This article reports a case of hyperthyroidism in a pregnant woman with hyperreactio luteinalis (HL), which may mimic gestational trophoblastic disease (GTD) and therefore requires a careful differential diagnosis.
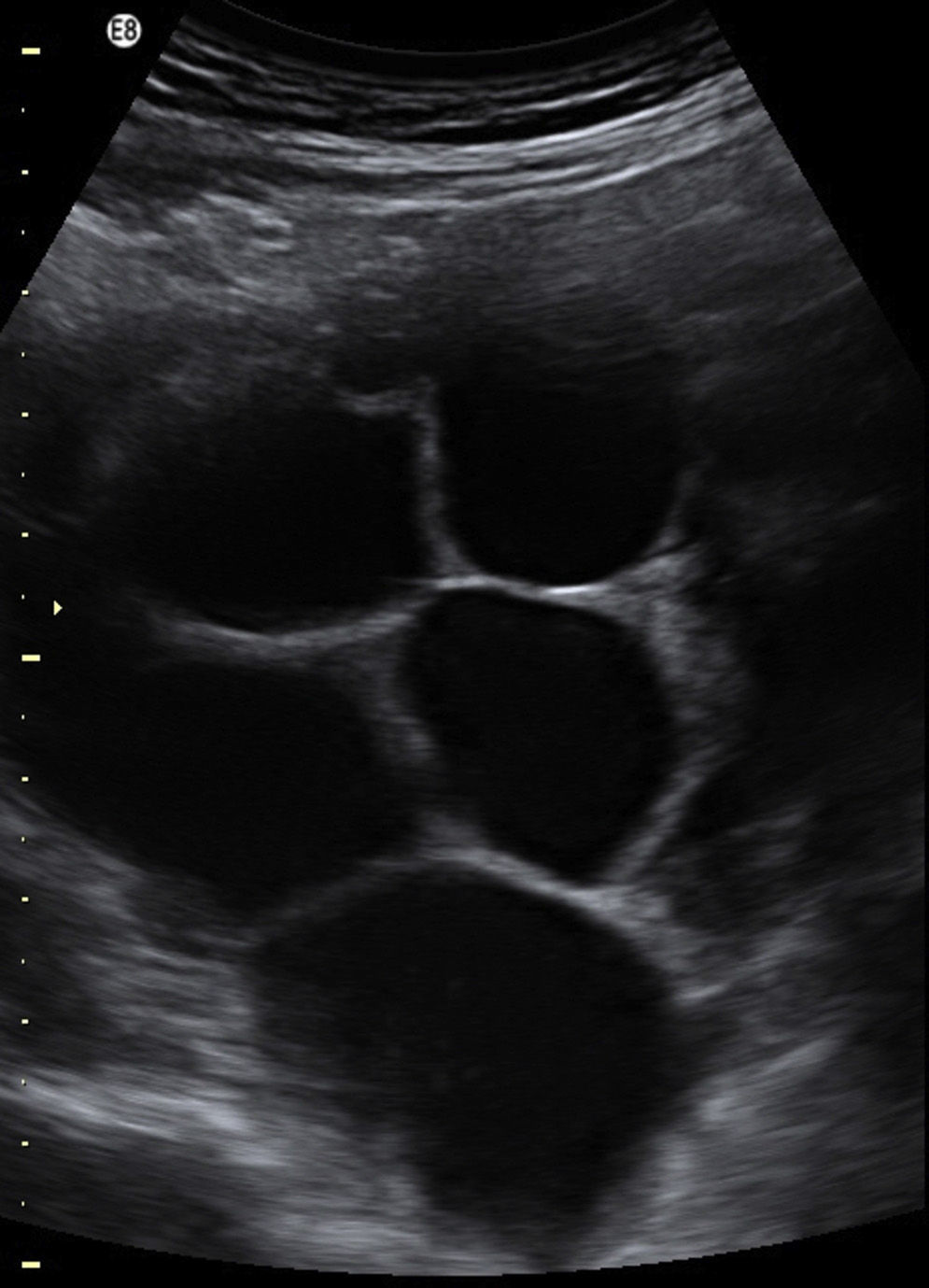
A nulligravida woman (with an 11-week pregnancy) was referred to endocrinology due to the finding of suppressed TSH with elevated FT4. She had no family or personal history of interest. The patient was in good clinical condition, except for low weight gain and sialorrhea. Examination revealed moderate diffuse goiter, with no signs of Graves’ ophthalmopathy. Laboratory test results included TSH level of 0.01mU/mL (0.4–4.0) and free thyroxine level >7.77ng/dL (0.89–1.80). Thyroid antibodies were negative. Thyroid ultrasound examination showed diffuse goiter and no nodules. Laboratory results were confirmed at week 13 of pregnancy. Ultrasonography showed a single pregnancy with a normal amount of amniotic fluid and enlarged ovaries, and multiple thin-walled, anechoic formations consistent with theca-lutein cysts (Fig. 1). Tumor markers (CEA, CA 15.3, CA 19.9, and CA 125) were tested due to the possibility of bilateral mucinous cystadenoma with normal results. The βHCG level was 155.562mU/mL). A chorionic villus biopsy performed at 14 weeks was consistent with a fetus with normal chromosomes. Treatment with methimazole 10mg/day was prescribed.
