In Spain, like in other countries where endemic measles has been eliminated, there is a need for available diagnostic tolos for confirming any cases in order to prevent and control its transmission. We describe the different microbiological tests used for the diagnosis of measles during an outbreak that occurred in 2019 in the province of Guadalajara (Spain).
MethodsSerological and molecular tests were performed at the Microbiology laboratory of the Guadalajara University Hospital and at the National Center for Microbiology of the Carlos III Health Institute (Majadahonda, Spain). Patient data were obtained from the surveillance system.
ResultsA total of 43 patients had a laboratory diagnosis of measles: 29 cases by PCR (pharyngeal exudate or urine) and positive specific IgM, 11 cases by PCR, and 3 cases only by a positive IgM. Genotype D8 was identified in 35 confirmed cases and genotype A in two that were discarded as post-vaccination cases. PCR was positive in the acute sera of 11 out of 14 patients with a negative IgM. Eleven confirmed cases had recieved one or two vaccine doses. Twelve adult patients were hospitalizated, all of them with a diagnostic of hepatitis.
ConclusionsThe combination of molecular tests and the presence of specific IgM is necessary for a correct diagnosis of measles and also to classify patients with a breakthrough infection or vaccine failures (primary or secondary). Genotyping is essential for the correct classification of the patients in the context of a measles elimination program.
En España, al igual que en otros países donde el sarampión endémico ha sido eliminado, es necesario utilizar de forma rutinaria las herramientas diagnósticas que confirmen los casos para su prevención y control de la diseminación. Se describen los diferentes ensayos microbiológicos utilizados para su diagnóstico durante un brote de sarampión en 2019 en la provincia de Guadalajara (España).
MétodosLas pruebas serológicas y moleculares se realizaron en el laboratorio de Microbiología del Hospital Universitario de Guadalajara y en el Centro Nacional de Microbiología del Instituto de Salud Carlos III (Majadahonda, España). Los datos de los pacientes se obtuvieron del sistema epidemiológico de vigilancia.
ResultadosSe diagnosticaron de sarampión un total de 43 pacientes por métodos microbiológicos: 29 casos por PCR (exudado faríngeo u orina) junto con IgM específica positiva, 11 pacientes solamente por PCR, y 3 pacientes exclusivamente por presencia de IgM. El genotipo D8 fue identificado en 35 pacientes y el genotipo A en dos casos descartados como post-vacunales. La PCR en suero fue positiva en 11 de 14 pacientes con ausencia de IgM en su primera muestra recogida de suero. Once casos confirmados habían recibido una o dos dosis de vacuna. Doce adultos fueron ingresados, todos diagnosticados de hepatitis.
ConclusionesLa combinación de pruebas moleculares y la presencia de IgM específica es necesaria para un diagnóstico correcto y la clasificación de los pacientes como fallo vacunal (primario o secundario). El genotipado es una herramienta fundamental para la correcta clasificación de los pacientes en el contexto de un programa de eliminación del sarampión.
Measles is a highly contagious respiratory disease that only affects humans. The existence of a highly effective specific vaccine has resulted in a significant decrease in the incidence of the disease. This has led the World Health Organization (WHO)1 to set the goal of eliminating this disease. In 2017, the WHO declared that Spain had achieved measles elimination by not having registered endemic transmission in the prior three years, in the presence of a sensitive and specific surveillance system. Thus, the cases of measles that occur in Spain are imported or related to importation, and the outbreaks are small and limited in time, mainly affecting unvaccinated adults or those with incomplete vaccination.2 Cases in fully vaccinated people in Spain were estimated at 3% until 2014.3 However, they have been increasing in recent years, as described in other countries in a situation of elimination and high vaccination coverage. For proper control and prevention of secondary cases and identification of chains of transmission, laboratory investigation of cases is necessary in the shortest time possible, including molecular characterisation of the strains. Classically, the diagnosis was based on the detection of specific antibodies of the IgM class against the virus. The delay in the detection of specific acute phase antibodies (IgM) or in the seroconversion of the IgG antibody titre has favoured the increasingly widespread use of the detection of viral genomes for diagnosis due to their earlier positivity.
