Pituitary apoplexy (PA) is an uncommon condition caused by infarction or hemorrhage in the pituitary gland, usually inside an adenoma. Acute damage leads to pituitary gland expansion and secondary compression of perisellar structures, causing neurological and endocrinological deficiencies of different severity that may become permanent and even life-threatening. The classical syndrome consists of sudden headache associated with vomiting, visual deficiency, ophthalmoplegia, and impaired consciousness.1
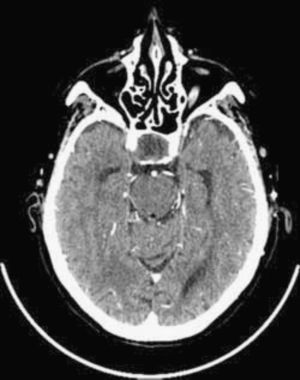
A case of pituitary apoplexy occurring after myocardial perfusion scintigraphy (SPECT) is reported here. This occurred in a 74-year-old female patient with cardiovascular risk factors who had an implanted pacemaker due to sinus disease and a history of ischemic heart disease starting 17 years previously with unstable angina. The patient had undergone percutaneous revascularization for a single coronary lesion in the anterior descending artery. Her history included a non-functioning pituitary macroadenoma diagnosed seven years before. Previous laboratory tests showed impaired pituitary function, with TSH levels of 2.6μIU/mL, T4 levels of 0.7ng/dL, and T3 levels of 2.1pg/mL three years earlier, but the patient was undergoing irregular monitoring at another center and did not receive replacement therapy. The patient reported an intolerance to acetylsalicylic acid and was being treated with ticlopidine and lorazepam. She was admitted to hospital for instable angina work-up. Treatment was started with low molecular weight heparin at a dose of 1mg/kg/kg twice daily, clopidogrel, carvedilol, nitrates, and atorvastatin, and the patient remained stable from the cardiovascular viewpoint from the start of treatment. Myocardial perfusion SPECT with Tc99 was performed at rest and after stimulus with dipyridamole on the fourth day of admission. On that day, the patient experienced malaise and nausea, and high blood pressure levels were found at the end of the test. No other changes were seen. In the ward, the patient had a BP of 160/99mmHg. In the following 24h she continued to have a feeling of nausea and vomiting and experienced high blood pressure, headache, and right ophthalmoplegia consisting of incomplete paralysis of the third cranial nerve with ptosis and mydriasis. Since magnetic resonance imaging could not be performed as the patient had an implanted pacemaker, an urgent CT scan of the head was requested to rule out bleeding complications. The scan showed a pituitary macroadenoma with no evidence of bleeding inside the tumor (Fig. 1). Laboratory tests which were performed because of a clinical suspicion of PA confirmed panhypopituitarism, showing the following values: TSH 0.61μIU/mL, T4 0.6ng/dL, T3 1.6pg/mL, cortisol 3.2μg/dL, prolactin 1ng/mL, FSH 1.7IU/mL, and LH 0.6mIU/mL. Hormone replacement therapy was therefore started with steroids at doses for acute adrenal insufficiency and levothyroxine 25μg/d. Ophthalmological examination revealed a significant visual acuity (VA) deficiency with paracentral islets in campimetry of both eyes. The patient remained hemodynamically and neurologically stable after the start of replacement therapy, but experienced recurrent angina episodes in the following days despite medical treatment, which led to the prioritization of coronary angiography over neurosurgical surgery. Three-vessel coronary disease was found, and percutaneous revascularization was performed with three stents coated with monoclonal antibodies being implanted. Because of the need to maintain double antiaggregation therapy for at least one month and neurological stability, neurosurgical surgery was delayed. Three months later, the tumor was resected through an endonasal approach with no complications. Histopathological examination revealed tissue consistent with a completely infarcted pituitary adenoma, with blood remnants and no evidence of viable tumor. Repeat ophthalmological examination at two months showed a recovery from visual deficiency, with a VA of 0.8 in both eyes, similar to that found one year before, and the disappearance of ophthalmoplegia. The patient is currently stable on hormone replacement therapy with hydrocortisone and levothyroxine.
PA is an uncommon endocrinological emergency whose pathogenesis has not been fully elucidated yet. Various theories have been proposed, from insufficient vascular supply due to high metabolic requirements2 to abnormal adenoma vascularization which makes it more susceptible to bleeding as compared to other central nervous system tumors.1 According to the reported data, most adenomas are non-functioning,3 so that PA may often be the form of presentation of a tumor not previously diagnosed. The actual incidence of PA is unknown, but it is estimated to occur in 0.6–21% of pituitary tumors.3–5 An incidental finding of pituitary hemorrhage and/or infarct in imaging tests or histopathological samples is more common, but these cases are not true PAs. PA usually occurs spontaneously, but several factors possibly contributing to its development have been reported. Thus, it has been associated with head trauma, radiotherapy, arterial hypertension or hypotension, major surgery (particularly cardiac surgery, due to blood pressure changes and anticogulant treatment), hormone stimulation tests or drug treatment with GnRH analogues, estrogens, dopamine agonists, and antiplatelet or anticoagulant drugs. PA has also been related to various diagnostic or therapeutic techniques using heparin or contrast media,6,7 but the pathophysiology of the process is unknown. This is, to our knowledge, the first case of PA reported after myocardial perfusion SPECT. The time sequence suggests that apoplexy was triggered by the procedure, maybe in relation to an unnoticed episode of arterial hypotension caused by dipyridamole. Blood pressure levels would have increased as a response to the stimulus or the stress situation, or simply due to fluctuation. A limitation of the reported case was that magnetic resonance imaging, the imaging test of choice, could not be performed.3 However, although bleeding inside the tumor was not seen in the CT scan, which has a low sensitivity to the detection of hemorrhage,3 histopathology showed the presence of blood remnants. Despite this, it would appear that a greater hemorrhagic component would have been expected in a patient on anticoagulant treatment such as the one reported, and it is a reasonable conclusion that the starting event was ischemic in nature. As regards treatment, it is generally agreed that it should initially be aimed at the control of water and electrolyte balance and the administration of hormone replacement therapy, particularly high-dose glucocorticoids. However, greater controversy exists as to which patients should undergo surgery and when. If impaired consciousness, a significant visual deficiency, or progressive symptoms exist, early surgical decompression in the first week is recommended,3,8,9 but the criteria defining a significant neuro-ophthalmological deficiency are not clear.9 In this regard, optical coherence tomograpy has emerged in recent years as a useful tool for visual diagnosis and prognosis in these patients. Visual recovery will depend on the timing of surgery, but may occur even when the surgical procedure has to be delayed.10 The fact that this occurred in our patient, in whom surgery was indicated but had to be delayed because of her concomitant cardiac disease, supports this theory. By contrast, ophthalmoplegia has a better prognosis with both conservative and surgical treatment.3 In other situations, conservative management may be adequate, but treatment should be individualized in each patient. Finally, our case report is not only intended to describe the eventual relationship of PA with the diagnostic test, but also to emphasize the importance of maintaining a high index of suspicion when making a diagnosis that continues to be essentially clinical.
Please cite this article as: Ferreira-González L, et al. Apoplejía hipofisaria tras gammagrafía de perfusión miocárdica. Endocrinol Nutr. 2012;59:606–8.