Primary hyperparathyroidism (PHPT) is due to a single adenoma in 85–5% of cases, and is often cured after adenoma removal. Intraoperative rapid determination of intact parathyroid hormone (PTHio) may be a tool for monitoring the effectiveness of PHPT surgery. The main objective of our study was to evaluate PTHio determination and to establish whether its successful implementation contributed to achieve minimally invasive surgery (MIS) and major ambulatory surgery (MAS) in the treatment of PHPT.
Materials and methodsRetrospective study of a consecutive series of patients diagnosed and operated on for PHPT at the University General Hospital of Ciudad Real between January 2005 and January 2012.
ResultsIn the study period, 91 patients underwent surgery: 39 (42.9%) under general anesthesia, while 52 (57.1%) were candidates for regional anesthesia by cervical block. Seventy-six out of 91 patients (83.5%) were amenable to MIS using a unilateral approach. Classical cervicotomy was performed in all other patients. PTHio determination was done in 75 patients, showing cure in the same surgery in 68 of them. MAS was performed in 70.3% (64) of the patients.
ConclusionsDetermination of PTHio may allow for changing the surgical approach to PHPT at our department, allowing for performance of MIS on an outpatient basis in a significant proportion of patients with some cosmetic improvement, probably less pain, shorter hospital stay, and less potential complications than bilateral cervical exploration.
El hiperparatiroidismo primario (HPTP) se debe a un adenoma único en el 85–95% de las ocasiones, lográndose frecuentemente la curación con la extirpación del mismo. La determinación rápida intraoperatoria de la paratirina intacta (PTHio) puede constituir una herramienta para el control de la efectividad de la cirugía del HPTP. El objetivo principal de nuestro estudio fue evaluar la determinación de PTHio y objetivar si su implementación colaboraba en lograr la aplicación de una cirugía mínimamente invasiva (CMI) y en régimen de cirugía mayor ambulatoria (CMA) en el tratamiento del HPTP.
Material y métodosEstudio retrospectivo de una serie consecutiva de pacientes diagnosticados e intervenidos quirúrgicamente de HPTP en el Hospital General Universitario de Ciudad Real entre enero de 2005 y enero de 2012.
ResultadosEn el periodo estudiado, se intervinieron 91 pacientes. 39 (42,9%) fueron intervenidos bajo anestesia general y 52 (57,1%) fueron candidatos a anestesia locorregional mediante bloqueo cervical. Del total, 76 (83,5%) fueron subsidiarios de CMI con abordaje unilateral. En el resto se realizó cervicotomía clásica. En 75 pacientes se realizó la determinación de PTHio, de los cuales, en 68 se demostró curación en el mismo acto quirúrgico. El 70,3% (64) de los pacientes fueron intervenidos en régimen de CMA.
ConclusionesLa determinación de PTHio puede permitir modificar la estrategia quirúrgica del HPTP en nuestro servicio, colaborando en la realización de una CMI en un porcentaje importante de pacientes, de forma ambulatoria, con alguna mejora estética, probablemente menor dolor, menor ingreso y con menos complicaciones potenciales que en la exploración cervical bilateral.
Primary hyperparathyroidism (PHPT) is the most common cause of hypercalcemia in the general population, with an estimated annual incidence of 0.1–0.3/1000 inhabitants.1
PHPT is a condition caused by a single adenoma in approximately 85–95% of cases, and is usually cured after adenoma resection.2,3 It is usually suspected in routine laboratory tests including calcium and phosphorus measurement, and most patients have little or no symptoms.4 According to the Third International Workshop on the Management of Primary Hyperparathyroidism, there is general agreement that parathyroidectomy may be adequate in this group of patients.5,6
For many years, the standard surgical approach was bilateral neck exploration, with all the parathyroid glands being evaluated in order to identify the pathological glands. This procedure was used because there was no reliable way of differentiating multi-gland disease (15%) from single-gland disease or single adenoma before surgery.7,8
In the past decade, the availability of modern radiotracers has allowed for the use of less aggressive treatments to cure the disease.999mTc-sestamibi scintigraphy has 80–100% sensitivity for adenoma and 0–100% sensitivity for hyperplasia. If scintigraphy shows a single uptake site, unilateral exploration may be adequate for patient treatment.10,11
On the other hand, methods to measure intact parathormone (iPTH) levels intraoperatively (ioPTH) have become a complement to the development of minimally invasive surgery (MIS) because they allow the effectiveness of the surgical procedure to be confirmed by documenting decreases in plasma iPTH levels. This methodology, combined with locoregional anesthesia and a unilateral approach, will facilitate the inclusion of patients in major ambulatory surgery (MAS) programs and so allow for ambulatory treatment of this disease.12,13 Minimally invasive parathyroidectomy (MIP) can cure patients of their disease with results which are just as reliable as when all four glands are explored but without hospital admission, a wide incision, or general anesthesia being required.14 In other words, this procedure should be an alternative to traditional surgery, in an attempt to improve its results.
