The management of patients with an incidentally detected pancreatic cyst is a significant clinical challenge. More than 80% are detected as incidental findings on CT scan or MRI. A case is presented of a 41-year-old patient with an asymptomatic pancreatic cyst which was detected during a check-up.
El tratamiento de los pacientes con un quiste pancreático incidentalmente detectado es un reto clínico considerable. Más del 80% son detectados como hallazgos incidentales durante la realización de una TAC o RM. Presentamos un caso de un paciente de 41 años con un quiste pancreático asintomático detectado durante una revisión.
Intraductal papillary mucinous neoplasia (IPMNs) was first described in 1982. Since then, its classification and management have evolved dramatically.1 The true prevalence of IPMNs is unknown. Most patients are asymptomatic at the time of diagnosis, and the cysts are usually discovered as an incidental finding on imaging.2 The use of computed tomography (CT) and magnetic resonance imaging (MRI) may partially explain the recent rise in prevalence of these lesions.3 The detection rate of pancreatic cysts by conventional MRI has been estimated to be as high as 13.5% in asymptomatic populations.4 IPMNs represent about 20–50% of all pancreatic cystic neoplasms and 38% of resected pancreatic cysts. The average age of diagnosis peaks at 60–70 years old, with a slightly higher prevalence in men and with recurrent acute pancreatitis without recognized biliary or alcoholic etiology as the most frequent expression.5 There are three varieties, the main duct tumor (MDT), the branch duct tumor (BDT), and mixed, having different incidences of malignancy and prognoses.6 The MDT has a frequency malignancy of 62% (36–100%) and BDT has a 2–3% of malignancy annual risk.7 At the time of diagnostics of IPMNs, approximately 10–20% of cases harbor invasive carcinoma, 10–20% in situ carcinoma, and the remaining 60–80% intraductal or intracystic adenoma with low degree dysplasia. There are some risk factors for malignancy in IPMNs such as size ≥3cm, a dilated main pancreatic duct, or the presence of an associated solid component, and if there present more than 2 risk factors, should be performed de EUS–FNA that has a sensitivity of approximately 60% and a specificity of 90% for the risk of malignancy in IPMNs.8 The molecular