To assess control of blood glucose and other cardiovascular risk factors in diabetic patients monitored at an outpatient endocrinology clinic. To ascertain treatment used and its changes over time.
Patients and methodsA cohort of 424 randomly selected diabetic patients (both type 1 and type 2) was monitored from 2004 to 2008. Final cohort size was 343 patients. Data were collected about epidemiological characteristics, cardiovascular risk factors, chronic complications, glycemic, lipid and blood pressure control, and treatment at baseline and 4 years.
ResultsAfter 4 years, the proportion of patients achieving glycosylated hemoglobin levels less than 7% remained stable (type 1: 18.5% in 2004 vs 21.7% in 2008, type 2: 26.6% vs 26.5%). The degree of achievement of lipid and blood pressure (BP) control levels increased in both groups. The complexity of treatment schemes used to achieve these results significantly increased.
ConclusionsStabilization of glycemic control after 4 years of follow-up was a positive result, considering the long course of diabetes, progressive pancreatic function impairment, and complexity of our cohort. Treatment optimization significantly improved BP and lipid control in the study group.
Valorar el grado de control glucémico y del resto de factores de riesgo cardiovascular en una cohorte de pacientes diabéticos seguidos en consultas externas durante 4 años. Conocer el patrón de tratamiento utilizado y su evolución.
Material y métodosEstudio de 424 pacientes diabéticos tanto tipo 1 (DM1) como tipo 2 (DM2), seleccionados aleatoriamente en 2004 y seguidos hasta 2008. La cohorte final fue de 343 pacientes. Se recogieron datos epidemiológicos, factores de riesgo cardiovascular, complicaciones crónicas, datos de control glucémico, lipídico y tensional, así como de tratamiento al inicio y a los 4 años.
ResultadosTras los 4 años, el porcentaje de pacientes que conseguían una hemoglobina glicada inferior a 7% se mantuvo estable (DM1 18,5 en 2004 frente a 21,7% en 2008 y DM2 26,6 frente a 26,5%). En ambos tipos de diabetes se incrementó de forma significativa el grado de consecución de objetivos de control lipídico y tensional. Para conseguir estos resultados las pautas de tratamiento se complicaron de manera significativa.
ConclusionesLa estabilización del control glucémico objetivada tras 4 años de seguimiento es un resultado positivo, considerando el largo tiempo de evolución de la enfermedad, el deterioro progresivo de la función pancreática y la complejidad de esta cohorte. Gracias a la optimización de los tratamientos utilizados, han mejorado de forma significativa el control tensional y lipídico del grupo estudiado.
The prevalence of diabetes mellitus, particularly type 2 diabetes, has increased considerably in recent years. It is estimated that by 2030 there will be over 366 million diabetics worldwide.1 Some of the causes that may account for this epidemic, such as obesity and sedentary lifestyles, are closely linked to the welfare society which exists in Western countries and to lifestyle changes in developing countries.2 The Di@bet.es study3 recently conducted in a representative sample of the Spanish population found an age-and sex-adjusted total prevalence of diabetes mellitus of 13.8%. The disease was undiagnosed in almost half the subjects (6.0%).
Diabetes is a condition which has a considerable healthcare and social impact because of its macroangiopathic and microangiopathic chronic complications and its high cardiovascular mortality.4,5 The need for intensive blood glucose control to prevent chronic complications of both type 1 (T1DM)6,7 and type 2 diabetes mellitus (T2DM)8–10 and the benefits of its long-term maintenance are well known. The disease should be treated using an integral approach to all the risk factors found in these patients. However, cardiovascular prevention clinical guidelines set goals which are difficult to achieve in practice.
The purpose of this study was to assess the extent to which the control goals of cardiovascular risk factors were achieved in a representative sample of diabetic patients seen at a specialized clinic under standard clinical practice conditions, and to ascertain the treatment pattern used and its changes over four years.
Patients and methodsAn observational, descriptive, 4-year study was conducted on a cohort of patients diagnosed with both T1DM and T2DM. During November and December, 424 patients were randomly selected from among those attending the outpatient clinic of endocrinology and nutrition of Hospital Virgen de la Salud (the first 2 patients diagnosed with diabetes mellitus seen each day at each clinic were selected).11 The group studied in 200411 continued to attend our clinics for regular monitoring until 2008. The final cohort size in 2008 was 343 patients. From the initial group selected in 2004, 23 patients died (5.4%: 48% due to cardiovascular causes, 22% due to tumors, and 30% for other reasons). All the patients who died belonged to the T2DM group. Fifty-eight patients were lost to follow-up (13.7%).
