We report the case of a 53-year-old woman with a personal history of chronic venous insufficiency and recurrent biliary colic who was seen after goiter was detected at during routine medical visit. A physical examination revealed diffuse grade 3 goiter associated with two to four bilateral hard nodules attached to deep planes. There were no adenopathies. No thyroid tenderness or other findings were made during the physical examination. Laboratory test results included: liver enzymes: GOT, 69IU/L; GPT, 53 UI/L; GGT, 360IU/L; AP, 2429IU/L. Thyroid hormones: TSH, 4.16μU/mL; FT4, 1.07ng/dL. Anti-thyroid antibodies (anti-thyroglobulin and anti-thyroperoxidase): negative. Acute phase reactants: C-reactive protein, 33.5mg/L; ESR: 73mm/h.
Thyroid ultrasound examination: four solid, hypoechoic, non-vascularized nodules 2–5cm in size were seen, two in each nodule. The predominant nodule, 5cm in size, was found in the middle portion of the right lobe. Fine needle aspiration: puncture of the dominant nodule was inadequate for cytological study. The patient was therefore referred for endocrine surgery because of nodule size. During surgery, a mass of a woody consistency was found, closely adherent to adjacent tissues, which prevented complete resection. Pathological study of surgical specimen. Gross examination: left lobe: brown whitish triangular fragment 1.5cm in size of elastic consistency, with no normal thyroid tissue upon sectioning.
Right lobe: triangular fragment 1.5cm in size with similar characteristics to the left fragment. Immunohistochemistry: CD-3 and CD-20: positive scattered lymphoid infiltrate.
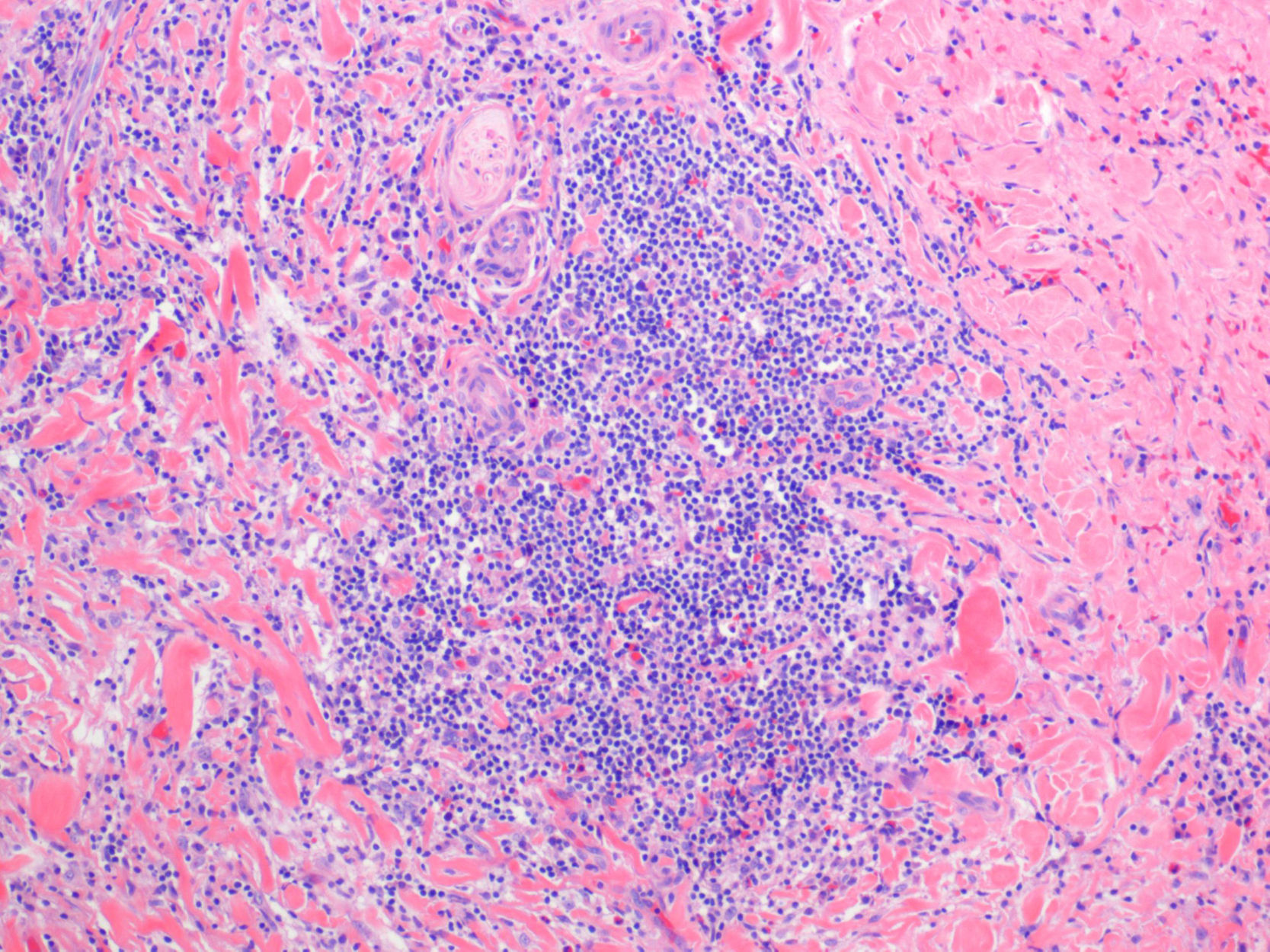
Kappa and lambda light chains: positive in plasmacellular infiltrate. Cytokeratin pan: negative. Thyroglobulin: positivity for vestiges of thyroid follicles. Microscopic examination: sections showed thyroid tissue in both lobes to be widely replaced by collagenized fibrous tissue, marked thyroid follicle atrophy, and marked infiltration of mononuclear inflammatory cells (Fig. 1). CT of the neck: diffuse decrease of usual density of thyroid parenchyma, with no invasion of adjacent tissues. Based on these findings in supplemental tests, Riedel's thyroiditis was diagnosed.
