Childhood obesity is a major and increasing health problem for society because it increases the risk of cardiovascular disease, type 2 diabetes mellitus, and hypertension. Thus, when obese children become obese adults, effects on their health and life expectation may be devastating.
Objectives(1) To assess the prevalence of metabolic syndrome (MS) in a child population with obesity and (2) to compare anthropometric and biochemical parameters in patients with one or two parameters of MS syndrome to those of patients who meet MS criteria.
Patients and methodsA descriptive, cross-sectional study was conducted in children and adolescents with severe obesity (weight >p97) seen at the endocrinology department of Hospital de Getafe. Variables examined included age, sex, height, weight, body mass index (BMI), waist circumference (WC), oral glucose tolerance test (OGTT), insulin, insulin resistance (IR) measured by HOMA, triglycerides (Tg), high density lipoprotein (HDL), and systolic and diastolic blood pressure (SBP and DBP). The definition of MS in adolescents was made according to criteria of the International Diabetes Federation (IDF), 2007.
ResultsA total of 133 patients, 67 males (50.4%) and 66 females (49.6%) with a mean age of 12.17±3.27 years, were enrolled into the study. All patients were obese, with a weight greater than the 97h percentile for age and sex. Prevalence of several cardiovascular risk factors was as follows: WC ≥90th percentile for age and sex, 100%; hypertension, 26.08%; hypertriglyceridemia ≥150mg/dL, 15.94%; HDL <40mg/dL, 10.86%; fasting blood glucose levels ≥100mg/dL, 7.97%. The overall prevalence of metabolic syndrome was 19.6%. A comparison of different anthropometric and biochemical parameters in patients with 1 or 2 MS criteria to those with 3 or more criteria showed that obesity and insulin resistance were significantly greater the greater the number of MS criteria met.
Conclusions(1) Prevalence of MS in obese children and adolescents is high, (2) arterial hypertension and hypertriglyceridemia are the most prevalent metabolic changes in the population studied and (3) early intervention to control childhood obesity is essential to prevent cardiovascular morbidity and mortality in the future.
La obesidad infantil es un problema sanitario creciente y de primer orden para la sociedad, ya que aumenta el riesgo de padecer enfermedades cardiovasculares, diabetes mellitus tipo 2 e hipertensión arterial. Así, cuando los niños obesos se convierten en adultos obesos, los efectos sobre su salud y expectativas de vida pueden ser devastadores.
Objetivos1). Determinar la prevalencia de síndrome metabólico (SM) en una población infanto-juvenil con obesidad, y 2). Comparación de parámetros antropométricos y bioquímicos en pacientes con 1 o 2 parámetros de SM frente a los pacientes que cumplen criterios de SM.
Material y métodosEstudio transversal descriptivo en niños y adolescentes con obesidad (> p97) tratados en el Servicio de Endocrinología del Hospital de Getafe. Las variables estudiadas fueron: edad, sexo, talla, peso, índice de masa corporal (IMC), circunferencia de cintura (CC), glucemia basal y tras sobrecarga oral de glucosa (SOG), insulinemia, resistencia a la insulina (RI) medida mediante HOMA, triglicéridos (TG), HDL, tensión arterial sistólica y diastólica (TAS y TAD). La definición de SM en adolescentes se hizo de acuerdo a criterios de la International Diabetes Federation (IDF) de 2007.
Resultados133 pacientes, 67 varones (50,4%) y 66 mujeres (49,6%), con edad media de 12,17±3,27 años. Todos los pacientes presentaban obesidad superior al p97 para edad y sexo. La prevalencia de los distintos parámetros del SM fue la siguiente: 100% CC > p90 para edad y sexo; 26,08% hipertensión arterial; 15,94% hipertrigliceridemia superior a 150mg/dl; 10,86% HDL < 40mg/dl; 7,97% glucemia en ayunas por encima de 100mg/dl. En conjunto, la prevalencia de SM fue del 19,6%. Cuando comparamos distintos parámetros antropométricos y bioquímicos en los pacientes con 1 o 2 criterios de SM frente a los que presentan SM completo, se observa que a mayor número de criterios de SM, el grado de obesidad y la RI son significativamente mayores.
Conclusiones1). En la obesidad infanto-juvenil, la prevalencia de SM es elevada; 2). La hipertensión arterial y la hipertrigliceridemia son las alteración metabólicas más prevalentes en la población estudiada, Y 3). Es fundamental realizar una intervención temprana en el control de la obesidad infantil, como mecanismo de prevención de morbi-mortalidad cardiovascular en el futuro.