In addition, the existence of measles cases in fully vaccinated people poses great diagnostic challenges both from a clinical point of view, since they may present with an atypical form of the disease, and from a laboratory diagnosis point of view, since specific IgM is not detected or appears later. This diminishes the negative predictive value of this technique, making molecular diagnosis more relevant for the correct classification of cases. Moreover, in countries with low circulation of the virus, specific IgM in a case without a clear epidemiological link or strong clinical suspicion does not allow the case to be confirmed. In this way, the WHO has established specific diagnostic algorithms for countries in a situation of measles elimination.1
In 2019, 606 suspected cases of measles were reported in Spain. The national incidence rate was 0.61 cases/100,000 inhabitants. Most of the cases were registered in the autonomous communities of Catalonia, Madrid, the Community of Valencia and Castilla-La Mancha. The highest rate by autonomous community was registered in Castilla-La Mancha, with 2.85 cases/100,000 inhabitants.2
This work describes the epidemiological, microbiological and clinical characteristics of the cases diagnosed in the province of Guadalajara (Spain) pertaining to an outbreak that also affected the autonomous communities of Madrid and Aragon, and the difficulties in diagnosing the cases.
MethodsThe study was conducted with the samples received between 8 April and 25 August 2019 at the Hospital Universitario de Guadalajara [University Hospital of Guadalajara], which serves a population of approximately 250,000 inhabitants. The samples came from patients who attended the hospital's Emergency Department or from different primary care centres throughout the province. The clinical-epidemiological data from all the patients were collected from the information provided by the Epidemiology Department of the Delegación de Sanidad y Asuntos Sociales de Guadalajara [Delegation for Health and Social Affairs of Guadalajara]. These data included: age, sex, symptom onset date, exanthem onset date, clinical signs and symptoms, known contacts, travel history, previous vaccination, complications, and requirement for hospitalisation.
Case definitionThe cases were classified following the criteria described in the surveillance protocol from the Red Nacional de Vigilancia Epidemiológica [National Epidemiological Surveillance Network]4:
Suspected case (clinically compatible case): person who meets the clinical criteria from whom it has not been possible to collect samples for serological confirmation and who has not been in contact with a laboratory-confirmed case.
Probable case (case confirmed by epidemiological link): person who meets clinical criteria and who has an epidemiological link to a laboratory-confirmed case.
Confirmed case (laboratory confirmed case): person not recently vaccinated who meets clinical and laboratory criteria (presence of specific IgM in serum or detection of virus RNA in throat swab and/or urine sample). A recently vaccinated person in whom the wild-type genotype of the virus is detected.
Case ruled out: a case that meets the clinical criteria for measles and has negative laboratory results, or that is epidemiologically linked to a laboratory-confirmed case of another exanthem-producing illness.
Microbiology studyDetection of specific IgG/IgM was carried out in serum samples by chemiluminescent immunoassay (LIAISON® Measles IgG/IgM, DiaSorin) in LIAISON® Analyser ® (DiaSorin, Saluggia, Italia).
Nucleic acid extraction was carried out with the MagCore® automatic extractor (RBC Bioscience, New Taipei City, Taipei) in the microbiology laboratory of the Hospital Universitario de Guadalajara. Measles virus genome amplification was performed by real-time PCR, specific for the nucleoprotein gene (RealCycler®, Progenie Molecular).
For the confirmation of the first 17 cases and the genotyping of the viruses, the samples were sent to the Centro Nacional de Microbiología del Instituto de Salud Carlos III [Charles III Health Institute National Microbiology Centre] (Majadahonda, Spain). Total nucleic acid extraction was carried out using the commercial QIAsymphony® Virus/Bacteria Midi Kit (96) (Qiagen) using an automatic extractor (QIAsymphony, Qiagen, Hilden Germany). The measles genome was detected using a multiplex real-time PCR for exanthematic viruses (rubella, measles, and parvovirus B19), included in the Programa de Vigilancia Microbiológica de sarampión y rubéola [Measles and Rubella Microbiological Surveillance Programme].5 Furthermore, the determination of the genotype and the analysis of variants was carried out by 450 nucleotide fragment sequencing of the nucleoprotein gene (N450), recommended by the WHO, after its amplification by means of a previously described real-time PCR.6 The determination of IgM and IgG at the Centro Nacional de Microbiología was carried out by ELISA (Enzygnost® Anti-Measles Virus [IgM/IgG], Siemens).
