Diabetes education is an essential tool to achieve treatment objectives in type 1 diabetes mellitus (T1DM). The aim of this study was to determine if understanding of diabetes by caregivers/patients or sociodemographic factors affect blood glucose control in children and adolescents with T1DM.
Patients and methodsThe level of knowledge of 105 caregivers of children and adolescents with T1DM was assessed using a survey adapted to the type of treatment used (multiple dose insulin [MDI] or continuous subcutaneous insulin infusion [CSII]). Mean HbA1c levels in the previous year was considered as metabolic control marker.
ResultsMean HbA1c levels were similar in both treatment groups, with slightly higher values in children over 12years of age. Patients on CSII had a longer time since disease onset and had poorer results, maybe because the items were more difficult due to the higher level of knowledge required for this treatment modality (p=0.005). Caregivers with lower educational levels achieved poorer scores in the survey, but mean HbA1c levels of their children were lower, probably because of their greater involvement in disease care.
ConclusionsThe level of knowledge of caregivers and/or patients with T1DM was high, and this was associated to good metabolic control. Studies to assess the impact of caregiver knowledge on metabolic control of children are needed.
En la diabetes mellitus tipo1 (DM1) la educación diabetológica es fundamental para lograr los objetivos de tratamiento. El objetivo de este estudio es determinar si el nivel de conocimientos diabetológicos de cuidadores/pacientes o los factores sociodemográficos afectan al control glucémico de niños y adolescentes con DM1.
Pacientes y métodosSe analiza el nivel de conocimientos de 105 cuidadores de niños y adolescentes con DM1 o de los pacientes adolescentes mediante una encuesta adaptada a la modalidad de tratamiento (múltiples dosis de insulina [MDI] o bomba de infusión subcutánea continua de insulina [ISCI]). Se considera la HbA1c media en el último año como marcador del control metabólico.
ResultadosLa media de HbA1c fue similar en ambos grupos de tratamiento (6,6±0,5 para MDI y 6,5±0,5% para ISCI, p=0,63), siendo discretamente más alta en niños mayores de 12años. Los pacientes con bomba tenían un mayor tiempo de evolución de la diabetes y obtuvieron peores resultados porque además la exigencia teórica de la encuesta fue superior por la mayor complejidad de manejo (p=0,005). Los cuidadores con nivel de estudios más bajos obtuvieron peores puntuaciones, si bien las cifras de HbA1c de sus hijos fueron más bajas, en probable relación con una mayor dedicación al cuidado de la enfermedad.
ConclusionesEl nivel de conocimientos analizados fue alto, y esto se asoció con un buen control metabólico. Son necesarios estudios que evalúen la influencia de los conocimientos de los cuidadores en pacientes con diferentes grados de control metabólico.
Type 1 diabetes mellitus (T1DM) is the most common form of diabetes in children. The Diabetes Control and Complications Trial (DCCT) showed that poor blood glucose control increases the risk of chronic microvascular complications, including renal and retinal complications.1 When T1DM starts in children or young adults, the course of disease is long, and metabolic control is essential to prevent the occurrence of such complications.2,3
Advances in treatment of T1DM have decreased the risk of complications and delayed their occurrence, with the resultant overall increase in quality of life of patients. Nutritional education, with systematic assessment of carbohydrates and use of the insulin-to-carbohydrate ratio, has allowed for optimizing insulin dosage.4 The basal-bolus scheme with multiple dose insulin (MDI) injections or continuous subcutaneous insulin infusion (CSII) and multiple capillary blood glucose measurements allow for better metabolic control. For this, adequate and continued diabetes education of patients and families is required.5,6 And although the effect of glycemic variability on the occurrence of chronic complications is unknown, the current goals of treatment of T1DM are to maintain adequate pre- and post-prandial blood glucose levels, avoiding both hyperglycemia and hypoglycemia, both harmful for the central nervous system and cardiovascular risk.7–9
Diabetes education is the main therapeutic tool to achieve implication of the family in care of children with T1DM, and the best metabolic control is achieved when participation and intervention of patients and families are adequate. Family empowerment refers to caregivers who have received more comprehensive training in management of diabetes in order to make them able to make decisions in multiple situations.10 This results in improved blood glucose control, and treatment optimization is greater the more intensified the modality used.11
There are studies assessing quality of life of patients in relation to the degree of metabolic control. The conclusion of such studies is that the better the metabolic control, the greater the quality of life perceived.12,13 The essential role of diabetes education nurses for achieving better metabolic control is also known.14,15 It is however difficult to find references describing the impact of patients and family education on glucose control.16
The purpose of this study was to assess whether the level of diabetes knowledge of caregivers/patients or sociodemographic factors affect blood glucose control in children and adolescents with T1DM. Secondary objectives were to ascertain whether better metabolic control contributes to decrease the occurrence of acute events (ketoacidosis and severe hypoglycemia) and whether differences exist in metabolic control related to the treatment modality used (MDI or CSII).
