on reaction with nitroprussiate is the standard technique for detection in urine, but has important limitations such as the fact that it offers only a semiquantitative estimate of the acetoacetate and acetone levels. This test may underestimate the severity of DKA, and on the other hand may continue to yield positive readings after the episode has been resolved.4 In recent years it has become possible to measure BHB in capillary blood using a reactive strip as a rapid and precise method for the detection of ketonemia.5,6 This test has demonstrated its usefulness in the diagnosis of different situations of worsened blood glucose control, such as ketosis7,8 and ketoacidosis.9 The aim of the present study was to establish the usefulness of capillary BHB measurement in the management of DKA in the hospital setting.
Patients and methodsPatients and study protocolThe patients included in the study presented type 1 diabetes mellitus, and all were over 18 years of age and were seen in some of the three participating Spanish hospitals (Hospital Vall d’Hebrón in Barcelona, Complejo Hospitalario Universitario in Santiago de Compostela, and Hospital Universitario Insular in Las Palmas), where they reported to the emergency service due to ketoacidotic decompensation. The ethical principles of the Declaration of Helsinki were followed, and the study was approved by the corresponding clinical research ethics committees. All patients gave written informed consent to participate in the study. The inclusion criterion was admission due to DKA and compliance with the biochemical criteria of the American Diabetes Association10 (blood glucose>250mg/dl; pH<7.30; bicarbonate<15mequiv./l, and moderate ketonuria and/or ketonemia).
The exclusion criteria were pregnancy or the coexistence of diseases capable of interfering with the study variables. Thirty patients were included, and each center applied a specific treatment protocol based on the intravenous administration of fast-acting insulin, with the purpose of reducing the hyperglycemia at a rate of 100mg/(dlh), followed by subcutaneous administration once the blood glucose levels were normalized. Fluid replacement was carried out with intravenous saline (0.9%), 1l in the first 30min, followed by 1l every 2h until medical criterion decided a switch to dextrose – with suspension after biochemical normalization. DKA resolution was defined when three of the following four criteria were met11: blood glucose<200mg/dl, bicarbonate≥18mequiv./l, pH>7.3 and anion gap≤2mequiv./l.
The clinical characteristics and DKA triggering factors were evaluated in each case. Likewise, evaluation was made of the clinical and laboratory test parameters during treatment and of the time to normalization of ketonemia versus ketonuria. The biochemical values (blood glucose, bicarbonate and pH) were monitored at baseline, periodically (every 2h), and at DKA resolution. Follow-up was carried out until the patient left the emergency or critical care unit, and for a maximum of 48h.
In addition, the professionals attending the patients received a satisfaction questionnaire addressing both methods for the measurement of ketosis, in which at the end of the treatment of ketoacidosis they were asked to answer the question: In your opinion, which is the most convenient, practical and reliable method?
Biochemical determinationsPlasma glucose was determined by means of the glucose oxidase method. Capillary blood glucose in turn was determined using a glycometer (MediSense Optium™; MediSense/Abbott Laboratories, Abington, United Kingdom). This system measures glucose and BHB using specific strips for each parameter. Five μl of capillary blood are needed. BHB in the presence of hydroxybutyrate dehydrogenase is oxidized to acetoacetate, with the concomitant reduction of NAD+ to NADH. NADH is reoxidized to NAD+ via a redox mediator, so that the current generated is directly proportional to the BHB concentration. The system is valid for concentrations of 0–6mmol/l and in three different levels of BHB (low up to 0.5; moderate up to 1.08; and high up to 3.55). The within-test coefficients of variation (calculated in three determinations for each sample) were 10.5%, 5.5% and 3.2%, respectively.12 Ketone bodies in urine were measured with reactive strips using a semiquantitative method (Ketodiastix, Bayer Diagnostics, Stoge Poges, United Kingdom). Ketosis was defined by ≥0.5mmol/l in capillary blood10 or positivity for ketonuria.11
Statistical studyThe statistical analyses were made by the investigating team and by an independent statistician. The SAS version 9.1 statistical package was used. Qualitative variables were reported as the frequencies and percentages of occurrence of each of the values. Quantitative variables in turn were presented as the mean, standard deviation (SD) and median. Correlation analysis was carried out based on the Pearson correlation coefficient (α<0.05).