The following were collected from all patients:
- 1.
Epidemiological and clinical data: type of diabetes mellitus, time since diabetes onset, sex, and age.
- 2.
The presence of classical cardiovascular risk factors: arterial hypertension, hyperlipidemia, obesity, and smoking.
- 3.
The presence of microangiopathic (retinopathy and nephropathy) and macroangiopathic (cerebral, peripheral, and coronary vascular disease) chronic complications.
- 4.
Anthropometric data (weight, height, body mass index [BMI] and blood pressure) and blood glucose and lipid control laboratory findings: glycosylated hemoglobin (HbA1c), triglycerides, total cholesterol, high density lipoprotein cholesterol (HDL-C), and low density lipoprotein cholesterol (LDL-C).
- 5.
Treatments administered (insulin therapy, oral antidiabetics, antihypertensive drugs, lipid-lowering drugs, antiaggregants). The most comprehensive information was collected about hypoglycemic treatment, that is, insulin dose in IU/kg/day, the number of doses, and whether combined or not with oral antidiabetics.
Hypertensive patients were defined as those with blood pressure (BP) values ≥140/90mmHg or receiving antihypertensive treatment. Patients with dyslipidemia were defined as those who were taking lipid-lowering treatment or had total cholesterol>200mg/dL or LDL-C>160mg/dL or triglycerides>150mg/dL. Patients with BMI>30 were considered obese, and those who admitted smoking at least 1–2 cigarettes daily in the previous month were considered active smokers. Microalbuminuria was defined as the presence of at least 2 measurements of urinary albumin excretion >30mg/day or >30mg/g of creatinine in the baseline sample. The presence of retinopathy of any grade was established on the basis of annual eye examinations, the results of which were taken from the clinical records. Finally, patients were considered to have diabetic macroangiopathy if they had any clinical signs of cerebral, coronary, or peripheral vascular disease and/or had undergone any revascularization or vascular recanalization procedure.
The recommendations of the American Diabetes Association (ADA) were used to assess metabolic control (of blood glucose, lipids, and blood pressure).12 The following were considered as adequate control goals: HbA1c<7%, LDL-C<100mg/dL, HDL-C>50mg/dL, triglycerides<150mg/dL, systolic BP (SBP)<130mmHg, and diastolic BP (DBP)<80mmHg.
Cohort results, both overall and by type of diabetes, in the final review in 2008 were compared to the results recorded in the baseline 2004 analysis.11
Since June 2004, HbA1c has been measured at our hospital using ion exchange high performance liquid chromatography (HPLC) (Bio-Rad Laboratories Variant II HbA1c program), a method certified by the National Glycohemoglobin Standardization Program (NGSP) and standardized to the reference method of the Diabetes Control and Complication Trial; normal range: 4–6% (DCCT).
Statistical analysisSPSS V15 software was used for statistical analysis. Numerical data are given as mean and standard deviation for quantitative variables and as percentage for qualitative variables. The 95% confidence interval was calculated to the latter. Differences between means were analyzed using Student's t test. A Chi-square test was used to analyze differences between proportions. A McNemar test was used to compare proportions of paired data between both periods. A value of p<0.05 was considered statistically significant.
ResultsSociodemographic dataAmong the 343 patients enrolled, 60 had T1DM (17.5%) and 283 T2DM (82.5%). There were 42.6% male patients. Mean age at the time of the study was 66.5±14.5 years (45.1±14.7 for T1DM and 72.1±10.2 years for T2DM patients, p<0.001), and mean time since onset of diabetes was 20.3±8.2 years (23.0±10.0 in T1DM and 20.0±7.8 in T2DM patients, p<0.01).
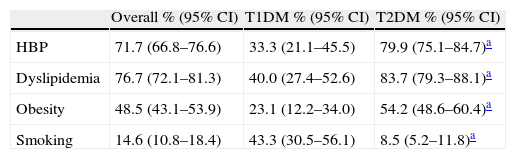
Prevalence of risk factors and chronic complicationsStudy patients had a high vascular risk profile. More than 70% were hypertensive or had dyslipidemia, and more than 45% were obese. This unfavorable risk profile was mainly seen in the T2DM group, except for active smoking, which was more common in the T1DM group. Table 1 shows the prevalence of cardiovascular risk factors.
