Oncocytic cells tumors or oncocytomas are lesions typically located in the kidney, thyroid gland, or salivary glands, although they have been reported in other sites.1 Specifically, adrenal oncocytoma (AO) is an uncommon condition of which only some 150 cases have been reported to date.2
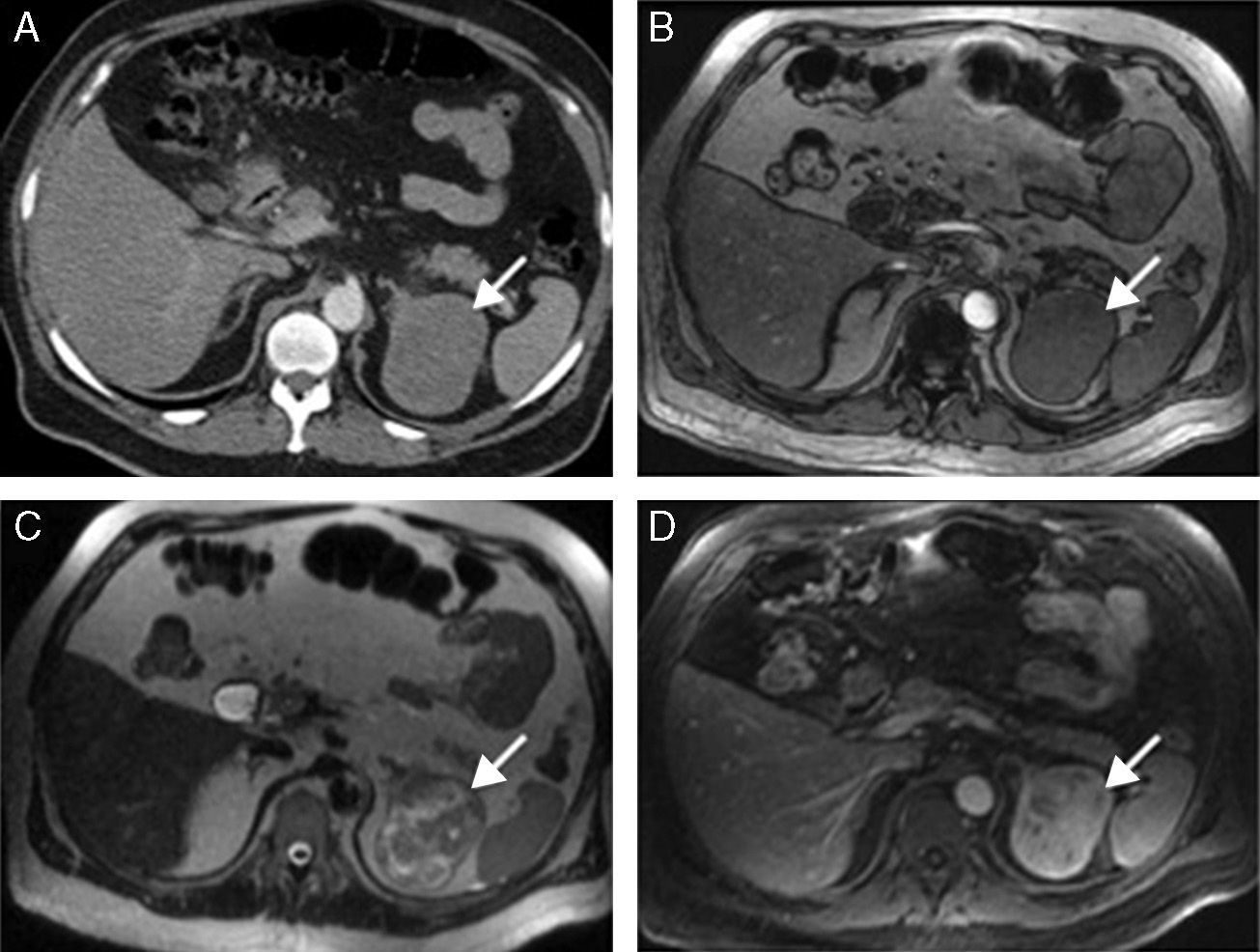
We report the case of a 61-year-old male patient with a history of HBP (high blood pressure) in whom ultrasonography performed for the presence of prostatic syndrome, increased PSA (prostrate-specific antigen) levels, and microhematuria revealed prostatic hypertrophy and a complex cystic lesion in the left kidney 5.7cm in size. A subsequent abdominal computed tomography (CT) showed an ovoid, solid, well-defined, hypodense left adrenal lesion 7cm×7cm×6.5cm in size with slight contrast uptake. As the study did not allow for the complete characterization of the lesion, magnetic resonance imaging was performed. This showed, in addition to the features seen in the CT, that the lesion was heterogeneous, isointense in T1 and hyperintense in T2, with progressive and marked contrast uptake in the dynamic study (Fig. 1), suggesting pheochromocytoma, carcinoma or adrenal hemangioma as possible diagnoses. Hormone tests were performed with the following results: basal cortisol 17.24μg/dL (normal 2.3–19.4), decreasing to 1.38μg/dL after rapid suppression (1mg dexamethasone); aldosterone/plasma renin activity ratio 18.96; DHEA sulfate 185.3ng/dL (normal 33–249); urinary excretion of epinephrine, norepinephrine, and dopamine 12.15μg/24h, 41.62μg/24h, and 249.08μg/24h, respectively (normal 1.7–22.4; 12.1–85.5; 0–1000). Catecholamines were measured once again in urine with normal results also. Scintigraphy with 131I-metaiodobenzylguanidine showed no tracer uptake by the lesion, and the carcinoembryonic antigen level was 1.11ng/mL (normal 0–3). Laparoscopic left adrenalectomy was performed through a transabdominal lateral approach. The postoperative course was uneventful, and the patient was discharged on the fourth day after surgery.