ResultsThe 30 patients included in the study (15 males and 15 females) presented a mean age of 36.5 years (SD: 5.5) and a body mass index (BMI) of 23.7kg/m2 (SD: 5.6) in males and 24.1kg/m2 (SD: 3.9) in females. In 5 cases (16.7%), DKA was the form of presentation of the disease, while the rest of the subjects presented a mean duration of the disease of 13.2 years (SD: 4.9). In these cases the most frequent DKA triggering factor was insulin omission (46.7%), followed by infection (13.3%), other concomitant diseases or processes (6.7%), insulin pump problems (6.7%) or dietary transgression (3.3%).
Upon admission, blood glucose was 415±106mg/dl, bicarbonate 9.6mmol/l (SD: 1.5), pH 7.13mmol/l (SD: 0.04), BHB 4.33mmol/l (SD: 0.48) and ketonuria 3+ (n: 24) and 4+ (n: 6). The glycosylated hemoglobin (HbA1c) value was 10.54% (SD: 1.21).
For evaluating the course, the patients were divided into three groups according to the time to resolution of DKA (group 1: <24h; group 2: 24–48h, and group 3: >48h). The overall time to resolution was 28.7h (SD: 16), while the mean time to resolution in group 1 (G1) was 17.58h (SD: 3.23). Group 1 (G1) comprised 20 cases (66.7%), group 2 (G2) 4 cases (13.3%), and group 3 (G3) 6 cases (20%).