ResultsDuring the period between 8 April and 25 August, 2019, 88 suspected cases of measles were reported in the province of Guadalajara (Spain). Of these, 48 were classified as confirmed because they met the clinical and laboratory criteria for measles. 43 were diagnosed at the Hospital Universitario de Guadalajara, and the other five in the autonomous communities of Madrid or Aragon. Eight cases were classified as suspected and three as probable. 29 cases were ruled out. Among these were two cases when verifying by genotyping (genotype A, vaccine strain), which involved postvaccinal exanthems, and another case with positive IgG and IgM due to not presenting with clinical symptoms, and due to two oropharyngeal samples and one urine sample being negative by PCR. In other cases that were ruled out, another aetiological agent was detected, parvovirus B19 in three cases and rubella virus in one case.
Serum samples were received from the cases (between zero and two per patient), 41 throat swabs and 15 urine samples.
The microbiological diagnoses of the 43 cases were made in 29 cases due to the presence of specific IgM and positive PCR (65.9%); in 11 cases due to positive PCR and in three cases due to the presence of IgM (Table 1). In five of the cases diagnosed by PCR and IgM, this was detected in a second serum sample.
Microbiological diagnostic method of the 43 cases of measles and its temporal relationship with the appearance of the exanthem.
| Days in relation to the appearance of the exanthem | ||||||
|---|---|---|---|---|---|---|
| Case | IgM | IgG | PCR (throat/urine) | −2 to 0 | 1 to 4 | >4 |
| 1 | Pos | Neg | Pos | x | ||
| Pos | Neg | x | ||||
| 2 | Neg | Neg | ND | x | ||
| Pos | Pos | Pos | x | |||
| 3 | Pos | Neg | Pos | x | ||
| 4 | Pos | Neg | Pos | x | ||
| 5 | Weak pos | Neg | Pos | x | ||
| Pos | Pos | x | ||||
| 6 | Neg | Pos | Pos | x | ||
| 7 | Pos | Neg | Pos | x | ||
| 8 | Weak pos | Neg | Pos | x | ||
| 9 | Weak pos | Pos | Pos | x | ||
| 10 | Neg | Pos | Pos | x | ||
| 11 | Weak pos | Neg | Pos | x | ||
| 12 | Pos | Neg | Pos | x | ||
| Pos | Pos | x | ||||
| 13 | Neg | Pos | Pos | x | ||
| 14 | Pos | Pos | Pos | x | ||
| 15 | Pos | Pos | Pos | x | ||
| 16 | Pos | Neg | Pos | x | ||
| 17 | Pos | Pos | Pos | x | ||
| 18 | Neg | Neg | Pos | x | ||
| 19 | Neg | Neg | Pos | x | ||
| Pos | Pos | x | ||||
| 20 | Neg | Neg | Pos | x | ||
| 21 | Neg | Neg | Pos | x | ||
| 22 | ND | ND | Pos | x | ||
| 23 | Pos | Neg | Pos | x | ||
| 24 | ND | ND | Pos | x | ||
| 25 | Pos | Neg | Pos | x | ||
| 26 | Pos | Pos | Pos | x | ||
| 27 | Pos | Pos | Pos | x | ||
| 28 | Pos | Pos | Pos | x | ||
| 29 | Pos | Neg | Pos | x | ||
| 30 | Neg | Neg | x | |||
| Pos | Neg | Pos | x | |||
| 31 | Neg | Pos | Pos | x | ||
| Neg | Pos | x | ||||
| 32 | Neg | Neg | Pos | x | ||
| Pos | Pos | x | ||||
| 33 | Pos | Neg | ND | x | ||
| 34 | Neg | Neg | Pos | x | ||
| Pos | Pos | x | ||||
| 35 | Pos | Neg | Pos | x | ||
| 36 | Pos | Pos | ND | x | ||
| 37 | Weak pos | Neg | Pos | x | ||
| 38 | Neg | Pos | Pos | x | ||
| 39 | Pos | Neg | Pos | x | ||
| 40 | Pos | Neg | Pos | x | ||
| 41 | Neg | Pos | ND | x | ||
| Pos | Pos | x | ||||
| 42 | Pos | Neg | Pos | x | ||
| 43 | ND | ND | Pos | x | ||
ND, not done; Neg, negative; PCR, polymerase chain reaction; Pos, positive; Weak pos, weak positive (1–1.4 index).