Patients and methodsAn observational, cross-sectional, non-interventional study was conducted on the knowledge and skills of families about management for diabetes. All caregivers of patients with T1DM up to 18 years of age who attended the pediatric diabetes clinic of Hospital Ramón y Cajal (Madrid) from November 2013 to January 2014 were surveyed. Caregivers agreed to participate and signed the appropriate informed consent. The study was approved by the ethics committee of the hospital.
One hundred and five patients out of the more than 350 patients regularly monitored at the unit participated in the study. Four pediatric endocrinologists and two diabetes education nurses collaborated in the study. The inclusion criterion was onset of T1DM more than two years before.
Most patients lived in the Madrid region, but some were from other regions but had received diabetes education from the same team. All patients were receiving intensified treatment for diabetes, either MDI or CSII, according to the recommendations of the International Society for Pediatric and Adolescent Diabetes (ISPAD),17 basal insulin detemir as one or two doses in those given and insulin aspart before each of the main meals for both modalities (3–5 doses daily), always based on the specific needs of each patient.
Data on age (with patient stratification into two groups, under 12 years and 12 years or older) and time since onset of diabetes were assessed. Mean HbA1c levels (using the Menarini HPLC method, NR 5.31±0.31%) as metabolic control marker (values <7% indicated good control), number of severe hypoglycemic events (with impaired consciousness. seizures, or coma), and number of episodes of hyperglycemia with ketosis and admission for ketoacidosis (ketotic decompensation) in the past year were assessed.
Surveys used included the one proposed by Mitchell et al.16 for patients on CSII and a modified survey for patients treated with MDI to be able to extrapolate the level of knowledge acquired from diabetes education with both treatment modalities. The survey was translated according to the concepts in Spanish explained during education sessions and at the visits, and for treatment with MDI, the concept in each question was extrapolated to the treatment modality (infusion system was replaced by type of needle, concepts related to basal rate were replaced by long-acting basal insulin, those related to boluses by fast-acting insulin, those related to pump handling by subcutaneous injection; the only concept that could not be extrapolated, the maximum bolus configured, was replaced by a conceptual question on duration of insulin action). After these changes, the survey addressed most concepts considered to be important for adequate diabetes control with both treatment modalities. Parents were asked about their educational level (higher, secondary, or primary education).