Decreasing BHB concentrations were accompanied by a rise in serum bicarbonate and pH, the correlation of these parameters being statistically significant: bicarbonate (r=−0. 24139; P=0.0161) and pH (r=−0.56419; P<0.0001).
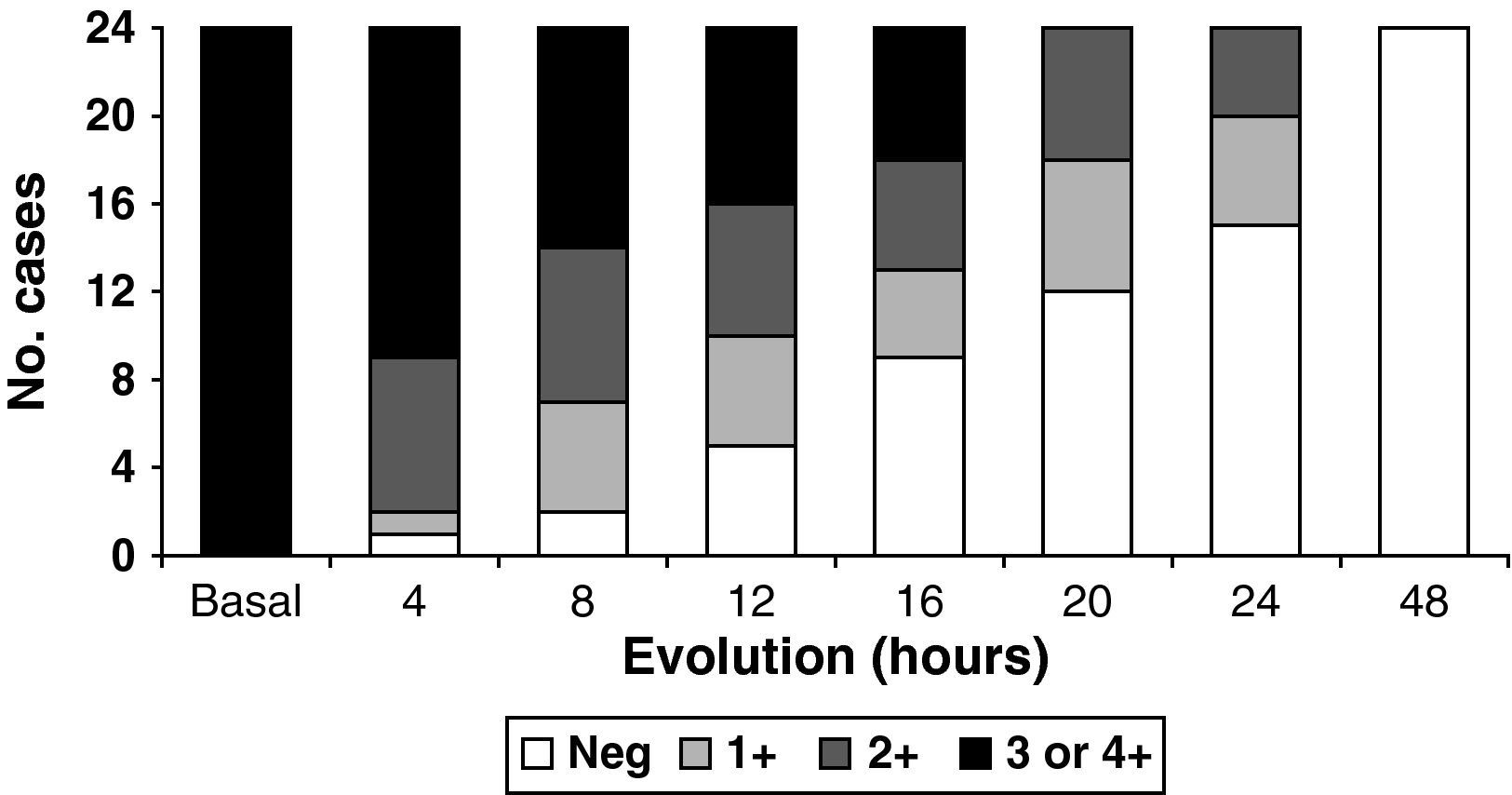
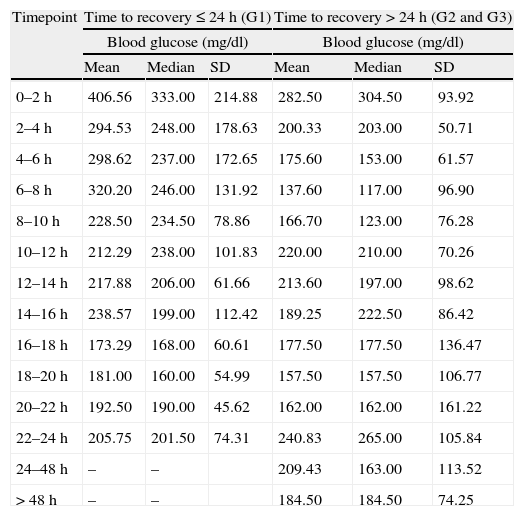
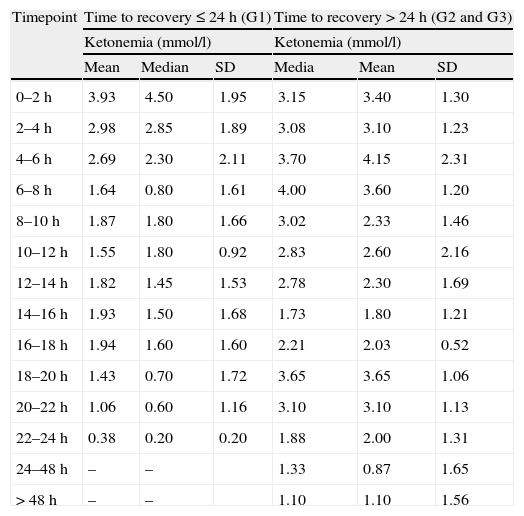
BHB normalized before ketonuria in the three groups into which the study population was stratified (G1: 15.5 vs 18.8h, P<0.05; G2: 18.2 vs 23.5h, P<0.01; G3: 37.3 vs 41.7h, P<0.01). Ten percent of the patients continued to present positive ketonuria readings with normal ketonemia (<0.5mmol/l). However, the times to normalization of ketonemia and ketonuria showed a statistically significant correlation in all the groups (group 1: P=0.042; group 2: P=0.007; and group 3: P=0.008). Fig. 1 shows the evolutive results of the ketonuria determinations in the cases where DKA resolved in under 48h, as these were the cases that could be fully monitored to negative conversion. Tables 1 and 2 show the evolutive data corresponding to blood glucose and capillary ketonemia. The data for groups 2 and 3 have been merged, due to the small sample sizes involved. Group 1 showed ketonemia normalization between 22 and 24h, coinciding with biochemical normalization of the DKA. In the rest of the groups the ketone body values in capillary blood (and in urine) remained elevated in some cases after 48h.