Of the 11 cases diagnosed exclusively by PCR, serum was only available in eight, in which the sample was taken early, within four days following the appearance of the exanthem (baseline serum for seroconversion study).
In the three cases in which the microbiological diagnosis was made exclusively by the presence of IgM, no sample was available for PCR.
Specific IgG antibodies were present in the first serum sample from 14 patients. In six patients, IgG seroconversion was evidenced with a second serum sample.
The genotype was determined in 37 cases; in 35 the variant was identified as MVs/GirSomnath.IND/42.16/ of genotype D8, and in the other two, genotype A (vaccine), so they were ruled out.
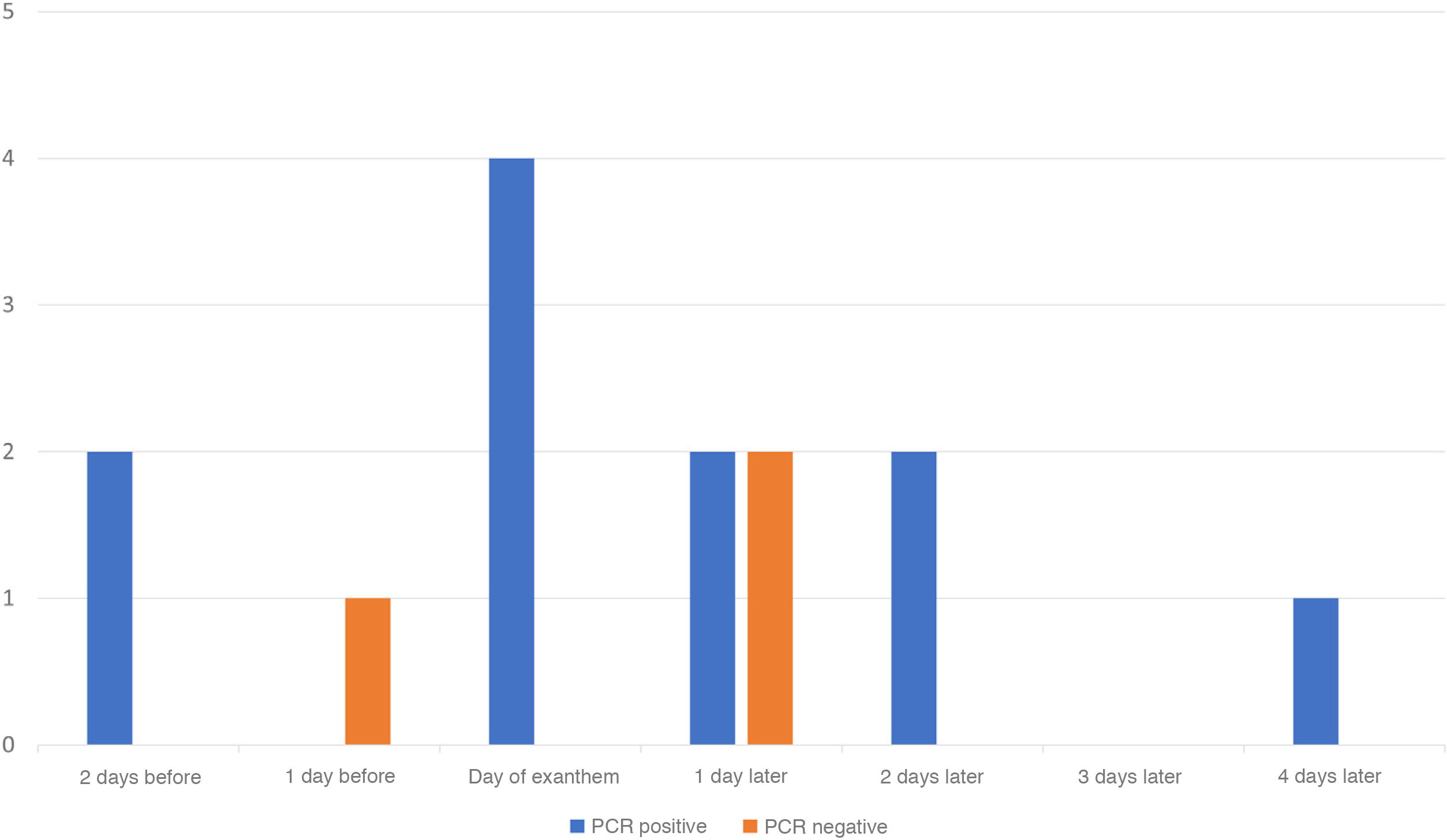
Serum PCR was performed on 14 serum samples from 14 patients with negative IgM in their initial sample, and in those in whom the diagnosis of measles was subsequently confirmed. In 11 cases it was positive. These samples were collected between two days pre-exanthem and four days post-exanthem. The other three serum PCR tests were negative (Fig. 1). Of the three negative samples, two belonged to vaccinated patients. In the third, although the patient's vaccination status was unknown, he was IgG positive and IgM negative at the onset of the clinical picture.
