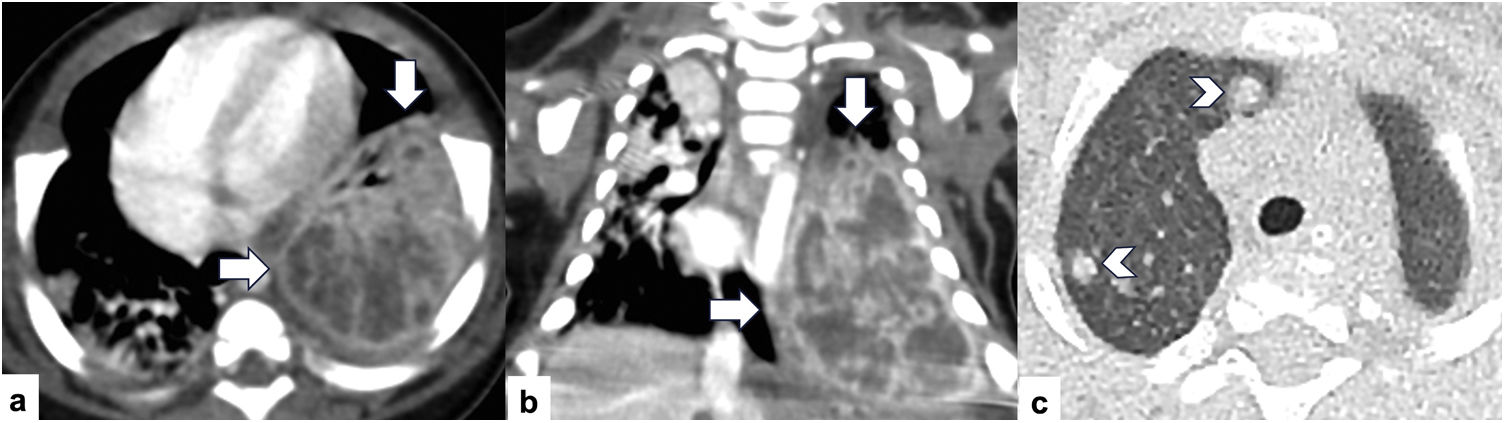
A 5-month girl presented with fever and respiratory symptoms. She had past medical history of multiple episodes of skin and gluteus abscesses treated with oral antibiotics. Physical exam revealed multiple subcutaneous nodules in the chest and enlarged lymph nodes in axillary regions. Chest CT was performed and showed a left lower lobe consolidation with cavitations suspicious of lung abscess and multiple pulmonary nodules in bilateral lungs (Fig. 1). Laboratory work up was negative for HIV, mycobacteria, and TB. Concomitant, clinical investigation revealed severe combined immunodeficiency with phenotypical features suggestive of cartilage hair hypoplasia. Lymph node biopsy showed fibroblasts and multiple aerobic filamentous bacilli with surrounding granulation tissue.
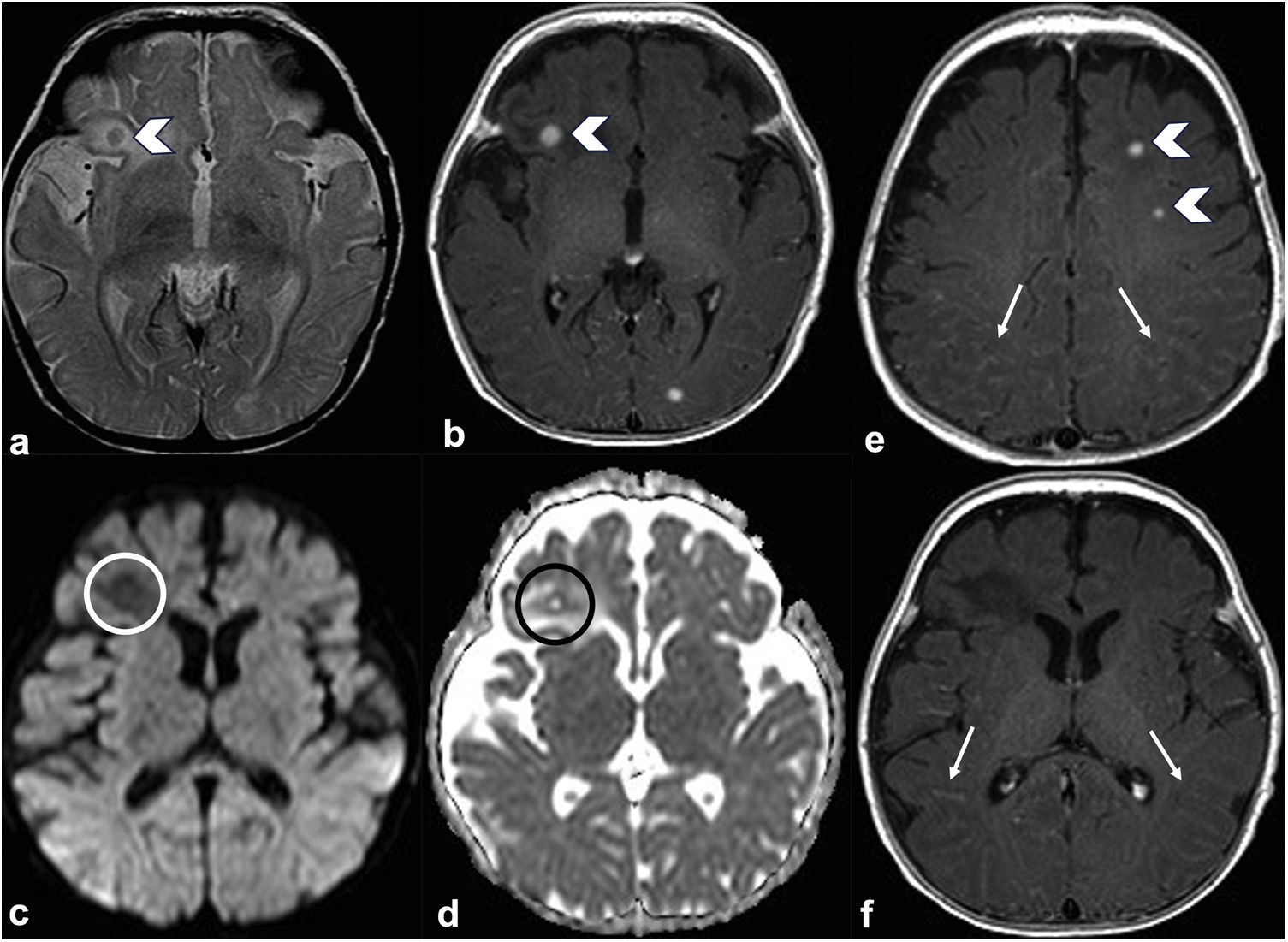
Evolution and diagnosisBrain MRI demonstrated multiple enhancing nodules in bilateral cerebellar hemispheres with low signal on T2 weighted images and surrounding vasogenic edema. There was neither restricted diffusion nor blooming artifact on susceptibility weighted images (SWI). Leptomeningeal enhancement was seen on bilateral parietal and occipital regions (Fig. 2). The imaging findings were suggestive of multiple granulomas and meningitis.
Axial T2 (a) and T1 with contrast (b) weighted images of brain MRI show a right frontal enhancing nodule with associated vasogenic edema (arrowheads). Axial DWI and ADC map (c and d) demonstrate no restricted diffusion of the right frontal lesion (circles). Axial T1 with contrast weighted images (e and f) show two enhancing nodules in the left frontal lobe (arrowheads) and abnormal leptomeningeal enhancement in bilateral parietal and occipital regions (arrows).