Obesity in children and adolescents is a major public health problem. Obesity is disproportionately increasing throughout the world, including poor countries where malnutrition has traditionally been the main problem. There are 110 million children with this disease, and forecasts for growth in the coming years are alarming. It is also known that 80% of children with overweight and obesity in childhood and adolescence will be obese in adulthood.1
Spain is considered the fourth leading country in the European Union with childhood obesity problems, with an estimated prevalence of 14% in children aged 2–9 years according to the EnKid study.2
Until some time ago, it was thought the children with obesity did not experience cardiovascular problems until they reached adulthood. However, we know now that children with overweight and obesity may have cardiovascular complications in the short and long term. Cardiovascular risk factors associated with childhood obesity include increased blood pressure (BP), high triglyceride (Tg) levels, decreased high density lipoprotein (HDL) levels, central obesity, and altered basal blood glucose levels. All of these risk factors are included in the definition of metabolic syndrome (MS).3
Children with obesity have a three-fold greater risk of high blood pressure (HBP) as compared to non-obese children. There are several studies which document the association of obesity and increased BP in children, and all of them have reported higher BP levels in patients with overweight/obesity when compared to children with normal weight.4
Different studies have also shown that changes in lipid metabolism are one of the risk factors for cardiovascular disease. Lipid profile in children with obesity is usually abnormal, with increased Tg and decreased HDL levels. LDL levels are usually normal, but particles are smaller, dense, and with a greater atherogenic power.5
The prevalence of type 2 diabetes mellitus (T2DM) has increased in children and adolescents in the past 20 years. In young people under 20 years of age, the estimated overall prevalence of T2DM is 0.18%, and is greater in females, according to the SEARCH study.6 The prevalence of carbohydrate intolerance in obese children and adolescents is estimated at approximately 10–30% depending on the series, while altered basal blood glucose occurs in approximately 7–15%.
The objective of our study was to assess the prevalence of the different components of MS in children and adolescents with obesity, and to compare different anthropometric and biochemical parameters between patients meeting 1 or 2 criteria for MS and those with complete MS.
Materials and methodsA descriptive cross-sectional study was conducted in 133 children and adolescents with obesity (>P97) aged 5–19 years seen at the department of endocrinology and nutrition of the Hospital de Getafe between January 2005 and January 2010. All patients attending the clinic were enrolled into the study because it was a specific clinic to which only patients with obesity, defined according to the research institute on growth and development of the Fundación Faustino Orbegozo as p>97 for age and sex, were referred.
The patients’ legal guardians, and sometimes the patients themselves, provided their informed consent for participation. The variables recorded included age, sex, height, weight, body mass index (BMI), waist circumference (WC), blood glucose, both basal and after an oral glucose tolerance test (OGTT), insulin, insulin resistance measured by HOMA, glycosylated hemoglobin (HbA1c), triglycerides (Tg), HDL, systolic blood pressure (SBP), and diastolic blood pressure (DBP).
MS was defined as the occurrence of three or more of the following cardiovascular factors (according to the 2007 International Diabetes Federation [IDF] criteria used in our study): obesity ≥P90 for age and sex, Tg ≥150mg/dL, HDL <40mg/dL, BP ≥130/85, basal blood glucose ≥100mg/dL. This definition was used because these are the established criteria for children aged 10–16 years, the age group of the majority of our patients.
All patients were evaluated at the endocrinological outpatient clinic of the hospital, and clinical and anthropometric data were collected. Weight was measured with the patients in the center of a scale in light clothing and without shoes. Height was measured with the patients standing with their backs leaning against the stadiometer of the same scale. BMI was calculated using the Quetelet formula (kg/m2).
To determine obesity based on the BMI of each patient, tables from the research institute on growth and development of the Fundación Faustino Orbegozo were used.
WC was measured, with the patients standing and with their heads in a horizontal position, at the midpoint between the lower margin of the last rib and the upper margin of the iliac crest.
BP was measured with the patients sitting with their left arm at heart level using a professional Riester sphygmomanometer manufactured in Spain. Several measurements were made, from which an average BP measurement was obtained. Values ≥130/85mmHg were considered pathological. Laboratory tests were performed at the central laboratory of the Hospital de Getafe. All patients attended the hospital after fasting for 12h.