The index case of the outbreak in Guadalajara was a woman who went to the hospital to visit a relative, causing secondary cases at the health centre. From this case, it was possible to establish up to 10 chains of transmission, four of which were related to health centres.2
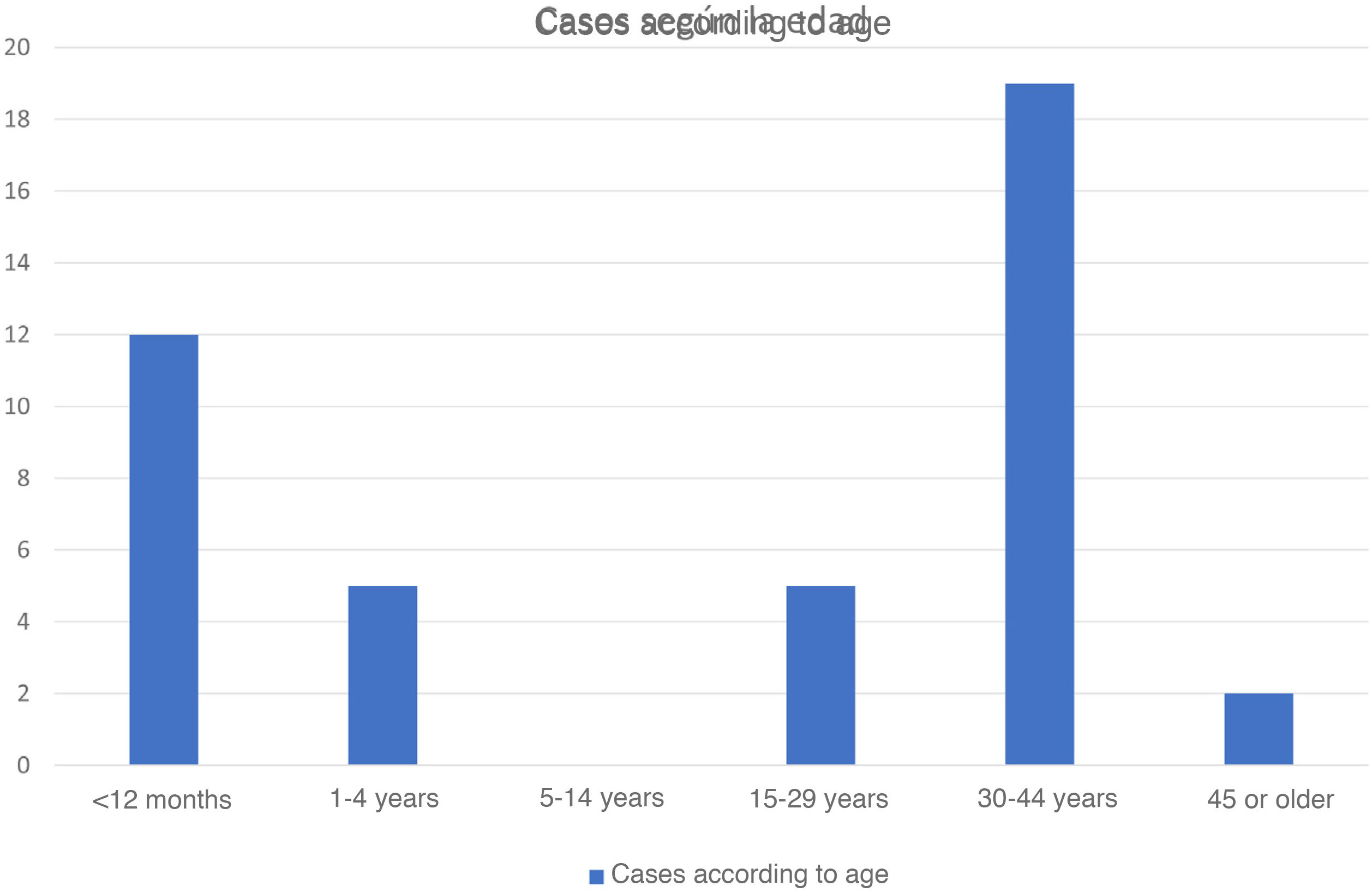
Of the diagnosed cases, 22 were women and 21 were men. In terms of age distribution, two groups were observed: 26 adults aged between 25 and 53 years and 17 children between four months and three years old (Fig. 2). The diagnosis of two four-month-old children, twin brothers who were negative for IgG at the beginning of the clinical picture in both cases, and whose mother was also diagnosed with measles stands out. In 11 patients there is evidence of having received a dose of the vaccine, in nine of having received one dose and in two, of two doses. In three vaccinated patients, the serological profile of the first sample received was positive for IgG and negative for IgM (Table 2). The diagnosis was made in all of them by oropharyngeal swab PCR.
Cases of vaccinated patients diagnosed with measles.
| Case | Age | No. of doses | IgM | IgG initial clinical picture | IgG* Increase | Throat PCR | Genotype |
|---|---|---|---|---|---|---|---|
| 1 | 34 y | 1 | Pos | Neg | ND | Pos | D8 |
| 2 | 34 y | 1 | Neg | Pos | ND | Pos | D8 |
| 3 | 25 y | 1 | Pos | Pos | Yes | Pos | D8 |
| 4 | 28 y | 2 | Neg | Pos | ND | Pos | D8 |
| 5 | 3 y | 1 | Pos | Pos | ND | Pos | D8 |
| 6 | 3 y | 1 | Pos | Pos | ND | Pos | D8 |
| 7 | 13 m | 1 | Neg | Neg | ND | Pos | D8 |