The lateral approach to the area where the adenoma is located, as determined before surgery by scintigraphy or ultrasound examination, allows for more direct access and provides better cosmetic results. An approximately 2-cm long incision, lateral to the medial margin of the sternocleidomastoid muscle, is made. This results in less postoperative pain and a shorter hospital stay, with a probable earlier return to work and, therefore, lower costs.15,16
The primary objective of our study was to assess ioPTH measurement and to ascertain whether its use contributes to the performance of MIS as MAS for the treatment of PHPT.
Patients and methodsA descriptive, observational, retrospective study was conducted of the clinical histories of 91 patients diagnosed with and undergoing surgery for PHPT at Hospital General Universitario in Ciudad Real from January 2005 to January 2012.
Patients with preoperative location and findings from 99mTc-sestamibi scintigraphy and/or ultrasound examination suggesting adenoma were selected.
Patients with suspected multiple endocrine neoplasia (MEN), significant associated thyroid disease, or secondary or tertiary HPT were excluded from the study. Patients with preoperative images not consistent with a single adenoma were also excluded.
The patients underwent surgery under general anesthesia or locoregional anesthesia using selective cervical plexus block.
Cervical plexus block consists of both deep and superficial blocks. In deep cervical plexus block, spinal nerves C2, C3, and C4 are anesthetized with 0.5% levobupivacaine. The superficial cervical plexus is blocked in the posterior triangle of the neck as it emerges adjacent to the midpoint of the posterior margin of the middle third of the sternocleidomastoid muscle with a 0.25% levobupivacaine dilution. This was combined with mild sedation with midazolam to ensure patient relaxation.
The surgical approach consisted of the classical Kocher cervicotomy or unilateral access through an incision of approximately 2–3cm, taking as reference the medial margin of the sternocleidomastoid muscle.
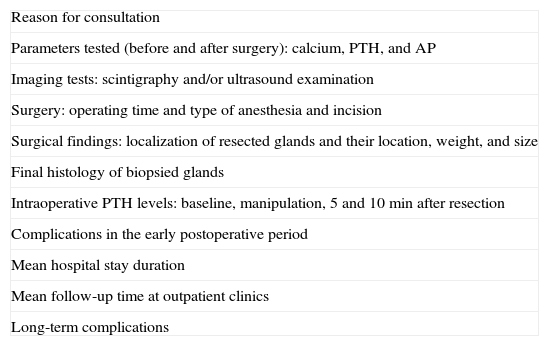
Table 1 shows the variables analyzed in our study.
Variables analyzed in the study.
| Reason for consultation |