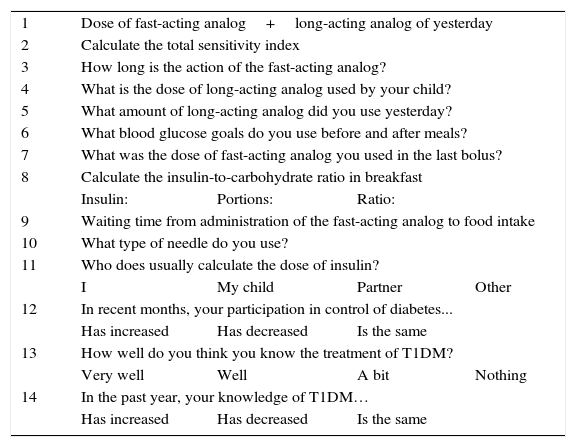
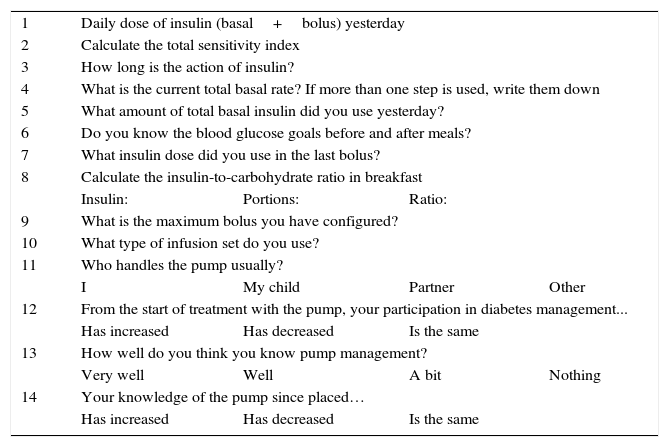
The main caregiver and the adolescent, when he/she was responsible for disease control, completed the 14-item diabetes knowledge questionnaire adapted to the treatment modality (MDI or CSII) (Tables 1 and 2). The first ten questions objectively assessed theoretical knowledge of the disease and its treatment, and were more complex in the model for CSII because this modality is supposed to require a greater level of technical knowledge. Adequate knowledge of basic concepts for daily management of the disease and its treatment method was required to answer the questions. The last four questions subjectively assessed the perception by parents and patients of their degree of involvement in care and their acquisition of knowledge about the disease over time. No cut-off point for considering disease knowledge adequate was established for the first ten questions. Our interest was rather to evaluate results between patients with the same treatment modality and to those using the other insulin administration method. Subjective questions were managed as information on perception by caregivers/patients, and were not related in any way to objective data.
Questions of the survey on treatment with MDI.
| 1 | Dose of fast-acting analog+long-acting analog of yesterday | |||
| 2 | Calculate the total sensitivity index | |||
| 3 | How long is the action of the fast-acting analog? | |||
| 4 | What is the dose of long-acting analog used by your child? | |||
| 5 | What amount of long-acting analog did you use yesterday? | |||
| 6 | What blood glucose goals do you use before and after meals? | |||
| 7 | What was the dose of fast-acting analog you used in the last bolus? | |||
| 8 | Calculate the insulin-to-carbohydrate ratio in breakfast | |||
| Insulin: | Portions: | Ratio: | ||
| 9 | Waiting time from administration of the fast-acting analog to food intake | |||
| 10 | What type of needle do you use? | |||
| 11 | Who does usually calculate the dose of insulin? | |||
| I | My child | Partner | Other | |
| 12 | In recent months, your participation in control of diabetes... | |||
| Has increased | Has decreased | Is the same | ||
| 13 | How well do you think you know the treatment of T1DM? | |||
| Very well | Well | A bit | Nothing | |
| 14 | In the past year, your knowledge of T1DM… | |||
| Has increased | Has decreased | Is the same | ||
Modified from Mitchell et al.16
Questions of the survey on treatment with CSII.
