A 61-year-old male with type II, insulin-dependent diabetes mellitus with poor control, came in for progressive low-back pain and persistent fever associated with dysuria. For the past 3 days, he had been taking oral amoxicillin plus clavulanic acid due to a suspected urinary tract infection. During the physical examination, there was notable pain in the right renal fossa with positive kidney punch. The basic analysis showed leukocytosis of 18,300×10e9/l with neutrophilia of 92.3%, elevated lactate (2.7mmol/l), procalcitonin (11.57ng/ml) and fibrinogen (703mg/dl). Urine sediment showed no bacteriuria or leukocyturia. An emergency abdominal ultrasound was performed with no pathologically significant findings.
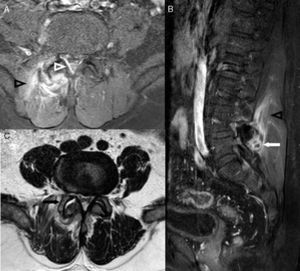
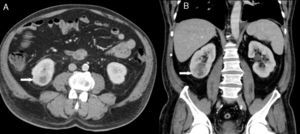
Clinical courseThe patient was admitted with a diagnosis of sepsis, of probable urinary focus. Treatment with amoxicillin/clavulanic acid was switched to ceftriaxone plus amikacin. In the haemocultures done at admission, Escherichia coli grew with the following susceptibility pattern: sensitive to cefuroxime, ciprofloxacin, gentamicin and co-trimoxazole, intermediate sensitivity to amoxicillin/clavulanic acid and resistant to ampicillin. The uroculture was negative. In light of these results, the same treatment was continued. On the fourth day of admission, backache and fever persisted, with additional pain irradiating to the right lower limb. For this reason, an MRI of the lumbar spine was requested due to suspicion of spondylodiscitis. Findings compatible with facet joint septic arthritis with adjacent focal meningitis were observed (Fig. 1). A CT-guided puncture aspiration of the right L4–L5 facet joint was performed, collecting joint fluid, the culture of which was also positive for E. coli. In order to detect possible intra-abdominal foci that would explain the presence of these bacteria in the facet joint, an abdominal CT was performed, observing focal pyelonephritis in the right kidney (Fig. 2). The patient was discharged after 10 days of intravenous antibiotic treatment, showing good response thereto, receiving oral antibiotic therapy with cefuroxime plus ciprofloxacin for 30 days.
MRI of the lumbar spine consistent with facet joint septic arthritis of right L4–L5. Axial (A) and sagittal (B) T1-weighted fat-suppressed image with intravenous contrast. Axial T2-weighted image (C). Joint effusion (black arrow) and a small collection (white arrow) located behind the facet joint is observed. The adjacent paraspinal musculature shows inflammatory changes (black arrowheads). In the posterior and lateral right epidural space, a thickening and contrast enhancement is observed (white arrowhead), due to adjacent focal meningitis.
Abdominal CT scan showing findings consistent with right focal pyelonephritis. Axial (A) and coronal (B) image with intravenous contrast in nephrographic phase. A focal hypodensity with poorly defined borders (white arrows) is observed in the lower end of the kidney, affecting the cortex and medulla.
Facet joint septic arthritis is a rare entity.1–3 Said condition forms part of the differential diagnosis of back pain and is probably being under-diagnosed.
The main agent implicated in this condition is Staphylococcus aureus; however, there have been cases published that implicate other micro-organisms, although less frequently.1,4 Micro-organisms reach the joint haematogenously (occasionally due to vascular catheter infection), but has also been reported due to direct inoculation via diagnostic or therapeutic punctures, or due to proximity.5
The diagnosis of facet joint septic arthritis is a clinical, microbiological, and radiological challenge. On the one hand, it is a rare condition, with poorly orienting symptoms, and, on the other hand, the definitive microbiological diagnostic method involves invasive techniques to obtain joint fluid. Its clinical presentation is very similar to spondylitis or spondylodiscitis, with it being important to distinguish between them given the differences in treatment and prognosis. Spondylodiscitis, due to the pain and risk of instability, requires greater immobilisation and subsequent physical therapy, tending to have more complications, mainly epidural abscesses, spinal cord compression and spinal column deformities.6,7 In this context, the imaging techniques play a key role in reaching the definitive diagnosis. These include MRI, due to its greater sensitivity and specificity, that make it the main diagnostic method for this entity.8
Treatment for this condition mainly requires use of systemic antibiotics, although in some cases severe neurological impairment can arise requiring percutaneous and/or surgical drainage.9 Although this entity does not usually have a fatal outcome, it may leave permanent functional sequelae or be accompanied by systemic complications secondary to sepsis.10
Please cite this article as: León Salinas JP, Albertz Arévalo N, Belloch Ramos E, Guerrero Espejo A. Una causa inusual de dolor lumbar en paciente con sepsis. Enferm Infecc Microbiol Clin. 2017;35:536–538.