| Parameters tested (before and after surgery): calcium, PTH, and AP |
| Imaging tests: scintigraphy and/or ultrasound examination |
| Surgery: operating time and type of anesthesia and incision |
| Surgical findings: localization of resected glands and their location, weight, and size |
| Final histology of biopsied glands |
| Intraoperative PTH levels: baseline, manipulation, 5 and 10min after resection |
| Complications in the early postoperative period |
| Mean hospital stay duration |
| Mean follow-up time at outpatient clinics |
| Long-term complications |
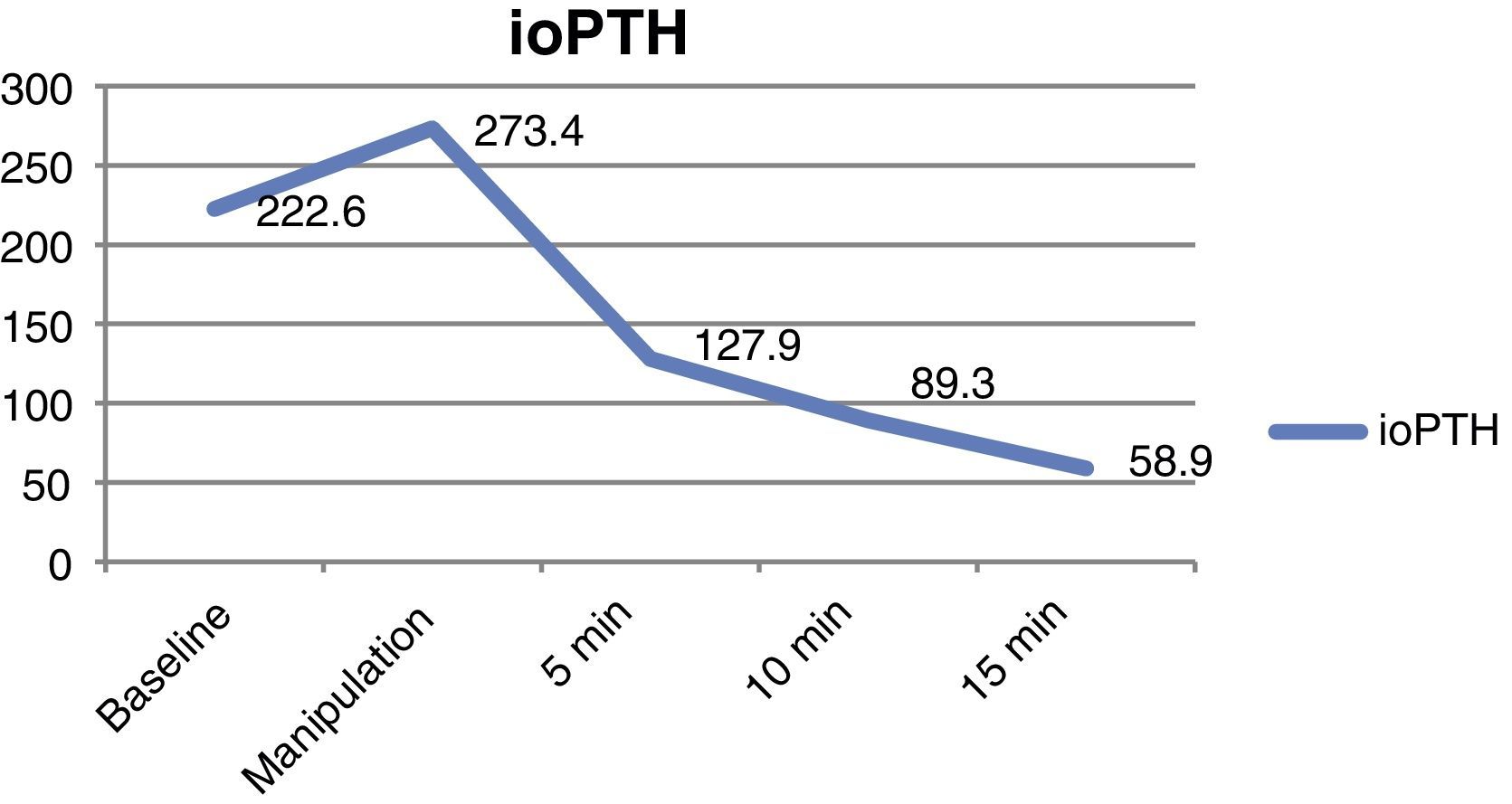
Intraoperative PTH measurement was performed using immunochemiluminescence (STAT-System; Future Diagnostic), which tests iPTH levels in venous samples taken during manipulation, 5 and 10min after adenoma resection. Its results were compared to baseline patient levels. The Miami criterion, which considers the test valid when iPTH decreases by ≥50% as compared to the maximum levels reached, was used to confirm adequate iPTH decrease.17,18
The normality of the study variables was assessed using graphic (histogram and quantile–quantile [Q–Q] plots) and statistical (Kolmogorov–Smirnov test) methods.
The descriptive statistical analysis for qualitative variables was defined using a frequency distribution table (95% confidence intervals). Quantitative variables were analyzed using statistical measures of central tendency (mean, mode, median) and dispersion (standard deviation).
Student's t and ANOVA tests were used to compare means, and a Chi-square test was used to compare proportions.
Data were analyzed using SPSS version 18.0 for Windows software.
ResultsOf the 91 patients who underwent surgery for PHPT, 76 (83.5%) were women and 15 (16.5%) were men, with a mean age of 57 years (13–87).
Thirty-nine patients (42.9%) were symptom-free at the time of diagnosis, which was incidentally made based on routine laboratory tests. All other patients had the following symptoms, some of them not clearly related to PHPT, in descending order of frequency: 12 patients (13.2%) initially had renal stones and colic, 11 (12.1%) urinary frequency and polydipsia, 6 (6.6%) osteoporosis, 6 (6.6%) asthenia and anorexia, 4 (4.4%) myalgia, 2 (2.2%) dysphagia and dysphonia, and one (1.1%) high blood pressure.