| 1 | Daily dose of insulin (basal+bolus) yesterday | |||
| 2 | Calculate the total sensitivity index | |||
| 3 | How long is the action of insulin? | |||
| 4 | What is the current total basal rate? If more than one step is used, write them down | |||
| 5 | What amount of total basal insulin did you use yesterday? | |||
| 6 | Do you know the blood glucose goals before and after meals? | |||
| 7 | What insulin dose did you use in the last bolus? | |||
| 8 | Calculate the insulin-to-carbohydrate ratio in breakfast | |||
| Insulin: | Portions: | Ratio: | ||
| 9 | What is the maximum bolus you have configured? | |||
| 10 | What type of infusion set do you use? | |||
| 11 | Who handles the pump usually? | |||
| I | My child | Partner | Other | |
| 12 | From the start of treatment with the pump, your participation in diabetes management... | |||
| Has increased | Has decreased | Is the same | ||
| 13 | How well do you think you know pump management? | |||
| Very well | Well | A bit | Nothing | |
| 14 | Your knowledge of the pump since placed… | |||
| Has increased | Has decreased | Is the same | ||
Modified from Mitchell et al.16
All families/patients had received diabetes education at our diabetes unit at diagnosis (25h in one week), after one month, and at each subsequent clinical visit. Education was provided by both endocrinologist and diabetes education nurses of the unit. Education sessions stress basic concepts of the disease (insulin, carbohydrate portions, basic nutritional concepts, sensitivity index) and its daily management (types of insulin, administration methods, characteristics of each