Laboratory parameters tested included glucose, insulin, and insulin resistance measured using Homeostasis Model Assessment (HOMA).
Normal fasting blood glucose was defined as levels ranging from 60 to 100mg/dL (3.3–5.5mmol/L); values of Tg ≥150mg/dL and HDL <40mg/dL were considered pathological, as were insulin levels higher than 14microIU/mL and HOMA-IR greater than 3.5.7,8 Glucose and lipids were measured in a Cobas 711 autoanalyzer using a colorimetric enzymatic method. Insulin was measured in a Cobas 601 autoanalyzer using a sandwich ELISA assay.
SPSS 15.0 software was used for statistical analysis. Quantitative variables are given as mean and standard deviation, and dichotomic variables as percentage. Quantitative variables from patients with or without prediabetes were compared using a Student's t-test for independent samples. A value of p<0.05 was considered statistically significant.
ResultsA total of 133 patients, 67 males (50.4%) and 66 females (49.6%), with a mean age of 12.17±3.27 years were recruited. All of them were obese (>P97 for age and sex).
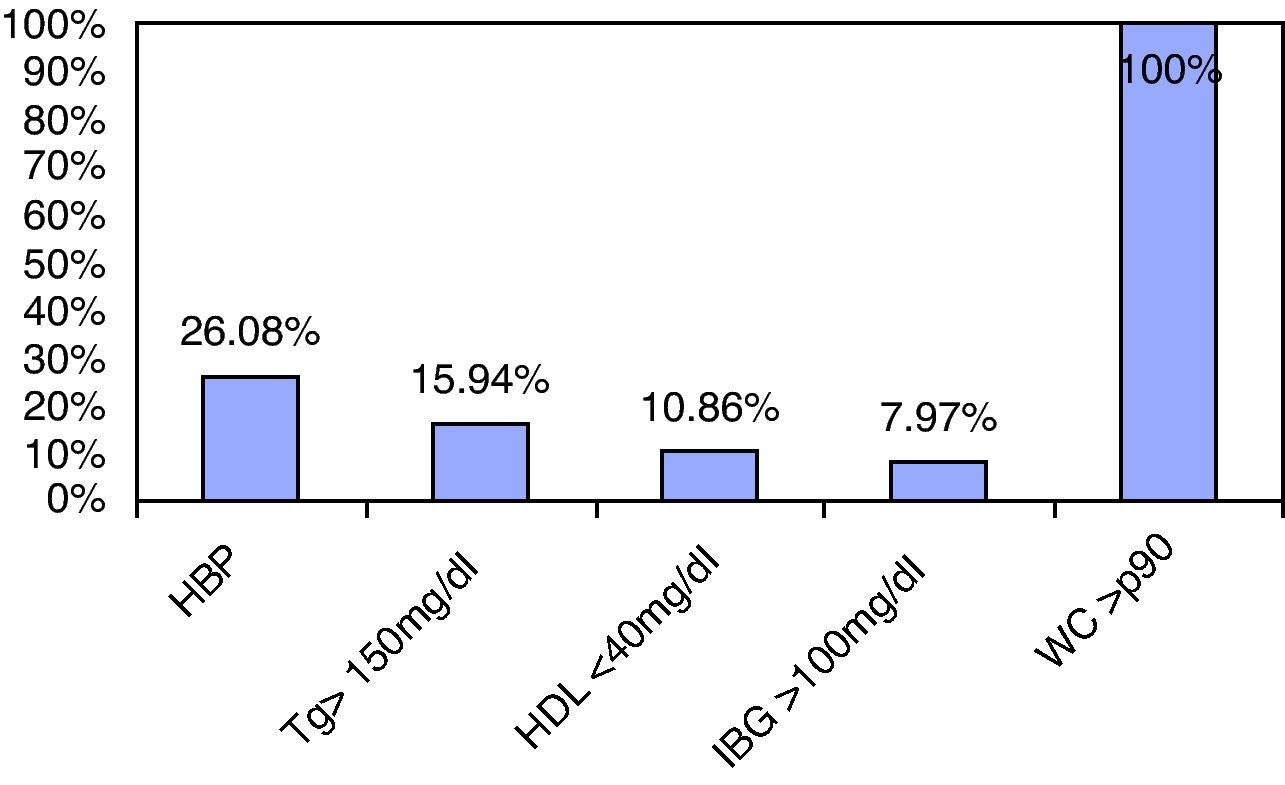
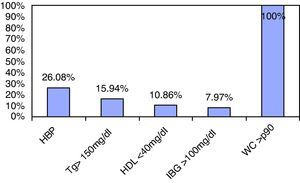
The prevalence of the different components of MS based on 2007 IDF criteria was as follows (Fig. 1):
- -
100% WC ≥P90 for age and sex.