Mean preoperative calcium, PTH, and alkaline phosphatase levels were 11.15 (±0.73)mg/dL, 184.12 (±110.92)pg/mL, and 113.79 (±74.95)U/L respectively.
All patients underwent scintigraphy, and 63 also underwent parathyroid gland ultrasound as a preoperative location method.
Surgery was performed under general anesthesia in 39 patients (42.9%), and under locoregional anesthesia using selective cervical block in 52 patients (57.1%). As regards the surgical procedure, 15 patients (16.5%) underwent a classical Kocher cervicotomy and 76 (83.5%) minimally invasive surgery using a unilateral approach. Conversion to the standard transverse cervicotomy to explore glands of both sides was required in seven (7.69%) of the latter patients because no decrease in iPTH meeting the Miami criterion was found.
Mean operating time in patients with the classical cervicotomy approach was 82.3 (±25.78)min, as compared to 51.67 (±11.2)min in patients undergoing minimally invasive exploration.
With regard to location, the right upper gland was resected in 6 patients (6.6%), the left upper gland in 7 (7.7%), the right lower gland in 42 (46.15%), and the left lower gland in 34 (37.36%). One patient each had the pathological gland in the superior mediastinum and the thymus gland respectively.
Mean gland weight was 64.63 (±11.81)mg, and mean gland size was 7.133 (±1.91)mm.
The final histological study showed that the probable cause of PHPT was adenoma in 86 patients (93.5%) and hyperplasia in 5 (6.5%).
The measurement of ioPTH was performed in 75 of the 91 patients. A greater than 50% drop in the PTH curve at 10min as compared to baseline was found in 68 patients (90.6%). This met the Miami criterion, and the patients were therefore considered to be cured at surgery. Fig. 1 shows the mean decreases in the PTH curve. ioPTH was not measured in the remaining 16 patients due to surgeon preference.
MAS was performed in 64 (70.3%) of the patients, while the remaining 27 (29.7%) were admitted to hospital as usual. The mean duration of hospital stay was 12h in patients undergoing MAS and 46.7h in those admitted to the hospitalization ward. The mean hospital stay of the whole series was estimated at 21.12h.
The mean follow-up time of patients at the general surgery outpatient clinic was 1.38 (±0.518) months. Patients were subsequently seen at the endocrinology department, with the following mean postoperative values found at 6 months after the procedure: calcium, 9.50 (±0.86)mg/dL; PTH, 60.12 (±45.33)pg/mL, and alkaline phosphatase, 83.31 (±29.46)U/L.
The complications seen were considered to be mild. In the early postoperative period, six patients experienced transient hypocalcemia, four moderate neck pain, one dysphagia, and two dysphonia. All these complications occurred in patients undergoing bilateral parathyroid gland exploration. Late complications included dysphonia in a patient attending the otolaryngology department after cervicotomy with bilateral exploration and hypercalcemia in three patients six months after surgery despite the finding of an intraoperative PTH decrease meeting the Miami criterion. This was probably due to the fact that the disease was manifested as an adenoma and was actually a hyperplastic disease. Finally, four patients required repeat surgery for persistent symptoms, two of them because of hyperplastic remnants and the other two due to the diagnosis of a second adenoma.