system), with interactive explanation of theoretical and practical concepts and supervising the insulin administration method after calculating with ratios and sensitivity indexes the dose corresponding to specific food portions. Patients referred from other Madrid areas or other regions received a complete initial education cycle with the same subsequent retraining.
IBM SPSS Statistics version 22 software was used for statistical analysis of basic descriptive data (absolute and relative frequencies, means, and standard deviations) and Student's t and Chi-square tests were used for hypothesis testing. Values of p<0.05 were considered statistically significant.
ResultsA total of 105 surveys were analyzed, of which 67 and 38 were completed by relatives/patients treated with MDI and CSII respectively. Mean patient age at the time of the study was 11.4±3.6 and 11.5±4.2 years in MDI and CSII patients respectively (p=0.86). Mean age at diagnosis was 5.9±3.7 years in patients on MDI and 4.4±3.9 years in those on CSII (p=0.052), and mean time since disease onset was 5.5±3.9 and 7.3±4.1 years respectively (p=0.029).
Estimated metabolic control based on mean HbA1c in the past year was 6.6±0.5% for MDI and 6.5±0.5% for CSII (p=0.63). No patient had experienced episodes of ketoacidosis or severe hypoglycemia in the previous year.
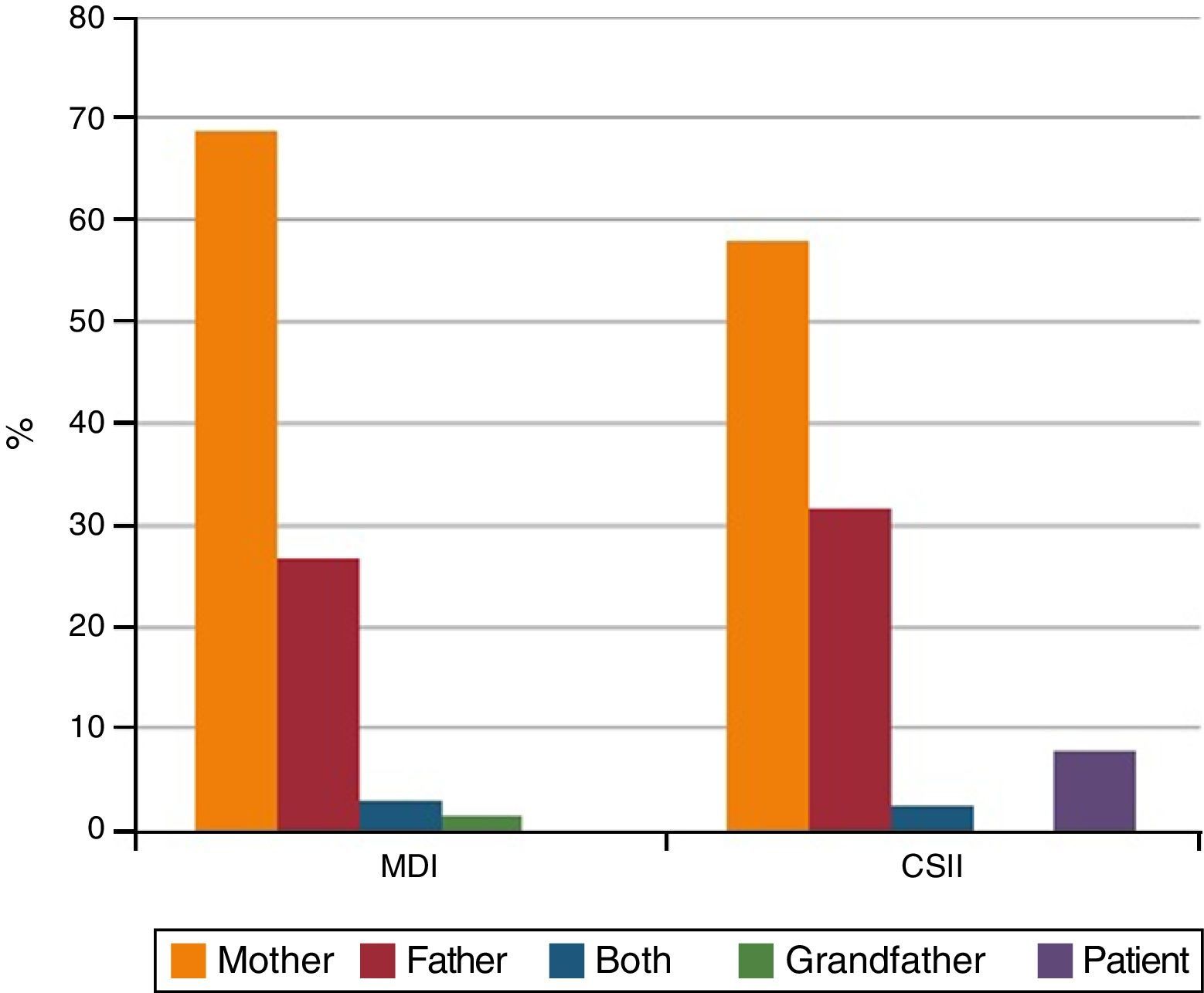
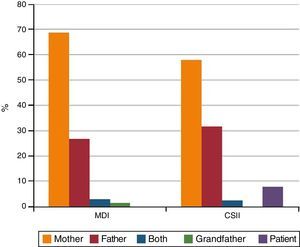
Surveys were completed by the mothers of 68.7% of patients on MDI and 57.9% of patients on CSII (p=0.16) (Fig. 1). Mean score in knowledge was 8.3 out of 10 in the MDI group and 7.5 in the CSII group (p=0.005).