Time course of blood glucose during the resolution of diabetic ketoacidosis.
| Timepoint | Time to recovery≤24h (G1) | Time to recovery>24h (G2 and G3) | ||||
| Blood glucose (mg/dl) | Blood glucose (mg/dl) | |||||
| Mean | Median | SD | Mean | Median | SD | |
| 0–2h | 406.56 | 333.00 | 214.88 | 282.50 | 304.50 | 93.92 |
| 2–4h | 294.53 | 248.00 | 178.63 | 200.33 | 203.00 | 50.71 |
| 4–6h | 298.62 | 237.00 | 172.65 | 175.60 | 153.00 | 61.57 |
| 6–8h | 320.20 | 246.00 | 131.92 | 137.60 | 117.00 | 96.90 |
| 8–10h | 228.50 | 234.50 | 78.86 | 166.70 | 123.00 | 76.28 |
| 10–12h | 212.29 | 238.00 | 101.83 | 220.00 | 210.00 | 70.26 |
| 12–14h | 217.88 | 206.00 | 61.66 | 213.60 | 197.00 | 98.62 |
| 14–16h | 238.57 | 199.00 | 112.42 | 189.25 | 222.50 | 86.42 |
| 16–18h | 173.29 | 168.00 | 60.61 | 177.50 | 177.50 | 136.47 |
| 18–20h | 181.00 | 160.00 | 54.99 | 157.50 | 157.50 | 106.77 |
| 20–22h | 192.50 | 190.00 | 45.62 | 162.00 | 162.00 | 161.22 |
| 22–24h | 205.75 | 201.50 | 74.31 | 240.83 | 265.00 | 105.84 |
| 24–48h | – | – | 209.43 | 163.00 | 113.52 | |
| > 48h | – | – | 184.50 | 184.50 | 74.25 | |
G: group.
Time course of ketonemia during the resolution of diabetic ketoacidosis.
| Timepoint | Time to recovery≤24h (G1) | Time to recovery>24h (G2 and G3) | ||||
| Ketonemia (mmol/l) | Ketonemia (mmol/l) | |||||
| Mean | Median | SD | Media | Mean | SD | |
| 0–2h | 3.93 | 4.50 | 1.95 | 3.15 | 3.40 | 1.30 |
| 2–4h | 2.98 | 2.85 | 1.89 | 3.08 | 3.10 | 1.23 |
| 4–6h | 2.69 | 2.30 | 2.11 | 3.70 | 4.15 | 2.31 |
| 6–8h | 1.64 | 0.80 | 1.61 | 4.00 | 3.60 | 1.20 |
| 8–10h | 1.87 | 1.80 | 1.66 | 3.02 | 2.33 | 1.46 |
| 10–12h | 1.55 | 1.80 | 0.92 | 2.83 | 2.60 | 2.16 |
| 12–14h | 1.82 | 1.45 | 1.53 | 2.78 | 2.30 | 1.69 |
| 14–16h | 1.93 | 1.50 | 1.68 | 1.73 | 1.80 | 1.21 |
| 16–18h | 1.94 | 1.60 | 1.60 | 2.21 | 2.03 | 0.52 |
| 18–20h | 1.43 | 0.70 | 1.72 | 3.65 | 3.65 | 1.06 |
| 20–22h | 1.06 | 0.60 | 1.16 | 3.10 | 3.10 | 1.13 |
| 22–24h | 0.38 | 0.20 | 0.20 | 1.88 | 2.00 | 1.31 |
| 24–48h | – | – | 1.33 | 0.87 | 1.65 | |
| > 48h | – | – | 1.10 | 1.10 | 1.56 | |
G: group.
In the satisfaction questionnaire administered to the professionals, the determination of capillary ketonemia was very positively assessed as being convenient and practical in 93.3% of the cases, and 96.7% considered the technique to be more reliable than ketonuria.