- -
26.08% blood pressure ≥130/85.
- -
15.94% hypertriglyceridemia ≥150mg/dL.
- -
10.86% HDL <40mg/dL.
- -
7.97% fasting blood glucose ≥100mg/dL.
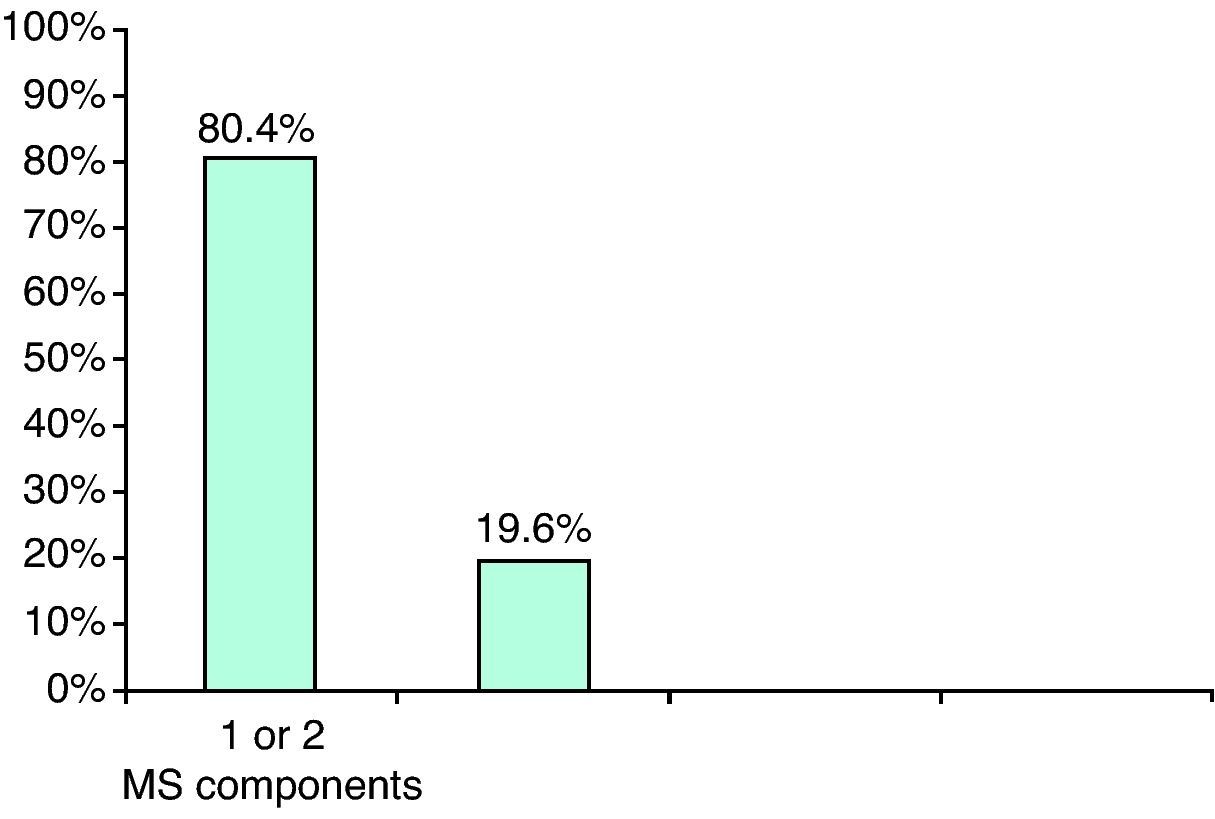
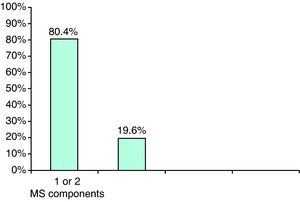
When the association of several of the components was studied, 80% of obese patients were found to have 1 or 2 MS components, and 19.6% had 3 or more MS criteria (Fig. 2).