Polycystic images persisted in ultrasound examination at week 15, but gradually decreased in size in subsequent examinations until they completely disappeared. The patient continued on antithyroid treatment until a live female fetus was delivered by cesarean section at week 38. βHCG gradually decreased to a normal level (1.8mU/mL) in postpartum laboratory tests, which also showed a TSH level of 0.22mU/mL and a FT4 level of 1.12ng/mL.
A diagnosis of hyperthyroidism in pregnancy is based on suppressed TSH with increased FT4 or FT3 levels.1,2 In the first trimester of pregnancy, TSH levels decrease due to stimulation by βHCG of the TSH receptor (TSHr), with a peak between 7 and 11 weeks. Thus, TSH levels ranging from 0.03mU/mL to 2.5mU/mL are considered normal in the first trimester, while values up to 3.0mU/mL are considered normal in the second and third trimesters. Therefore, low TSH levels in the first trimester with normal FT4 may be considered “physiological!”.1 As to the etiology of hyperthyroidism, there are conditions caused by pregnancy itself, encompassed under the term of transient gestational thyrotoxicosis (TGT). On the other hand, any other etiology of thyroid hyperfunction occurring outside pregnancy may also develop during pregnancy.2
TGT is the most common cause of hyperthyroidism in pregnancy (1–3% of all pregnancies). TGT is defined as hyperthyroidism limited to the first half of pregnancy in the absence of thyroid antibodies and the physical features of Graves’ disease (GD). The condition results from increased βHCG levels or a greater affinity of the hormone for TSHr.2,3 The most characteristic condition is hyperemesis gravidarum, but multiple pregnancy or GTD may also occur. Other less common causes include HL or hyperplacentosis, characterized by increased placental weight and βHCG production. In gestational familial thyrotoxicosis (GFT) there is hypersensitivity to TSHr at physiological βHCG levels due to a dominant autosomal mutation.2
In the reported patient, the clinical signs and supplemental tests were not consistent with GTD or toxic uni- or multinodular goiter. Sustained βHCG levels in the high range throughout pregnancy and theca-lutein cysts suggested GTD; however, the uterus had an adequate size for the time of amenorrhea and did not show the characteristic “snowflake” image, there was a fetus, and the karyotype studied in the chorionic villus biopsy was normal. In addition, the patient had no symptoms of hyperemesis gravidarum and there was no family history of a similar condition, which made GFT unlikely.
The data therefore suggested hyperthyroidism due to HL, a benign condition which is uncommon in pregnancies not associated with GTD (approximately 30 cases have been reported in normal single pregnancies4). Its etiology is unknown, but it is thought that high βHCG levels and increased ovarian sensitivity to the hormone lead to the formation of theca-lutein cysts.5,6 Patients may experience complications such as twisting, abdominal pressure, or intracystic bleeding5,7,8; however, the condition usually causes no symptoms and is incidentally found in pelvic ultrasonography or cesarean section. Most cases (54%) are diagnosed in the third trimester (only 16% are diagnosed in the first trimester).4,6,9 HL may be confused with ovarian hyperstimulation syndrome, but the latter usually occurs in the first trimester, is associated with more severe symptoms (abdominal pain and ascites), and occurs more frequently after the induction of ovulation.6
Ovarian doppler ultrasonography is the main imaging test to establish diagnosis; the presence of color flow inside a septum or a solid component suggests malignancy. In the reported case, cystic images with no solid component and low enhancement with color doppler suggested a benign condition, as did subsequent cyst regression and resolution.4,5,8 Abdominal magnetic resonance imaging was not requested because it provides no additional information in these cases, as shown by the study by Haimor-Kochman et al.5
Recurrence in subsequent pregnancies has been reported in very few cases in the literature.6 Other potential complications associated with HL include preterm delivery, eclampsia, HELLP syndrome,4 and hyperandrogenism (25% of cases).6,7,9
In conclusion, although HL is extremely rare in normal single pregnancies, it is important to differentiate it from malignant tumors to avoid unnecessary surgery, given that spontaneous symptom resolution and cyst regression reported in the reviews available warrant a conservative management.6,7
Please cite this article as: González Aguilera B, Guerrero Vázquez R, Moreno Reina E, Gros Herguido N, Relimpio Astolfi F. Hiperreactio luteinalis, una causa rara de hipertiroidismo en la gestación. Endocrinol Nutr. 2015;62:146–147.