Prevalence of classical cardiovascular risk factors in the overall 2008 cohort and for each group of diabetes.
| Overall % (95% CI) | T1DM % (95% CI) | T2DM % (95% CI) | |
| HBP | 71.7 (66.8–76.6) | 33.3 (21.1–45.5) | 79.9 (75.1–84.7)a |
| Dyslipidemia | 76.7 (72.1–81.3) | 40.0 (27.4–52.6) | 83.7 (79.3–88.1)a |
| Obesity | 48.5 (43.1–53.9) | 23.1 (12.2–34.0) | 54.2 (48.6–60.4)a |
| Smoking | 14.6 (10.8–18.4) | 43.3 (30.5–56.1) | 8.5 (5.2–11.8)a |
T1DM: type 1 diabetes mellitus; T2DM: type 2 diabetes mellitus; 95% CI: 95% confidence interval; HBP: high blood pressure.
More than one-fourth of patients (26.2%) had some macroangiopathic complication (31.4% of T2DM and 1.7% of T1DM patients, p<0.001). This group of patients constituted the secondary prevention group. Forty-three percent of diabetic patients had retinopathy (43.5% and 40.0% in the T2DM and T1DM groups, a non-significant [NS] difference), and 30% had retinopathy of some grade (31.8% and 21.7% in the T2DM and T1DM groups, NS).
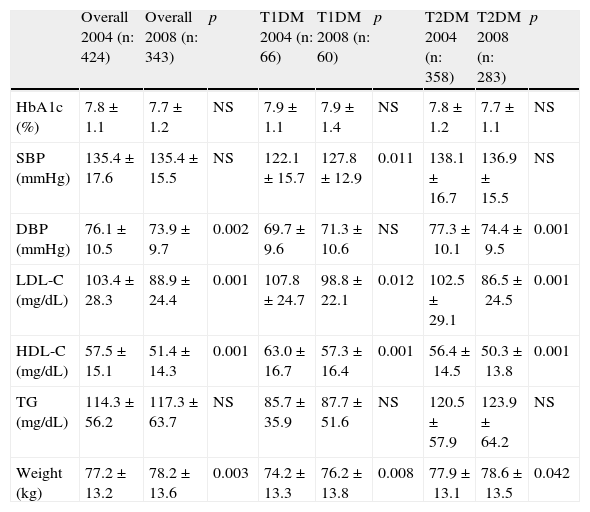
Metabolic and blood pressure controlTable 2 shows the final results of glucose, lipid, and blood pressure control in the study cohort, as well as the results obtained in the 2004 analysis.
Changes over time in chemical and anthropometric parameters: results in the overall group and for each type of diabetes comparing the two periods analyzed.
| Overall 2004 (n: 424) | Overall 2008 (n: 343) | p | T1DM 2004 (n: 66) | T1DM 2008 (n: 60) | p | T2DM 2004 (n: 358) | T2DM 2008 (n: 283) | p | |
| HbA1c (%) | 7.8±1.1 | 7.7±1.2 | NS | 7.9±1.1 | 7.9±1.4 | NS | 7.8±1.2 | 7.7±1.1 | NS |
| SBP (mmHg) | 135.4±17.6 | 135.4±15.5 | NS | 122.1±15.7 | 127.8±12.9 | 0.011 | 138.1±16.7 | 136.9±15.5 | NS |
| DBP (mmHg) | 76.1±10.5 | 73.9±9.7 | 0.002 | 69.7±9.6 | 71.3±10.6 | NS | 77.3±10.1 | 74.4±9.5 | 0.001 |
| LDL-C (mg/dL) | 103.4±28.3 | 88.9±24.4 | 0.001 | 107.8±24.7 | 98.8±22.1 | 0.012 | 102.5±29.1 | 86.5±24.5 | 0.001 |
| HDL-C (mg/dL) | 57.5±15.1 | 51.4±14.3 | 0.001 | 63.0±16.7 | 57.3±16.4 | 0.001 | 56.4±14.5 | 50.3±13.8 | 0.001 |
| TG (mg/dL) | 114.3±56.2 | 117.3±63.7 | NS | 85.7±35.9 | 87.7±51.6 | NS | 120.5±57.9 | 123.9±64.2 | NS |
| Weight (kg) | 77.2±13.2 | 78.2±13.6 | 0.003 | 74.2±13.3 | 76.2±13.8 | 0.008 | 77.9±13.1 | 78.6±13.5 | 0.042 |
HDL-C: high density lipoprotein cholesterol; LDL-C: low density lipoprotein cholesterol; T1DM: type 1 diabetes mellitus; T2DM: type 2 diabetes mellitus; n: number of patients in each group; HbA1c: glycosylated hemoglobin; SBP: systolic blood pressure; NS: not significant; DBP: diastolic blood pressure; TG: triglycerides.