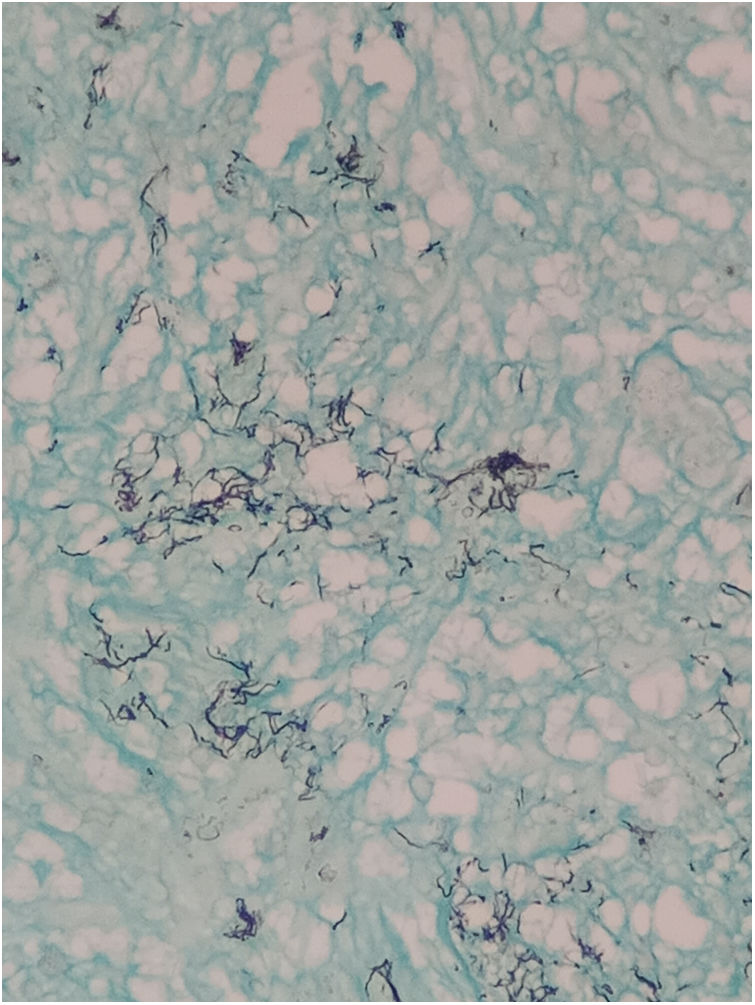
The patient underwent a left frontal craniotomy for resection of one the lesions and confirm the etiology, the sample was sent for bacterial and fungal culture. Bacterial culture showed aerobic filamentous bacilli consistent with Nocardia (Fig. 3). The patient was hospitalized for approximately 3 months and treated with intravenous antibiotics trimethoprim/sulfamethoxazole (TMP/SMX)) with improvement of the symptoms. She was discharged home on treatment doses of TMP/SMX.
Nocardiosis is an uncommon central nervous system (CNS) infection with a mortality rate of about 34% and more frequent in immunocompromised patients.1 It is caused by a branching filamentous bacteria that is weakly acid fast positive, mostly isolated from plants and soil, which usually infects humans as result of inhalation or direct skin inoculation.1 It often spreads from the lungs to other sites, usually skin and brain. CNS infection is commonly found as a secondary lesion due to hematogenous spread with less than 10% of the cases reported to originate in the CNS.1 It often presents as brain abscess and corresponds to 2% of all brain abscesses.1
The development of granulomas is commonly found in chronic infections such as those produced by mycobacterias as tuberculosis and leprosy. Regarding nocardiosis, it has been described that mycolic acid containing glycolipids induce granulomatous changes like mycobacteria. These glycolipids persist in the macrophages for a long time because they are resistant to digestion by lysosomal enzymes. Moreover, these glycolipids act on macrophages through lysosomal or plasma membranes to release chemotactic factors and colony factors which participate in granuloma formation.2
In pediatric population Nocardia CNS infection is rare with high mortality rate of approximately 40%.3 Symptoms are non-specific, focal deficit can be seen in 40% of the cases and seizures can be present in 30% of the patients.3 Given it is a very rare infection in children, immunocompromising diseases must be rule out, including chronic granulomatous disease, transplants, malignancy, chronic steroid, or genetic disorders3 as our patient who had severe combined immunodeficiency with phenotypical features suggestive of cartilage hair hypoplasia. Moreover, in immunocompromised patients with pulmonary nocardiosis is recommended to perform screening of CNS infection with intracranial imaging. Standard medical treatment is trimethoprim/sulfamethoxazole for a period of 6 months through intravenous route followed by oral administration for a long period up to 1 year in immunocompromised patients.3
Although Nocardia CNS infection is rare, it should be included in the differential diagnosis of patients with brain abscess, meningitis and/or granulomas and further work up must be guaranteed to rule out immunodeficiency. In addition, in patients with high clinical suspicion, such as those with pulmonary or skin infection, concomitant CNS compromised should be excluded.
Authors’ contributionsAll authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Jose Rincón-Sarmiento, Angela Guarnizo, Gabriela Lamas and Carlos Rugilo. The first draft of the manuscript was written by Angela Guarnizo and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethics approvalEthical approval was waived by the local Ethics Committee of “Hospital de Pediatría Prof. Dr. Juan P. Garrahan” in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Informed consentThe article does not contain photographs or indication that could be traced back to a human participant. The patient's mother gave a written informed consent for all testing during the clinical process.
FundingThe authors have no relevant financial or non-financial interests to disclose.