The COVID-19 pandemic has been generating a serious public health crisis in Peru, which has recently recorded a mortality of approximately 9.4%, with 2,043,262 confirmed cases and 191,447 deaths.1 These data reflect the precarious health situation of the country due to the limited number of hospitals, the shortage of essential materials for health care, the poor implementation of specialised laboratories and the reduced availability of hospital beds, mechanical ventilators and specialised health personnel.2 Added to this is the health burden of infectious and chronic diseases such as tuberculosis (TB) and other respiratory infections that represent 86.2% and 86.6%, respectively, in years of life lost due to premature death.3
TB and COVID-19 are currently the two leading causes of death in the world among infectious diseases, and TB/COVID-19 coinfection favours the progression and worsening of both diseases because both diseases tend to induce an unbalanced inflammatory response, which doubles the risk of mortality in affected patients (RR=2.10; 95% CI, 1.75–2.51; p<0.00001).4,5
Prior to the pandemic, in 2018, 235,345 incident cases of TB were reported in America, and Peru was classified as one of the countries with the highest incidence (98.2 cases/100,000 inhabitants), ranking second after Brazil, with a high burden of people infected throughout the continent.6 Metropolitan Lima and Callao report 64% of the TB cases, 79% are multidrug resistant (MDR-TB) and 70% are extremely resistant (XDR-TB).7
In 2020, the global TB programme of the World Health Organization (WHO) showed a 25–30% drop in notifications of cases of people infected by several countries with a high disease burden, such as India, Indonesia and the Philippines. Likewise, in the Americas, the diagnosis of new TB cases fell between 15% and 20% during 2020, due to the pandemic.8 This would negatively impact TB mortality, since WHO models indicate that, if 50% of those infected are not identified for a period of three months, it would lead to around 400,000 more people succumbing to this disease.9
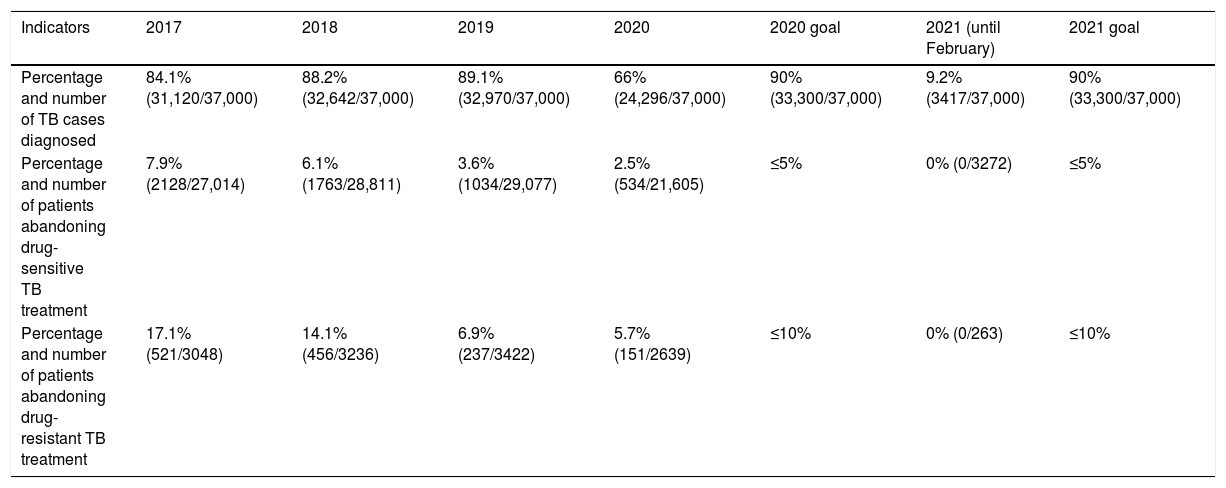
At the beginning of the pandemic, the offer of services at the first level of care was limited to emergencies, with health promotion and risk prevention being restricted, as well as outpatient consultations to monitor patients with chronic diseases.10 This may have led to the underdiagnosis of TB cases in 2020 (Table 1). It can be expected that the number of MDR-TB cases will increase in 2021–2022 and further affect treatment outcomes.11
Advances and gaps in TB overage in Peru from 2017 to February 2021.
| Indicators | 2017 | 2018 | 2019 | 2020 | 2020 goal | 2021 (until February) | 2021 goal |
|---|---|---|---|---|---|---|---|
| Percentage and number of TB cases diagnosed | 84.1% (31,120/37,000) | 88.2% (32,642/37,000) | 89.1% (32,970/37,000) | 66% (24,296/37,000) | 90% (33,300/37,000) | 9.2% (3417/37,000) | 90% (33,300/37,000) |
| Percentage and number of patients abandoning drug-sensitive TB treatment | 7.9% (2128/27,014) | 6.1% (1763/28,811) | 3.6% (1034/29,077) | 2.5% (534/21,605) | ≤5% | 0% (0/3272) | ≤5% |
| Percentage and number of patients abandoning drug-resistant TB treatment | 17.1% (521/3048) | 14.1% (456/3236) | 6.9% (237/3422) | 5.7% (151/2639) | ≤10% | 0% (0/263) | ≤10% |
Source: Dirección de Prevención y Control de la Tuberculosis (DPCTB) [Tuberculosis Prevention and Control Directorate], Ministry of Health, Peru.
The pandemic has caused us to lose interest in communicable and chronic diseases such as TB, which, associated with socioeconomic factors and a health system hit by the pandemic, could lead to it becoming a greater public health problem than it currently represents. In order to reduce the need for visits to health facilities, the monitoring of the therapeutic regimen of these patients should be guaranteed with the timely and uninterrupted delivery of their medication implemented with epidemiological surveillance based on digital technologies. Likewise, in order to mitigate underdiagnosis, a telemedicine system based on health promotion and community monitoring could be implemented, allowing the necessary services to be brought as close as possible to the people and communities affected by TB.
In the case of patients who cannot access these digital technologies or face-to-face assessment in health centres, TB units could be set up to ensure all the necessary health measures to increase confidence among the population and reduce the risk of resistant forms of TB. These among other measures would be able to boost early diagnosis, access to medications and control of adherence to treatment, while avoiding the spread of COVID-19.
FundingSelf-financed.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Cardenas-Escalante J, Fernandez-Saucedo J, Cubas WS. Impacto de la pandemia por COVID-19 en la tuberculosis en el Perú: ¿nos estamos olvidando de alguien? Enferm Infecc Microbiol Clin. 2022;40:46–47.