After 4 years of follow-up, no statistically significant decrease was found in HbA1c values. Significant improvements were found in control of blood pressure, specifically DBP, and LDL-C. A decrease in HDL-C levels and a weight increase, both significant, were also seen.
Table 2 also shows the results of glucose, lipid, and blood pressure control for the two types of diabetes in the two periods analyzed. Maintenance of HbA1c values at 4 years, as well as an improved control of lipid (LDL-C) and blood pressure (only in T2DM) levels, was found in both types of diabetes.
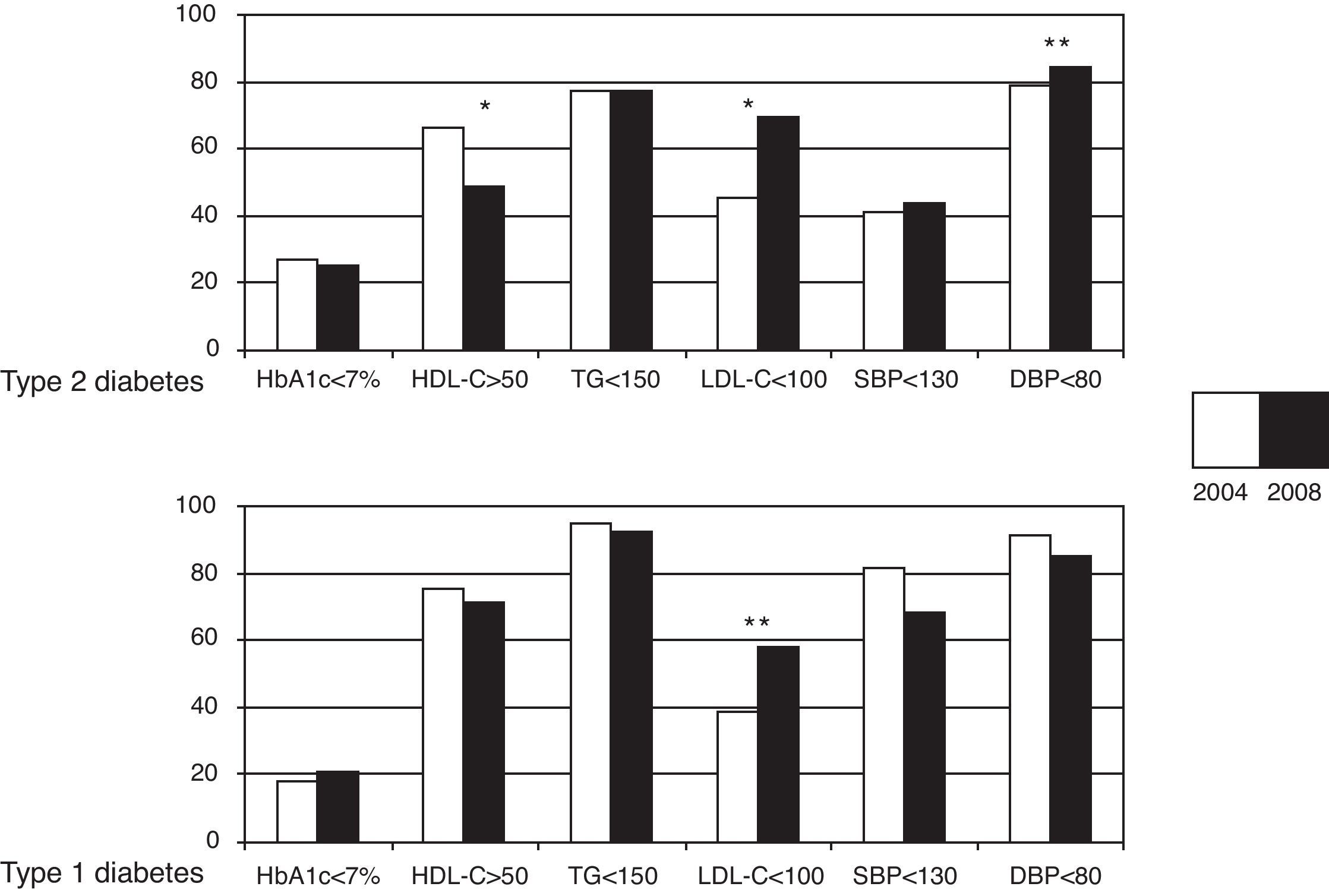
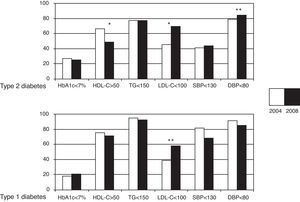
Fig. 1 shows the achievement rate of the control goals, using ADA criteria,11 for the two types of diabetes, comparing the results of 2004 and 2008. The proportion of patients with good metabolic control (HbA1c<7%) remained stable. Only a quarter of the patients from both the T1DM and T2DM groups achieved this goal. Most patients studied in 2008 (66.4%) achieved a “safe” control of diabetes with HbA1c values <8%.