analyses of the cyst fluid for diagnosis are still evolving and there is not marker that distinguishes benign from malignant.7 Histologically, the gastric type is typically low grade, with normally small percentage developing into carcinoma, although if a carcinoma does develop in these patients, it is usually of the tubular type and behaves a conventional pancreatic ductal adenocarcinoma. In the published series, resectability in patients with IPMNs was 90–100%, while mortality and morbidity in patients with cancer related to IPMN were similar to those related to pancreatic surgery for ductal adenocarcinoma. Five-year survival is 100% for adenomas, 80–90% for in situ carcinomas, and 50–70% for invasive carcinomas.8–10 Therefore, an integral approach is important to make a correct diagnosis and initiate the proper management as soon as possible.
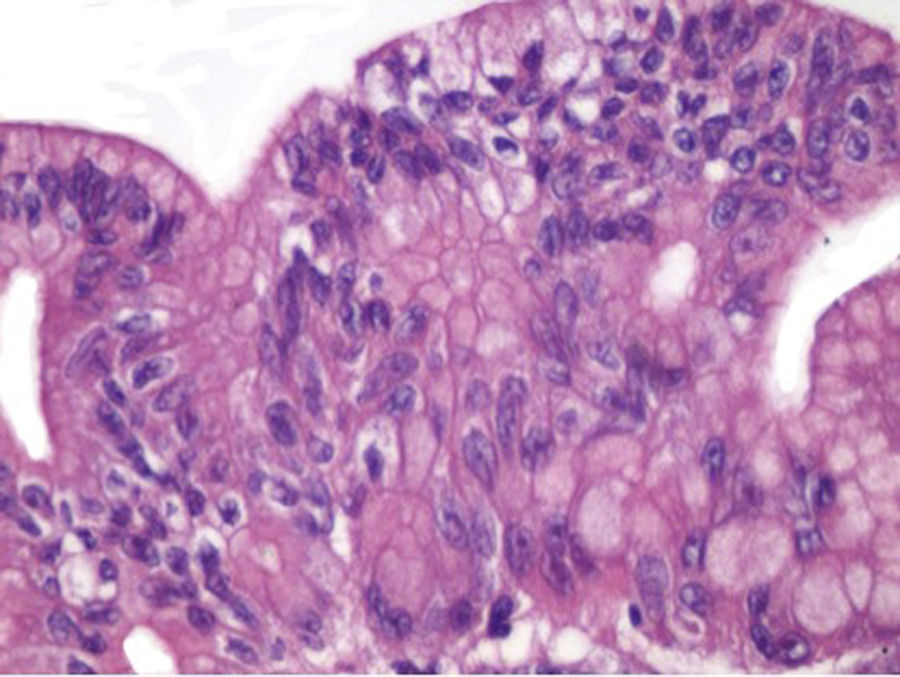
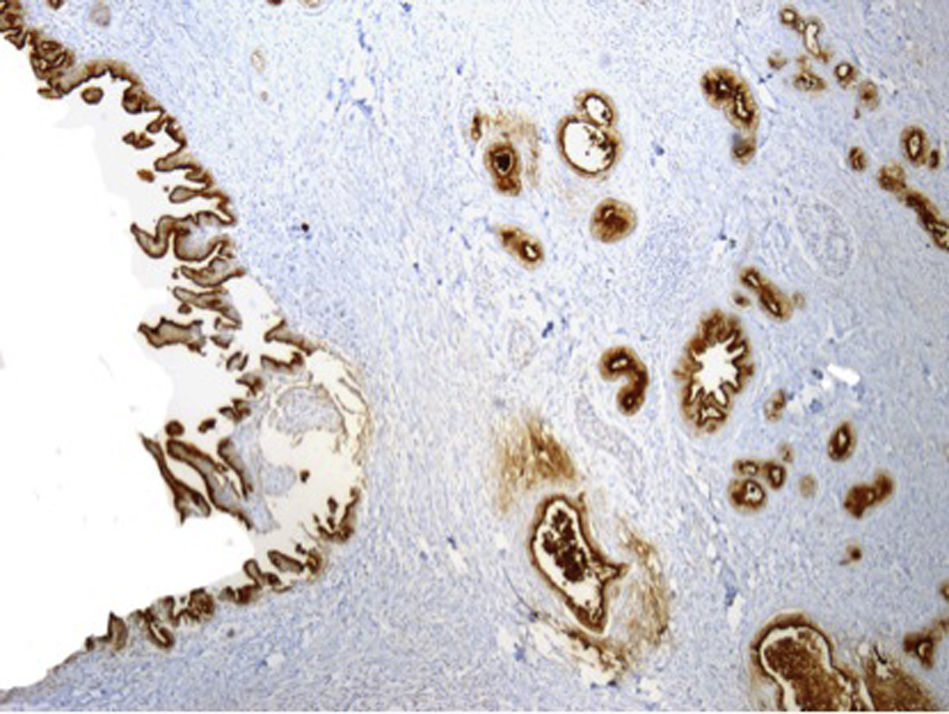
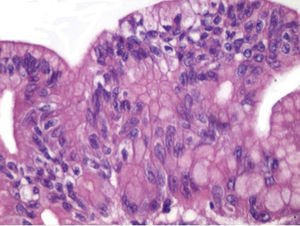
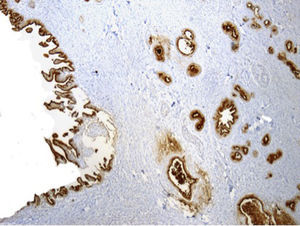
Case presentationIn November 2014, a 41-year-old female with an asymptomatic history was admitted for general check-up. She had relevant health record, and on physical examination the only thing that stood out was a BMI of 27kg/m2. During studies, non-contrast CT detected a hypodense cystic lesion located in the head and uncinate process of the pancreas that measured 20×11mm (Fig. 1). In January 2015, an endoscopic ultrasonography-guided fine-needle aspiration (EUS-FNA) was made, with a heterogeneous cystic tumor, with solid part, located in the head of the pancreas without vascular involvement, no communication with the pancreatic duct and main pancreatic duct in a maximum diameter of 3mm in the head. The lesion was suggestive of IPMNs of BDT (Fig. 2). The cytological abnormalities were compatible with BD-IPMN with moderate dysplasia, and no adenocarcinoma cytological data were identified. In August 2015, the patient underwent Whipple surgery with preserving pylorus. The histopathological findings were compatible with infiltrative ductal adenocarcinoma of intestinal type originating in BD-IPMN with dysplasia high and low degree with surgical margins tumor-free and no affection of main pancreatic ducto (Figs. 3 and 4), MUC2 and CK19 positive (Fig. 5). The post-surgical evolution was favorable with hospital discharge.