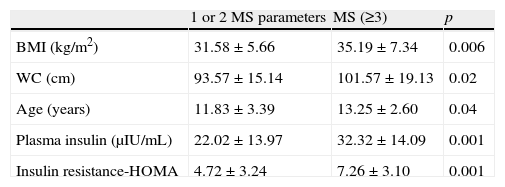
A comparison of the different anthropometric and biochemical parameters in patients with 1 or 2 MS criteria and those with complete MS (Table 1) showed that the degree of obesity and IR were significantly greater the greater the number of MS criteria (BMI 31.58±5.66 vs 35.19±7.34kg/m2, p=0.006; HOMA 4.72±3.24 vs 7.26±3.10, p=0.001).
Comparison of anthropometric and biochemical data.
| 1 or 2 MS parameters | MS (≥3) | p | |
| BMI (kg/m2) | 31.58±5.66 | 35.19±7.34 | 0.006 |
| WC (cm) | 93.57±15.14 | 101.57±19.13 | 0.02 |
| Age (years) | 11.83±3.39 | 13.25±2.60 | 0.04 |
| Plasma insulin (μIU/mL) | 22.02±13.97 | 32.32±14.09 | 0.001 |
| Insulin resistance-HOMA | 4.72±3.24 | 7.26±3.10 | 0.001 |
Overweight and obesity in children and adolescents have been associated with several cardiovascular risk factors and have been shown to be associated with the early development of atherosclerotic lesions.9 The Bogalusa Heart Study, conducted on 9167 subjects, reported that obese children had increased LDL cholesterol, triglyceride, and BP levels and low HDL levels as compared to normal subjects.10
In our study, MS prevalence was 19.6%, i.e. one out of every five patients. Other studies have reported similar MS prevalence rates ranging from 10% to 21%.11 The most prevalent component of MS, excluding abdominal circumference because all our patients were obese, was HBP, with a prevalence of 26.08% (somewhat lower than that reported by other studies [49%]), followed by hypertriglyceridemia (15.94%). Our results do not agree with those from other studies in obese children where the most prevalent component was hypertriglyceridemia, found in 54% of subjects.12
The potential mechanism underlying increases in BP values is related to visceral fat, which increases insulin resistance. This hyperinsulinemia increases renal sodium absorption, sympathetic activity, and activity of the renin-angiotensin–aldosterone system (RAAS), which contributes to increased BP.13
Different studies have shown that the impaired metabolism of plasma lipoproteins in childhood and adolescence is another cardiovascular risk factor. There are pathological studies showing a positive correlation of LDL and Tg with the extent of early atherosclerotic lesions in adolescents and young adults, as well as a negative correlation with HDL cholesterol levels. In our study, one out of every 10 children had HDL levels less than 40mg/dL, and almost two out of every 10 children had high triglyceride levels. Insulin resistance of lipoprotein lipase in peripheral tissue may contribute to increased triglyceride levels and may be responsible for decreased HDL levels through an increase in the extent of Apo1/HDL-C degradation as compared to its synthesis.14
The earliest change associated with central obesity is probably related to carbohydrate metabolism. This is a progressive change, ranging from the occurrence of hyperinsulinism, associated or not with insulin resistance, to T2DM, with intermediate stages of impaired basal blood glucose and carbohydrate intolerance (CHI).15 The prevalence of impaired blood glucose (IBG) measured in our study was somewhat higher as compared to other European studies conducted on adolescent obese populations. One of these, published in 2008 by Felszeghy et al.16 and conducted on 250 Caucasian, severely obese subjects with a mean age of 13 years, found a 4.4% prevalence of IBG. An additional study conducted in Italy on 710 obese patients aged 6–18 years reported a 4.5% prevalence.17
Finally, it should be noted that the prevention and early management of the different MS components in childhood and adolescence is of the utmost importance because multiple studies have shown these parameters to be associated with a greater cardiovascular risk in adult age. Adults who were obese as children have a higher prevalence of cardiovascular risk factors such as HBP or hypertriglyceridemia as compared to those who had a normal weight in childhood.
Effort should be aimed at fighting obesity, physical inactivity, or poor diet in childhood. This is the only way to prevent adolescents from growing up into unhealthy adults.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Guijarro de Armas MG, et al. Prevalencia de síndrome metabólico en una población de niños y adolescentes con obesidad. Endocrinol Nutr. 2012;59:155–9.