Achievement of glucose, lipid, and blood pressure control goals. Comparison between 2004 and 2008 for both types of diabetes. HbA1c: glycosylated hemoglobin; HDL-C: HDL cholesterol; TG: triglycerides; LDL-C: LDL cholesterol; SBP: systolic blood pressure: DBP: diastolic blood pressure. *p<0.01; **p<0.05.
In 2008, 70.2% of T2DM patients had LDL-C levels within the recommended goal (p<0.001), and 84.5% had DBP<80mmHg (p<0.05). In the T1DM group, only 57.6% achieved the LDL-C goals, although they had significantly improved as compared to 2004. BP control goals non-significantly worsened in the 2008 analysis in the T1DM group, but goal achievement was high (87.7% had DBP<80mmHg and 68.4% SBP<130). A worsening of HDL-C results was shown for both types of diabetes, but was more significant in patients with T2DM.
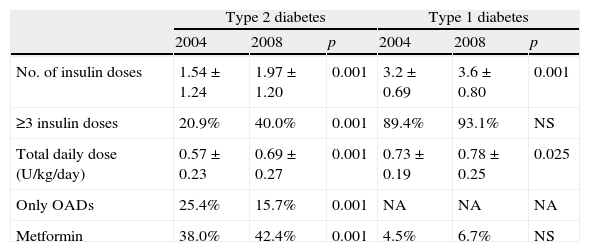
Changes in treatments used over timeTo achieve the results previously discussed, treatment patterns had become significantly more complex during these 4 years. Table 3 shows the changes in glucose lowering treatment. The number of insulin doses, the complexity of insulin regimens used, and the total daily dose increased in both T1DM and T2DM. The proportion of patients with T2DM given insulin significantly increased; in 2008, only 15% of patients used oral antidiabetics (in any combination) as the only treatment for their diabetes. The proportion of patients using metformin significantly increased to almost 50% of the study group.
Changes over time in glucose lowering treatment used for each type of diabetes.
| Type 2 diabetes | Type 1 diabetes | |||||
| 2004 | 2008 | p | 2004 | 2008 | p | |
| No. of insulin doses | 1.54±1.24 | 1.97±1.20 | 0.001 | 3.2±0.69 | 3.6±0.80 | 0.001 |
| ≥3 insulin doses | 20.9% | 40.0% | 0.001 | 89.4% | 93.1% | NS |
| Total daily dose (U/kg/day) | 0.57±0.23 | 0.69±0.27 | 0.001 | 0.73±0.19 | 0.78±0.25 | 0.025 |
| Only OADs | 25.4% | 15.7% | 0.001 | NA | NA | NA |
| Metformin | 38.0% | 42.4% | 0.001 | 4.5% | 6.7% | NS |
≥3 insulin doses: scheme with 3 or more insulin doses daily; OADs: oral antidiabetic drugs (this data refers to patients with type 2 diabetes only); Metformin: use of metformin, alone or combined with other oral antidiabetics or with insulin as insulin facilitator; NS: not significant; NA: not applicable.
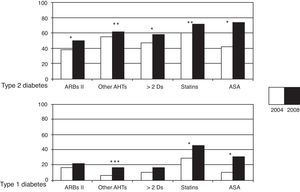
Changes in all other treatments (antihypertensive, lipid-lowering, and antiaggregant drugs) are shown in Fig. 2. Percent use of all treatments analyzed significantly increased in both the T1DM and T2DM groups. Antihypertensive treatment schemes increased in complexity in both groups. Thus, 60% of patients with T2DM and 17% of those with T1DM used more than two antihypertensive drugs. In 2008, 73.5% of patients with T2DM and 46% of those with T1DM used statins.
