The thyroid gland is an uncommon site for distant metastases from extra-cervical tumors. Malignant melanoma and kidney, lung, breast, and gastrointestinal carcinomas are the most common origins of these rare metastases. We report the case of a patient with rapidly progressive thyroid metastasis from a lobular breast carcinoma operated on three years previously.
An 83-year-old female patient underwent surgery in 2007 for a breast tumor by left radical mastectomy and axillary lymphadenectomy. The pathological report confirmed a grade 2, infiltrating lobular carcinoma 5cm×4.5cm×4.5cm in size with no involvement of surgical margins and no tumor infiltration in resected lymph nodes (pT2N0). Estrogen receptor expression was 20% and progesterone expression was 5%. Treatment was therefore started with aromatase inhibitors. Subsequent oncological monitoring showed no tumor recurrence.
Three years after surgery, the patient experienced for one month a progressive dyspnea which worsened in a supine position, with no cough, expectoration, or fever. She reported a parallel neck enlargement with cervical tightness. Chest X-rays performed in the emergency room showed no evidence of cardiopulmonary disease, but a tracheal displacement suggesting goiter. Computed tomography (CT) of the neck was therefore performed. The CT scan confirmed the presence of a large multinodular goiter with severe tracheal stenosis (Fig. 1), after which the patient was referred to the endocrinology outpatient clinic.
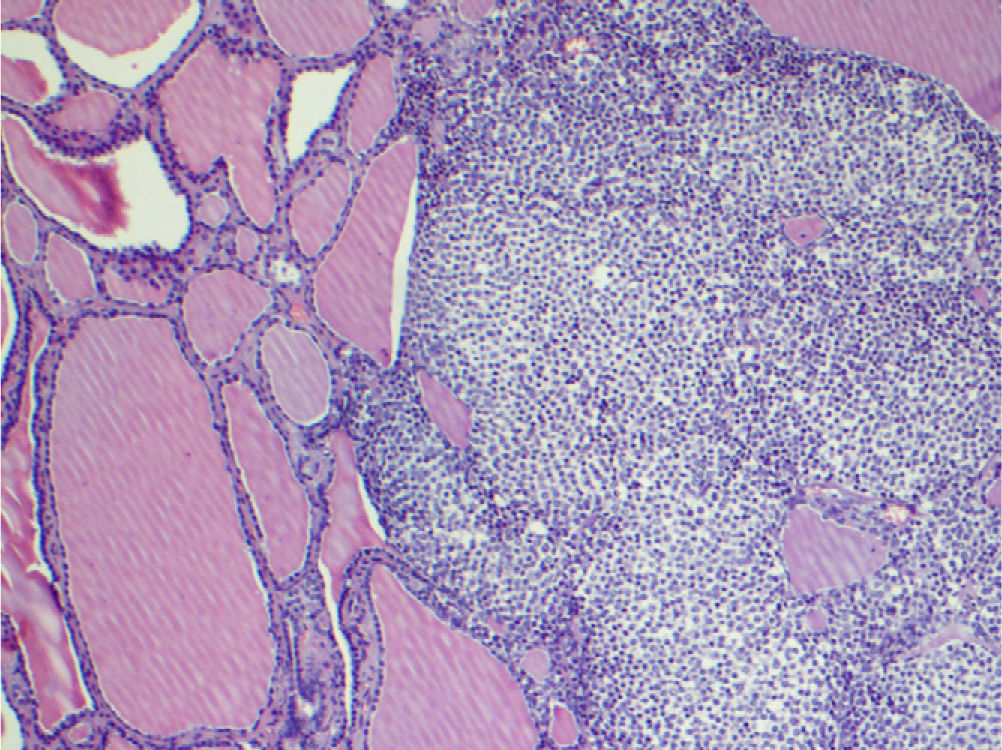
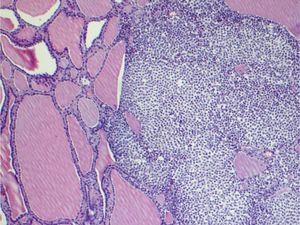
At the clinic, the patient showed stridor with advanced respiratory difficulty. In a neck examination, a goiter of hard consistency, immobile on swallowing, and with no cervical adenopathies was palpated. The patient reported having had goiter since a young age, but it had never been studied. Thyroid function was normal, with a TSH level of 0.82μIU/mL (0.27–4.2) and a free T4 level of 1.28ng/dL (0.93–1.71). Because of rapid goiter growth and symptomatic tracheal compression, urgent surgery was decided upon. During surgery, only left hemithyroidectomy plus istmectomy could be performed because the contralateral lobe was found adhered to adjacent structures with gross tracheal infiltration. Dyspnea subsided after surgery. Pathological analysis of the specimen revealed thyroid metastatic infiltration by a lobular breast carcinoma (Fig. 2).
Two week after thyroidectomy, the patient attended the emergency room for anuria over the previous 24h. A CT scan of the abdomen showed a big pelvic mass compressing both ureters with significant bilateral hydronephrosis. Nephrostomy was performed, and the patient was admitted to the oncology ward. In addition to pelvic mass, hepatic and bone metastases were found, with no evidence of local recurrence. The patient died one month after surgery.
Thyroid metastases are uncommon in standard clinical practice, but not in post mortem studies, in which they are found with a frequency ranging from 0.5% in unselected autopsies to 24% in patients with tumor history.1 In most autopsy series, the primary tumors most commonly causing thyroid metastases are breast and lung carcinomas. In clinical series, however, the most common cause is renal carcinoma.2 The rarer cases reported include metastases from a choriocarcinoma.3 In a series of 43 patients with metastatic thyroid involvement, 33% of primary tumors were renal, followed by tumors in the breast (16%), lung (16%), esophagus (9%), and skin (5%).4 In another study analyzing 18,105 thyroidectomies and 29,708 cytologies of samples taken by fine needle aspiration, the prevalence rates of metastatic tumors were 0.13% and 0.07% respectively.5 Prevalence increased to 1.4% in a series of 1013 patients with thyroid cancers, 14 of which were metastatic.6 In all these series, the most prevalent breast cancer was ductal infiltrating carcinoma, while a lobular infiltrating carcinoma was found in the case reported here.4
Most patients are diagnosed by fine needle aspiration, although the surgical specimen is sometimes required for final diagnosis.6 Differential diagnosis between an anaplastic thyroid carcinoma and a secondary tumor is often difficult. The presence of cervical adenopathies, advanced patient age, and neoplastic history may suggest a metastatic tumor, but a positive thyroglobulin test will provide definite diagnosis of an anaplastic carcinoma.7 In the case reported, the patient's age, the rapid growth of previously known goiter, and stone-hard consistency suggested anaplastic carcinoma rather than metastasis. Thyroid metastases are usually diagnosed in advanced disease stages and are associated with a life expectancy of only a few months.5 Although treatment is palliative in nature, thyroid surgery may improve symptoms and the quality of life in these patients.
In conclusion, when faced with a patient with a history of tumor and a thyroid nodule, a cytological evaluation should be performed on a sample taken by fine needle aspiration to rule out a potential metastatic origin.7
We thank Dr. Miguel Paja Fano for his great help in this and many other studies.
Please cite this article as: Egaña N, et al. Metástasis tiroidea de carcinoma lobulillar de mama. Endocrinol Nutr. 2012;59(3):215–24.