A 20-year-old-man presented with a mass over manubrium sterni for 4 months. He is from Ethiopia and came to Turkey 6 months ago. The patient also complained of fatigue and back pain. He had fever and weight loss (8kg), but no cough, and sputum. The patient denied an underlying disease and trauma. The previous medical history was also unremarkable for medications. On examination, the patient looked fatigue and fully cooperative. The mass was about 11cm×9cm in size and fluctuating but had no pain and no redness (Fig. 1). The laboratory values showed a total white blood cells count of 9300cells/mcL, with 70% neutrophils, C-reactive protein: 90mg/dL (0–5), sedimentation rate: 105mm/h. He had anemia of chronic disease and hemoglobin level was 10g/dL. Ultrasound revealed a fluid collection with intense content, indicating an abscess formation. Fine needle aspiration puncture was administered for diagnosis. Some fluids were aspirated for culture and ampicillin–sulbactam 1/0.5g every 6h was empirically administered for pyogenic sternal infection. Despite the administration of the antibiotic for 10 days, the swelling did not regress, on the contrary, continued to increase in size. The gram staining of the samples revealed abundant leukocytes but no microorganisms. The solid and liquid cultures of the materials were all sterile. Also, it was negative for acid-fast bacteria. Urinalysis, basic chemistry, and hepatic function testing were within normal limits. Serologies for syphilis, Brucellosis, Hepatitis B Virus, Human Immunodeficiency Virus, Epstein–Barr Virus, Toxoplasmosis, and Cytomegalovirus were unremarkable.
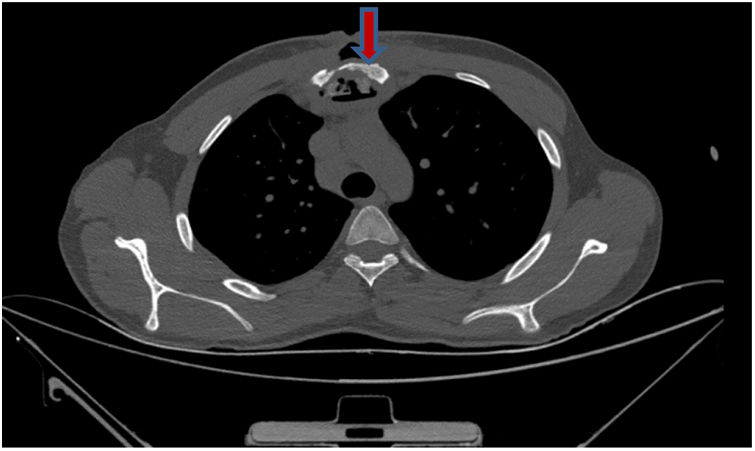
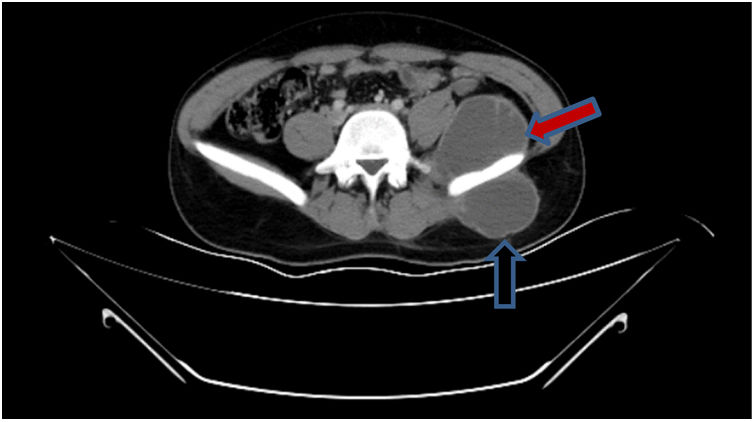
Diagnosis and evolutionIn detailed medical history, there was a positive history of tuberculosis (TB) in his family. Hemocultures were sterile. Computed tomography revealed a mass causing significant bone destruction on manubrium sterni and extending to the anterior mediastinum (Fig. 2). In addition, vertebral osteomyelitis was observed, showing enhancement of L1, T12, T11, T10, T9, and T8. Abdominal scan demonstrated a psoas abscess measuring approximately 66mm×45mm and a gluteal abscess measuring 40mm×56mm (Fig. 3). Due to the lack of improvement, the sternal mass was surgically removed. The routine bacterial cultures were repeated but remained sterile. A tuberculin skin test was positive (induration=20mm). Tuberculosis culture was not available and therefore could not be performed. Polymerase chain reaction (PCR) of the excised tissue was positive for TB. The biopsy disclosed necrotizing granulomatous inflammation which was consistent with TB. A diagnosis of TB was made and quadruple anti-TB drugs including isoniazid, rifampin, pyrazinamide, and ethambutol were initiated. The abdominal abscess was drained completely. A material also tested positive for TB via PCR. The drugs were administered for 9 months. The patient has been doing well for 3 months and no recurrence.
Osteomyelitis of the sternum is a rare condition that can lead to multiple diagnostic differentials in adults. Generally, it results from a complication of sternotomy, trauma and mediastinitis.1 Commonly, the causative agent is Staphylococcus aureus. Therefore, antibiotics covering this microorganism are administered empirically.
TB is primarily infection of the lungs and rarely bone involvements can be observed. Skeletal tuberculosis refers to TB involvement of the bones and/or joints. It accounts for 10–35 percent of cases of extrapulmonary TB.2,3 Mycobacterial infection of the sternum is an extremely rare condition and constitutes less than 1% of TB osteomyelitis.4,5 Generally, it results from either an extension from hilar lymph nodes or hematogenous/lymphatic dissemination of TB from other infectious focus.4 Sternal TB manifests as an insidious swelling and pain. Generally, a single mass occurs on anterior chest wall. Aspiration and anti-TB chemotherapy are treatment options in sternal TB. Surgery is recommended if a large sequestrum needs to be removed.
In conclusion, TB is an infectious disease which can manifest in a variety of clinical entity. As in our case, TB should be included in the differential diagnosis of a patient presenting with a sternal mass, especially in endemic regions.
Conflict of interestThere is no conflict of interest.