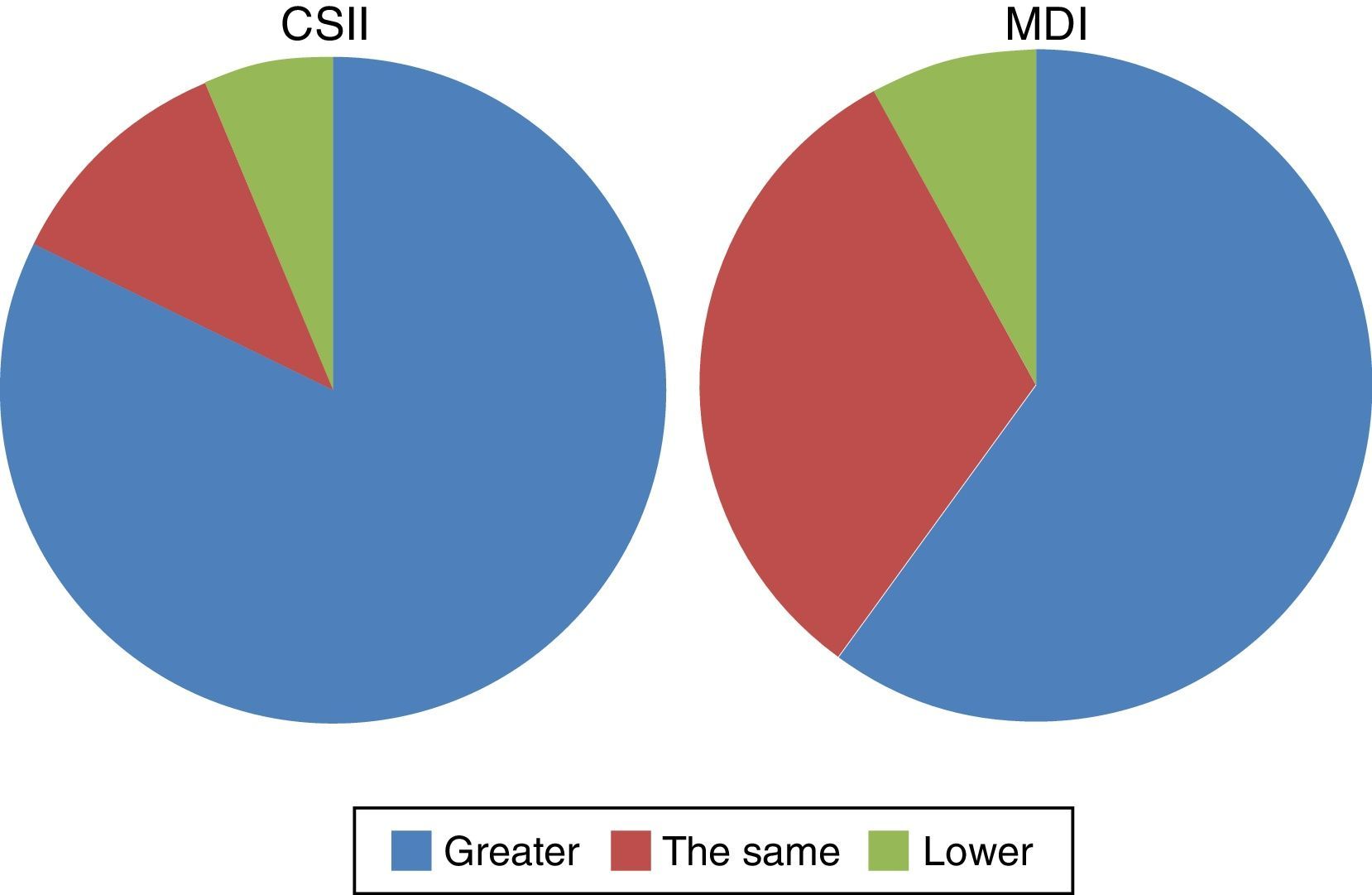
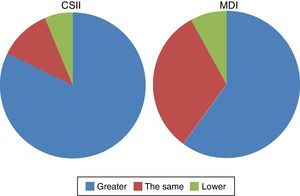
In subjective questions, 62.7% and 89.5% of patients treated with MDI and CSII respectively or their parents reported that their knowledge of diabetes had improved with successive visits and intensification in diabetes education (p=0.011) (Fig. 2).
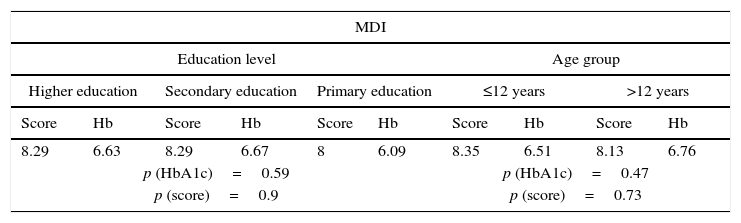
No statistically significant differences were found between the groups analyzed when the education level of caregivers and patient age were compared to the subjective score in the questionnaire (CSII: p=0.095 and p=0.20 respectively; MDI: p=0.79 and p=0.40 respectively) or the mean HbA1c level (CSII: p=0.41 and p=0.42 respectively; MDI: p=0.48 and p=0.42 respectively), but there was a trend to a poorer score in the survey when patient was older and the more elementary was the educational level of the caregiver (Table 3).