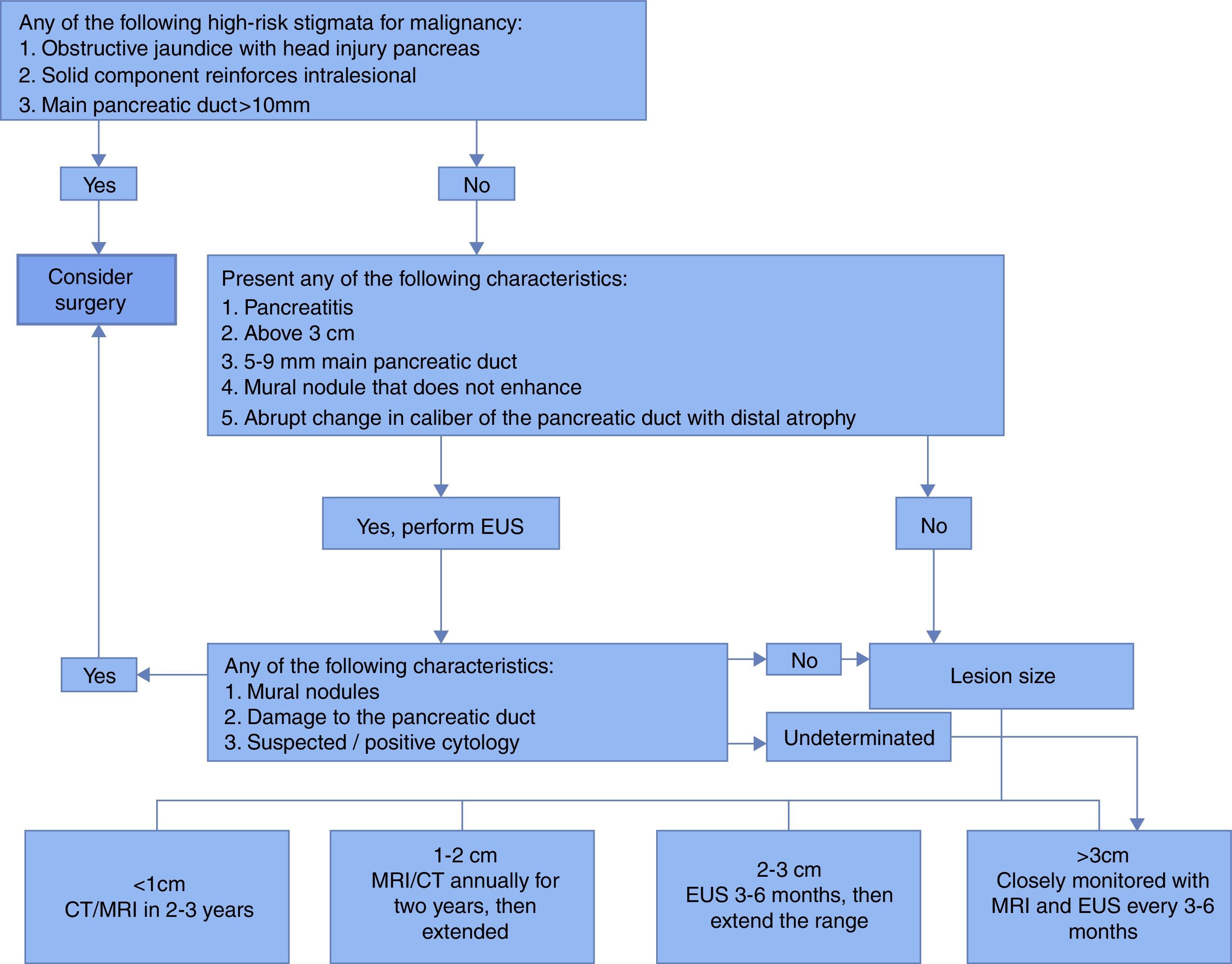
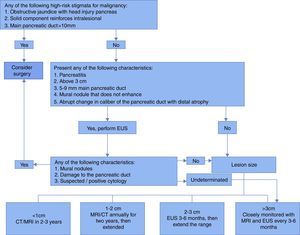
This year, the American Gastroenterological Association (AGA) presented its guidelines for the management of asymptomatic neoplastic pancreatic cysts and a decision support tool for clinicians. Most of the guidelines are conditional recommendations based on very low quality evidence. Based on retrospective cohorts, the prevalent risk of malignancy in cysts >3cm compared with those <3cm in size mildly increased, that increased the risk of malignancy approximately 3 times, as well as the risk of cancer in cysts associated with a dilated main pancreatic duct and solid component, the latter increased the risk of malignancy approximately 8 times.8 These recommendations are consistent with the Sendai guidelines (Fig. 6). In the case of our patient, the cyst was detected during a CT scan for a check-up. The hypodense pancreatic cystic lesion measured 20×11mm in CT, without any of the components of malignancy risk. The AGA recommends doing an MRI every two years after a one-year follow-up for cysts without >2 high-risk features, then stopping surveillance entirely for cysts that have no concerning features and seem stable by MRI imaging for >five years, regardless of size. We have to reconsider to base our decisions on a particular patient guided only by the size of the lesion. Our patient is an example of a natural history of IPMN and risk of malignancy.
Ethical responsibilitiesProtecting people and animalsThe authors declare that this research has not been conducted experiments on humans or animals.
Data privacyThe authors declare that this article does not appear patient data.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
FundingThe authors did not receive sponsorship to undertake this article.
Conflict of interestsThe authors declare no conflict of interest.