DiscussionParathyroidectomy has become one of the most commonly performed endocrine surgical procedures, because PHPT is the most frequent endocrine disease after diabetes mellitus and thyroid disease. The surgical approach to PHPT was initially based on simultaneous diagnosis and treatment of the disease, which required comprehensive cervical exploration.19 Most endocrine surgeons traditionally performed in all patients a complete bilateral cervical exploration of the four parathyroid glands and the two recurrent laryngeal nerves, and preoperative localization studies were seldom performed. These were reserved for repeat surgery due to recurrent or persistent disease.9,20
The use of unilateral exploration by the surgeon depends on an adequate preoperative localization work-up study. Until the development of the new scintigraphic techniques, standard radiographic procedures for detecting parathyroid disease such as ultrasound examination, computed tomography or MRI had little value, mainly because of their low sensitivity and the need for a radiologist highly experienced in the interpretation of these gland disorders. However, the development of modern cationic radiotracers such as 99mTc-sestamibi and 99mTc-tetrofosmin has made it possible to improve the study of anatomical and functional localization, and to differentiate single- from multi-gland disease.9,10,21 This has allowed for a less aggressive surgical approach to resection in single-gland disease located before surgery. Less invasive surgical procedures appear to decrease operating time and risk, as well as the extent of the dissection, with the resultant advantages in the postoperative period. In addition, the surgeon may approach the site of the lesion to resect pathological glands and to locate ectopic and hyperplastic glands or multiple adenomas, which are the main cause of surgical failure, thus decreasing the number of repeat surgeries, which are associated with increased morbidity. An added advantage is that the image obtained does not depend so much on the examiner as on other techniques such as ultrasound examination. Computed tomography, MRI, arteriography, or selective PTH venous sampling are usually reserved for patients in whom other localization techniques have been inadequate or conflicting. Most authors agree that the proportion of adenomas identified is greater when two imaging tests such as scintigraphy and ultrasound examination are used.5,6,22,23ioPTH was measured in 75 of our patients. A drop in the PTH curve meeting the Miami criterion was found in 68 patients, who were therefore considered to be cured.
The importance of this measurement lies in the opportunity to perform during surgery a test confirming that the procedure has been effective. Other procedures to assess the adequate resection of abnormal parathyroid tissue, such as nuclear probe and sestamibi scintigraphy, have been reported. The measurement of ioPTH has the highest sensitivity, positive predictive value, and accuracy of all the perioperative complements used in parathyroid surgery. According to an international survey, this measurement is currently used by 68% of surgeons.24 For many authors, ioPTH measurement is, combined with imaging tests, one of the mainstays of MIS. Many authors currently advocate a switch from the traditional paradigm of bilateral exploration in PHPT surgery to unilateral exploration as a more adequate surgical approach when a single altered gland is located before surgery.25,26
The advantages of MIS include the reduction in operating time and hospital stay; the use of local or locoregional anesthesia, thus decreasing pharyngeal discomfort from orotracheal intubation and anesthesia recovery time; the reduction of the risks of recurrent laryngeal nerve damage and hypocalcemia; surgery limited to the involved side, decreased incision length and, thus, decreased postoperative inflammatory reaction; outpatient surgery; and cost reduction. This approach therefore is an attractive alternative for the patient.27,28
In our department, a unilateral approach was used in 80.46% of operated patients (70), which agrees with reports from other authors, who performed it in 60–74% of cases. MAS was performed in 68.97% of patients (60), while the remaining 29.89% were admitted to the hospital ward.
MAS allows patients to be discharged on the same day of surgery, once they have been evaluated and found to meet the basic criteria for discharge, which include the following: no symptoms of hypocalcemia, adequate ambulation, spontaneous micturition, no intractable pain, scar in good condition, good oral tolerance, and vital signs within normal limits. The patients are given a written report, the complications they may have and the situations in which they should attend the emergency room are explained to them, and they complete a satisfaction survey.29,30 Early complications are uncommon and mild, including postoperative bleeding after MIP which is usually self-limited and occurs in the first 6–8 hours.31 Various authors have shown that patients undergoing MIP have less risk of developing hematoma affecting the airway because of the small volume of dissection performed in the neck. Results are comparable to those of bilateral parathyroidectomy in terms of cure and recurrence, and superior in terms of duration, aggressiveness, and postoperative stay and hypocalcemia.32
All the complications seen in our patients were considered mild and occurred in patients in whom bilateral neck exploration under general anesthesia had been performed. No bleeding occurred in the early postoperative period. Six patients (6.6%) had transient, non-significant hypocalcemia that required no treatment, while four patients reported neck pain not related to cervical block, one reported dysphagia, and two patients experienced dysphonia. Only one of these patients continued to have dysphonia in long-term follow-up.
We therefore conclude that intraoperative iPTH measurement is a helpful surgical strategy for PHPT at a second-level hospital, allowing for minimally invasive parathyroidectomy in an outpatient setting. The limitations of our study include its retrospective nature and short follow-up period. However, we think that this procedure may be considered safe and effective in selected cases, as it decreases the complications derived from bilateral exploration and achieves excellent results and low patient morbidity.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: García-Santos EP, Martín-Fernández J, Gil-Rendo A, Menchén-Trujillo B, Martínez de Paz F, Manzanares-Campillo MC, et al. Determinación rápida intraoperatoria de la paratirina intacta en la cirugía del hiperparatiroidismo primario. La experiencia en nuestro centro. Endocrinol Nutr. 2014;61:3–8.