Analysis of mean scores in the questionnaire and HbA1c levels by treatment group, education level of the main caregiver, and age group.
| MDI | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Education level | Age group | ||||||||
| Higher education | Secondary education | Primary education | ≤12 years | >12 years | |||||
| Score | Hb | Score | Hb | Score | Hb | Score | Hb | Score | Hb |
| 8.29 | 6.63 | 8.29 | 6.67 | 8 | 6.09 | 8.35 | 6.51 | 8.13 | 6.76 |
| p (HbA1c)=0.59 | p (HbA1c)=0.47 | ||||||||
| p (score)=0.9 | p (score)=0.73 | ||||||||
| CSII | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Education level | Age group | ||||||||
| Higher education | Secondary education | Primary education | ≤12 years | >12 years | |||||
| Score | Hb | Score | Hb | Score | Hb | Score | Hb | Score | Hb |
| 7.75 | 6.54 | 7.17 | 6.33 | 6.25 | 6.93 | 8 | 6.44 | 6.9 | 6.66 |
| p (HbA1c)=0.055 | p (HbA1c)=0.54 | ||||||||
| p (score)=0.095 | p (score)=0.2 | ||||||||
Modified from Mitchell et al.16
No statistically significant differences were shown for any of the analyses performed to relate mean HbA1c levels with who was the main caregiver, the type of treatment, age, level of knowledge of the main caregiver, time since disease onset, or survey results in both objective and subjective items.
DiscussionThe degree of metabolic control is related to diabetes education of the patient or caregiver, but the good metabolic control of study patients – with HbA1c levels in the past year of 6.6±0.5% and 6.5±0.5% with MDI and CSII respectively – makes it difficult to find differences between treatment modalities. Mitchell et al.16 found similar results and emphasized the importance of diabetes education to improve metabolic control in children and adolescents treated with CSII. The benefits of diabetes education for long-term control of adult patients with T1DM and T2DM are also well known.14 We have found no studies in the literature assessing the impact of progress in knowledge of diabetes on the control of pediatric patients treated with MDI.
Patients treated with CSII had lower mean age at diagnosis and longer time since onset of T1DM at the time of the survey. The longer time since onset of diabetes in this group was due to recruitment of children diagnosed with T1DM before 6 years of age and older children diagnosed several years before and with adequate control who wanted to use this treatment modality. Age is a criterion for indication of CSII.6,17 Younger patients benefit from CSII because they have less total insulin requirements and because the infusion device allows for adapting treatment to an irregular intake. Moreover, parents are more dedicated to care of diabetes in young children.
An indication of good metabolic control in patients participating in the study was the absence of acute decompensation episodes with ketosis of severe hypoglycemia, either because patients usually had adequate blood glucose levels or because patients and their caregivers reacted to the first signs and symptoms of acute decompensation of the disease as the result of adequate diabetes education.
A limitation of the study was that the questionnaire used in each treatment modality was a non-validated translation into Spanish; for CSII, a translation of the original Mitchell questionnaire, and for MDI an adaptation by the authors. We consider important that patients with diabetes know both surveys and the results achieved in standard clinical practice.
The reported study has other limitations that may be analyzed based on the difficulties found by participants to complete the survey and the results obtained, and on the subsequent difficulty to validate responses. The level of theoretical knowledge required to answer the survey for the MDI group was basic, and caregivers needed to know the usual and individual routine of patient insulinization. The survey relating to CSII was more comprehensive as regards questions on theoretical knowledge and required understanding of pump function to obtain the information requested (last bolus, total basal dose of the previous day, maximum bolus configured etc.).