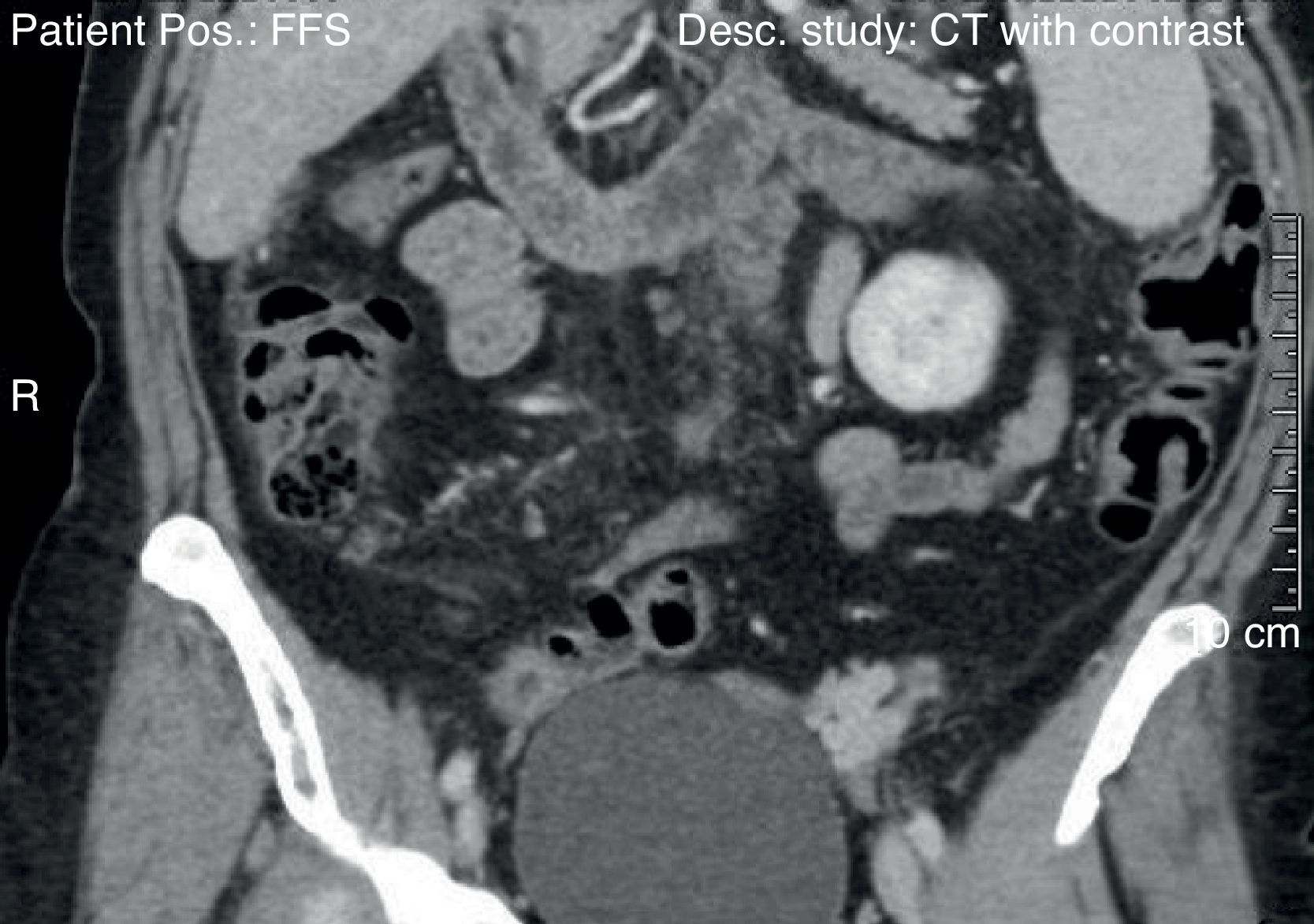
In parallel to thyroid work-up, and based on recurrent episodes of biliary colic, renal colic and urinary infection, associated with intermittent claudication and chronic venous insufficiency, the internal medicine department performed a CT scan of the abdomen and pelvis that revealed portal thrombosis with abundant esophageal varices and peridiaphragmatic, perisplenic, and pericolonic collaterals; moderate splenomegaly and a small splenic cyst; right renal atrophy, fibrosis of intrarenal excretory system and right ureter entrapment; distal retroperitoneal and periaortic presacral fibrosis and fibrosis around the iliac vessels with complete obstruction of the iliac and collateral veins through prominent gonadal veins (Fig. 2).