DiscussionThe measurement of capillary ketonemia has been available for several years in our setting, with the main application of differentiating simple hyperglycemia from major metabolic decompensation.6,7 With this technique it has been shown that the incidence of cases requiring hospital admission or emergency care decreased 50% among the patients in which ketonemia was measured during days with concomitant diseases or processes, compared with those in which urine strips were used.13 The present study shows that during DKA treatment, capillary ketonemia is directly related to the severity of acidosis and to the serum bicarbonate and pH values, in concordance with the observations of other authors.5,14,15 Capillary ketonemia allows real-time assessment of the metabolic condition of the patient, and moreover constitutes a key diagnostic parameter for starting the treatment of ketoacidotic decompensation.8,9 In addition, there is good correlation with ketonemia determination in plasma.5
Although in recent decades there has been important progress in the monitorization of capillary blood glucose, the analysis of ketone bodies in capillary blood has had little impact, since in many centers ketonuria measurement with reactive strips remains the standard practice. In addition to being a semiquantitative technique, the urine strip fundamentally measures acetoacetate, not BHB – the ketone body that most precisely assesses the course of DKA. A limitation to its use is the fact that obtainment of the urine sample in the emergency service can often cause a delay in both diagnosis and treatment. In practice, there may be a delay of between 20min and 2h between patient admission and obtainment of the first urine sample.9 On the other hand, the result of ketonuria testing can be affected by a number of drugs, such as captopril, N-acetylcysteine, penicillamine and ascorbic acid, with the risk of obtaining false readings.5
Another aspect to be taken into account in relation to ketone body monitoring of the course of DKA is the fact that during the resolution phase BHB is oxidized back to acetoacetate; as a result, ketonuria measurement, which detects the latter substance, proves positive during the course of ketosis and remains positive once ketosis has been reverted. In effect, we have seen that some patients maintained positive ketonuria levels after the normalization of ketonemia. This may give rise to a potential risk of hypoglycemia if supplementary insulin dosing is carried out to revert ketosis.4 In the present study we have observed that there is no constant relationship between the ketonemia and ketonuria values, particularly in the first hours after starting treatment for DKA. In contraposition to the abovementioned limitations, the capillary ketonemia technique is easy to perform, offers immediate results, and is not affected by concomitant medication. In effect, for the clinicians in the study, BHB measurement was seen to be a more convenient, practical and reliable diagnostic method in the emergency care setting than the determination of ketonuria.
The decrease in BHB was accompanied by a reduction in serum bicarbonate and pH, with a correlation between the two variables, in coincidence with the observations of other authors.15,16 The levels of bicarbonate and pH represent nonspecific parameters of DKA, and pose some limitations. In effect, the pH value is susceptible to sudden ventilation changes, and bicarbonate can be elevated in chronic respiratory acidosis and decrease in chronic kidney disease. Moreover, the bicarbonate deposits take time in recovering after the resolution of metabolic acidosis.1 There also may be interferences in the acid–base balance from other situations, especially negative anion gap hyperchloremic acidosis.17 Capillary ketonemia is much less invasive than blood gas measurement, offers the opportunity of monitoring the patient on an hourly basis independently of the degree of dehydration,16 and requires no interpretation of laboratory data.18 In addition, BHB is an early marker of both decompensation and recovery of patient metabolic status. As an example, this parameter recovers earlier and more relevantly than blood glucose after interruption and reinitiation of the insulin infusion pump.19
On the other hand, the management of DKA has evolved in the last 40 years from the administration of high insulin doses to more modern protocols that recommend insulin therapy in intravenous perfusion at low doses until blood glucose is normalized. It is known that in many cases ketosis and acidosis can persist for hours after the correction of hyperglycemia; insulin therapy therefore must be continued together with intravenous glucose. The monitoring of ketonemia, which affords real-time values, makes it possible to adjust the insulin dosage according to normalization of both the blood glucose and ketonemia levels. Mention should be made of the economical efficiency of DKA management based on BHB normalization,16 since it allows faster transition from intravenous to subcutaneous insulin, reducing patient stay in intensive care or in the emergency service. There are no conclusive results drawn from specific economical assessment studies.20
Despite the limitation implied by the few cases reported, our findings indicate that capillary ketonemia measurement offers improvement in the management of DKA in the emergency setting, involving a much less invasive approach than blood gas measurement, and allowing hourly monitorization of the patient condition independently of the degree of dehydration. The technique is moreover easy to use, and makes it possible to more precisely define the required duration of intravenous treatment. Future studies are needed to evaluate the impact of capillary ketonemia in terms of shortened stay in the emergency service or critical care unit, and as regards the potential cost-effectiveness resulting from simplification of the usual intervention protocol.
Conflicts of interestThe authors state that they have no conflicts of interest.
The autodiagnostic material for this study was supplied by Abbott Diabetes Care, España, which in turn offered logistic support and served as coordinator among the participating hospital centers.
Please cite this article as: Rodríguez-Merchán B, et al. Betahidroxibutirato capilar en la monitorización de la cetoacidosis diabética. Endocrinol. Nutr. 2011;58:347-52.