The question on blood glucose goals was answered yes or no in some surveys without detailing the values, possibly due to inadequate formulation of the question. In these cases, answers were considered erroneous. Thus, 68% of all responses in this item were incorrect (71% and 63% in the groups treated with MDI and CSII respectively, p=0.373). Another questions with a greater proportion of failures were those referring to duration of insulin action (in both surveys) and time from injection to intake (in the MDI questionnaire). Caregivers gave incorrect answers for duration of insulin action in MDI in 18% of the cases and in CSII in 23.7% of the cases (p=0.482). As regards time from injection to intake, 38% of patients on MDI did not wait the adequate time they had been recommended during educational sessions.
As regards relation between metabolic control and diabetes education, the study reflects some trends in analysis in the different groups assessed. Mean questionnaire scores were higher in the group treated with MDI. However, results can hardly be compared to those of the group treated with CSII because the questionnaire is more demanding for this second group due to the greater technical complexity of the CSII system. CSII therapy requires a higher degree of diabetes education provided more continuously and with greater interaction.4,10–12,16
No differences were seen in blood glucose control depending on the educational level of caregivers in the group treated with MDI. A trend to poorer metabolic control was seen in patients given CSII when caregivers had primary education. This trend may possibly be due to the greater difficulty for these caregivers to acquire new skills, although it cannot be ruled out that their training level was similar to that of parents with higher education level but they had problems to translate that knowledge into their answers to the test items. The economic level of parents was not considered in our study, although higher education levels are usually associated to higher economic levels.18
The study by Mitchell et al.16 concluded that the greater the education level of patients with CSII (as documented in the survey), the better the metabolic control. These authors found that the main reason for incorrect answers was inability to obtain data from reading of the infusion device and to answer the questions. Caregivers of patients with better metabolic control manipulated more often the infusion device, and answered that their degree of participation was the same or less since therapy had been changed from MDI to CSII. The education level of the main caregiver was not considered in this study.
Adolescent patients who completed the survey had poorer scores and poorer mean HbA1c values. Caregivers of adolescents who had started to delegate treatment to the patient also had a lower level of knowledge than before because the adolescent now had a greater participation in diabetes education and made his/her own decisions. Both circumstances are explained by the longer time since onset of disease and the impact of patient participation in control of his/her diabetes. Adolescents with T1DM, like any other adolescent with a chronic disease, demand autonomy, freedom, and greater participation in disease control, and sometimes confront their parents because of their overprotection.13,19 Because of this, there is less parental supervision in the group of adolescents.
An important finding in this study is that 62.7% of surveyed patient on MDI and 89.5% of those on CSII had the subjective impression that their knowledge of diabetes increased with the successive visits and the degree of metabolic control of patients was good and sustained over time.
In conclusion, a high level of knowledge of caregivers’ results in good metabolic control of children and adolescents with T1DM monitored at our pediatric diabetes unit, irrespective of type of treatment. Continued diabetes education is essential to achieve motivation and implication of families for reaching treatment goals and blood glucose control. Surveys allow for analyzing the most common mistakes in treatment of diabetes and, thus, for directing future educational interventions to reinforce knowledge and to improve and modify acquired behaviors. Hence the importance of developing tools to measure knowledge in diabetes adapted to the pediatric population and validated in Spanish. Studies assessing the impact of knowledge and continued education of caregivers on metabolic control in children and adolescents monitored at pediatric diabetes clinics are needed.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Alonso Martín DE, Roldán Martín MB, Álvarez Gómez MÁ, Yelmo Valverde R, Martín-Frías M, Alonso Blanco M, et al. Impacto de la educación diabetológica en el control de la diabetes mellitus tipo 1 en la edad pediátrica. Endocrinol Nutr. 2016;63:536–542.