As regards liver involvement, biliary cirrhosis (stage A 5–6) was shown, with portal thrombosis that is still present. Anticoagulation was ruled out because of two episodes of upper gastrointestinal bleeding and melena secondary to rupture of esophageal varices that required hospital admission.
Based on these findings, treatment with prednisone (40mg/24h in a cyclic scheme) and tamoxifen (20mg/day) was prescribed. Two years later, thyroid ultrasound examination showed a significant reduction of the size of the thyroid nodules (which became subcentimetric), a marked improvement of fibrosis in CT, and subclinical hypothyroidism that required treatment with levothyroxine 50mcg/day. It should be noted that cholestatic parameters evolved to total normalization after treatment with glucocorticoids and tamoxifen was started.
Currently, the patient is only being treated with levothyroxine 75mcg/day. Treatment with glucocorticoids and tamoxifen is not required.
Riedel's disease, also called thyroid fibrosclerosis or fibrosing thyroiditis, is a chronic inflammatory thyroid disease characterized by the replacement of gland parenchyma by fibrous tissue that extends to adjacent structures. The inflammatory infiltrate is a conglomerate of T and B cells, macrophages, eosinophils, and extracellular proteins. Its incidence and prevalence are both low. Its prevalence has been estimated at approximately 0.05% of thyroidectomies, and is four times more common in women aged 30–50 years.1
Considerable controversy exists regarding its etiology, and there are currently two different views. On the one hand, some authors think that it is an autoimmune condition, a variant of Hashimoto thyroiditis or the last stage of De Quervain thyroiditis, based on the presence of anti-thyroid antibodies in approximately 40–70% of patients and the frequent coexistence of other autoimmune diseases such as Graves’ or Addison's disease and pernicious anemia. On the other hand, there are also authors who think that it is a part of a systemic process of fibrosclerosis characterized by fibroblast proliferation through cytokines such as transforming growth factor beta. This contention is supported by the occasional association of retroperitoneal and mediastinal fibrosis, sclerosing cholangitis, and orbital pseudotumor.2
The most common clinical sign is the rapid growth of the thyroid gland, which acquires a stony consistency, eventually causing compressive symptoms such as dysphagia, dysphonia, and dyspnea. The fact that this is the first and virtually the only clinical sign leads the physician to first consider a diagnosis of thyroid lymphoma or anaplastic carcinoma, because these are conditions with a greater incidence and prevalence as compared to fibrosing thyroiditis3 or other benign diseases such as subacute De Quervain's thyroiditis or the fibrous variant of Hashimoto's thyroiditis.4,5 However, it should be noted that, unlike in lymphoma, in particular, and in anaplastic carcinoma, lymph nodes are not involved in Riedel's disease.
Laboratory findings do not provide clear indications, because most of the patients have a normal thyroid function, and may show indirect evidence of a systemic fibrosclerosis process with the involvement of other systems. No specific findings are made using ultrasound and subsequent fine needle aspiration, because the sample is inadequate for cytological study in nearly all cases.6
Surgical resection and pathological examination of the surgical specimen are therefore required for final diagnosis because in Riedel's thyroiditis there is an infiltration of thyroid tissue by a conglomerate of eosinophils, T and B cells, and fibroblasts, an absence of necrosis and anaplastic cells (ruling out lymphoma, sarcoma, and anaplastic cancer), an absence of Hürthle cells or oncocytes (ruling out the fibrous variant of Hashimoto's thyroiditis), and an absence of giant cells (ruling out De Quervain's thyroiditis).7
There are no clinical trials on the treatment of this rare disease. Small-scale studies and case series have reported a good response to glucocorticoids8,9 because they decrease progressive infiltration, fibrosis, and the destruction of adjacent structures, and also to tamoxifen, an antiestrogen used for breast cancer with fibrosis-inhibiting properties, which acts as a modulator of transforming growth factor beta, promoting the production of extracellular tissue and fibrosis, decreasing mass size by 50% or more, and sometimes achieving complete resolution of the disease.10
The diagnosis of Riedel's thyroiditis is therefore difficult in that it is only made after other more prevalent conditions have been ruled out and because partial or total thyroid gland resection is required.
Conflicts of interestThe authors state that they have no conflicts of interest.
☆ Please cite this article as: Jiménez Varo I, et al. Infiltración linfocitaria progresiva tiroidea en paciente con hepatopatía crónica. Endocrinol Nutr. 2013;60:98–100.