Changes in concomitant treatments (antihypertensive, lipid-lowering, and antiplatelet aggregant drugs) in the 4 years of follow-up for both types of diabetes. ASA: acetyl salicylic acid; ARBs: angiotensin II receptor blockers; Ds: drugs; Other AHTs: other antihypertensive drugs. *p<0.001; **p<0.01; ***p<0.05.
The greatest increase as compared to 2004 (p<0.001) was found in antiaggregant treatment, and was mainly due to the increased use of antiaggregants for primary prevention (26% in 2004 vs 57% in 2008 for the overall group, p<0.01). In secondary prevention, antiaggregant therapy was used in 95% of patients, while an additional 4.5% were on anticoagulant treatment.
DiscussionThis study demonstrated the difficulties involved in achieving an optimum control of diabetic patients in standard clinical practice in a wide group of patients. Such difficulties not only affected glucose control, but also the management of all other associated risk factors. The proportion of patients who received treatment for control of cardiovascular risk factors was high, and treatment complexity increased because of the drug combinations used.
Only 25% of diabetic patients achieved a HbA1c reduction of less than the recommended value of 7%. This proportion remained stable after 4 years of follow-up for both types of diabetes. Taking into account the length of time since the onset of diabetes in this cohort (longer than 20 years) and disease complexity (a quarter of the patients had some associated macroangiopathic or microangiopathic complication, and the prevalence of other cardiovascular risk factors was high), the final result may be considered satisfactory.
The improvement found in lipid and blood pressure control was more evident. Sixty-eight percent of patients achieved LDL-C levels<100mg/dL, and mean LDL-C values were 88.9mg/dL, 15% lower as compared to 2004. Triglyceride control remained stable during the 4 years of the study, with adequate control achieved in more than 80% of patients. DBP control also improved, although to a lesser extent, decreasing 2mmHg as compared to the previous study. In 2008, 85% of patients had DBP<80mmHg.
The results obtained in HDL-C control were less encouraging, as the proportion of patients with HDL-C levels>50mg/dL decreased (65.8% in 2004 vs 53% in 2008). Two of the potential explanations for this may be the few pharmacological resources that were available for controlling this factor and the fact that the patients, themselves, could have cooperated more in terms of improving their lifestyle habits. Increasingly sedentary lifestyles and the weight gains recorded (1kg on average as compared to 2004) may be related to this result.
The difficulty in achieving adequate metabolic control is also reflected in several recent Spanish studies. In the multicenter Melodía Study,13 conducted at 41 departments of endocrinology and nutrition in Spain which had enrolled patients with T1DM and T2DM, the results were very similar to those reported here, particularly with regard to glucose and blood pressure control. Twenty-five percent of patients had HbA1c<7%, 45.2% SBP<130mmHg, and 61.2% DBP<80mmHg. In the Roca-Rodríguez et al. study,14 conducted at Málaga and Cádiz hospitals, the achievement of metabolic control goals was assessed in T2DM patients. The proportion of patients achieving HbA1c values<7% (30.4%) was higher than in our cohort. However, as occurred in the present study, the proportion of patients with HbA1c less than 7% did not improve after 3 years of follow-up (31.7% in 2005, 30.4% in 2008).
On the other hand, in a setting different from that of specialized care, a study conducted in Ciudad Real by the ELIPSE group15 on diabetic patients attending primary care clinics reported a poorer control of cardiovascular risk factors. Only 10.2% of patients had LDL-C levels<100mg/dL, and 18.5% achieved BP values 130/85mmHg. The authors attributed these poor results to the underuse of drug treatments. It is noteworthy that more than 50% of patients in this study (51.5%) had HbA1c values<7%. The Díez Porres et al. study,16 in assessing the control of cardiovascular risk factors in T2DM in two rural areas, also found a better metabolic control, with 41% of patients achieving the HbA1c goal, but reported poorer blood pressure and lipid control (BPD<80mmHg in 53% and LDL<100mg/dL in 30%). Patients with type 2 diabetes seen in primary care possibly have a shorter disease duration and a greater pancreatic reserve, which makes adequate glucose control easier to achieve.