Axial CT and MRI sections centered on the adrenal region. (A) CT with intravenous contrast: hypodense, well-circumscribed left adrenal mass. (B–D) MRI images: in T1 sequences (B), the lesion is isointense on out-of-phase; in T2 sequences (C) it is heterogeneous with hyperintense areas; and in T1 sequences with intravenous gadolinium (D), the lesion shows progressive gadolinium uptake.
Histological study showed a round, well-circumscribed tumor 6cm×6cm×5cm in size of a solid appearance and brown upon sectioning, microscopically consisting of oncocytic cells (>90%), with one mitosis/50hpf and no atypical mitoses. Bleeding areas were identified. No necrosis was found. The tumor had a thin fibrous capsule with some focal image of capsular invasion, no vascular invasion and free surgical margins. Immunohistochemistry showed positivity for vimentin (intense and diffuse), melan-A (patchy), and synaptophysin (weak), while AE1-AE3, chromogranin A, and S-100 were negative. The Ki-67 index was less than 5%. According to the Lin-Weiss-Bisceglia classification,3 the lesion was an AO of uncertain malignant potential due to the presence of a minor criterion (capsular invasion).
AOs are uncommon lesions which typically occur as incidentalomas. Approximately 25% of AOs reported in the literature are malignant, but in some recent series proportions higher than 60–70% have been found.4,5 AO has been reported to be associated with hormone hypersecretion in 31.5% of patients, mainly as Cushing's syndrome, virilizing syndrome, or mimicking a pheochromocytoma.6
Grossly, AOs are usually big (8.5cm in mean size), round, well-circumscribed, encapsulated, solid, and with a brownish section, in which bleeding and/or necrosis areas may be identified. The histological feature defining these tumors is a proliferation of oncocyte cells, characterized by an increased size and granular eosinophilic cytoplasm, secondary to the accumulation of mitochondria. As regards immunophenotype, they are usually positive for vimentin, calretinin, alpha-inhibin, and melan-A, and negative for S-100 and chromogranin.7 Other markers, such as cytokeratin AE1/AE3 and synaptophysin, show a more erratic behavior, and their positivity is less common and patchy in some cases.
Although Weiss criteria8 are used to establish the malignant behavior of adrenocortical carcinomas, such criteria are not applicable to AOs; for a better stratification, the same group proposed for AOs the Lin-Weiss-Bisceglia system,3 which differentiates major criteria (>5mitoses/50hpf, the presence of atypical mitoses or venous invasion) and minor criteria (size >10cm or weight >200g, the presence of tumor necrosis, capsular or sinusoidal invasion). The presence of any major criterion classifies the tumor as malignant, while any minor criterion such as a lesion of uncertain potential and the absence of all criteria suggests a benign lesion.
The evaluation of AOs by imaging tests is complex and usually shows no specific features allowing for preoperative diagnosis.9 AOs usually occur as big, well-circumscribed lesions with a heterogeneous appearance, and the presence of signs of local invasion is uncommon. Benign AOs may however be differentiated from malignant AOs in that the latter occur as somewhat bigger lesions (9.4 vs 3.7cm) showing less enhancement after contrast administration in CT (62 vs 98HU) and less contrast washout in the late phases (12% vs 72.3%).5
As regards the treatment of these lesions, their association with hormone hypersecretion and their suspected malignancy (often derived from their size) make surgery the treatment of choice. Because of this suspected malignancy, latent in most cases, the most commonly used approach in the reported cases has been open adrenalectomy, although the use of laparoscopic surgery,10 based on the theory that a complete resection maintaining tumor capsule integrity, allows for the safe treatment of these lesions, has been reported.
Please cite this article as: Muñoz de Nova JL, García-Sanz Í, del Campo Val L, Delgado Valdueza J, Martín-Pérez E. Oncocitoma: una lesión infrecuente en la glándula suprarrenal. Endocrinol Nutr. 2015;62:144–145.