These results obtained in standard clinical practice provide a contrast to the clinical recommendations issued by the various scientific societies. This is found in large studies in both T1DM and T2DM. In the Swedish register of patients with type 1 diabetes, only 21.2% of patients achieved HbA1c levels<7% in the 2004 cross section.17 The US NHANES study, which included patients with both T1DM and T2DM, reported more encouraging results. HbA1c values less than 7% were achieved in 49% of patients in 2002 and in 56.8% in 2004. However, most of these patients had been suffering from diabetes for less than 14 years, and approximately 60% were being treated with oral drugs alone.18 Results have also recently been reported in Spain showing an improved control of cardiovascular risk factors and a reduction in chronic complications associated with diabetes in a group or T2DM patients followed up for 10 years (1993–2003, GEDAPS study).19
The maximum benefits in diabetes control are achieved by using a multifactorial approach, as shown by the Steno-2 study.20 In the intensive treatment arm of this study, as in our study, optimum control of cardiovascular risk factors was not achieved, but there was a 50% decrease in microvascular and macrovascular complications. Subsequent study follow-up for 5 years confirmed the persistence of these benefits, as well as a significant reduction in cardiovascular mortality.21
Glycemic control benefits in T1DM and T2DM were shown in the Diabetes Complication and Control Trial (DCCT)6 and the United Kingdom Prospective Diabetes Study (UKPDS).8 Recent studies such as ACCORD9 or ADVANCE10 have attempted to achieve more strict HbA1c goals in patients with high cardiovascular risk and longer diabetes duration. None of them showed benefits in terms of cardiovascular complications, and all-cause and cardiovascular mortality even increased in ACCORD, leading to the early termination of the study. The current trend when establishing blood glucose goals places more emphasis on the need for strict control in the first few years after diabetes onset,6,8 because this can achieve a significant reduction in morbidity and mortality and in the occurrence of complications in subsequent years (glycemic memory).7 However, in patients with cardiovascular complications or a long course of disease, the achievement of HbA1c values ranging from 7% and 8% may be safer. Overall glycemic control achieved was in line with this, according to the clinical and evolutionary profile of the study patients.
Some recently reported studies by the ACCORD group have provided clues about the actual need for the intensification of lipid22 and blood pressure23 treatment to achieve a stricter control of risk factors and thereby decrease cardiovascular events. Regarding lipid control, treatment intensification by adding fibrates to statin therapy to optimize lipid parameters does not improve results in terms of cardiovascular risk. As for blood pressure control, it has not been shown that a BP decrease to less than 120mmHg improves results as compared to a BP level lower than 140mmHg. We must therefore consider to what extent patient treatment should be complicated and to what purpose. In the future, recommendations for controlling all risk factors will possibly be individualized for each diabetic patient.
This study had some limitations. First, the proportion of patients lost from the initial cohort was greater than 10%, but the characteristics of these patients lost to follow-up were not different from those of the patients analyzed in 2008 (data not shown). Second, both patients with T1DM (a smaller sample) and patients with T2DM were included in the analysis. In fact, these were two clearly distinct groups with different demographic characteristics, as well as different risk profiles and extent of control. However, both groups showed a consistent behavior after the four-year follow-up: stabilization of glycemic control, improved lipid and blood pressure control, weight increase, and increased treatment complexity. In agreement with other studies13,18 which include both types of diabetes, we think that this study of a representative patient sample provides data which support the claim that multidisciplinary management allows for the achievement of improved mid-term, and possibly long-term, results.
It should be stressed that although significant improvements had been achieved over these four years, the patients enrolled in the study continued to have a suboptimal control of cardiovascular risk factors. We conclude, therefore, that whenever the intensification of drug treatment does not achieve a marked improvement in the goals proposed, as in our cohort, a change of treatment approach is probably indicated. An approach aimed at promoting patient responsibility and autonomy using educational, self-control, and hygienic and dietary measures, and at promoting lifestyle changes, will possibly be a very positive contribution to the achievement of better treatment compliance and improved results. We think that actual understanding of the characteristics of the diabetic population and the degree of goal achievement will help us implement changes to improve the risk profile and quality of life of patients, and decrease in the future the risk of macrovascular and microvascular disease.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Llamazares Iglesias O, et al. Control metabólico y de factores de riesgo cardiovascular en una cohorte de pacientes con diabetes mellitus. Resultados a los 4 años. Endocrinol Nutr. 2012;59(2):117–24.