| 8 | 7 m | 1 | Neg | Neg | ND | Pos | D8 |
| 9 | 13 m | 1 | ND | ND | ND | Pos | D8 |
| 10 | 24 y | 2 | Neg | Pos | Yes | Pos | D8 |
| 11 | 36 y | 1 | Neg | Pos | ND | Pos | D8 |
ND, not done; Neg, negative; m, months; PCR, polymerase chain reaction; Pos, positive; y, years.
The following complications were diagnosed: 13 cases of acute hepatitis, five of diarrhoea, two of otitis, and one of keratitis. The 13 patients with hepatitis presented with a significant increase in the ALT enzyme (more than double the upper limit of normal). This mainly affected unrelated young subjects, 12 adults (25–47 years, mean: 36 years) and one child. Liver involvement was the reason for admission for all adult patients.
The most common symptoms in this group of hospitalised patients were: skin rash (present in 100%), fever (also present in 100%), arthromyalgia (which appeared in 77%) and Koplik's spots (seen in 54%).
Regarding laboratory test abnormalities, along with increased ALT, all adult patients also presented at admission with increased AST, GGT and LDH enzymes. In the case of the paediatric patient, these alterations were not observed during admission, but rather in the control laboratory tests one month after hospital discharge.
Five of the patients with liver involvement also presented with elevated total bilirubin. Together, 46% presented with jaundice with bilirubin levels >1.2 mg/dl. Hepatotropic virus serology (HAV, HBV, HCV, CMV, and EBV) was requested in all these patients, with negative results in all cases. The diagnosis of toxic hepatitis was ruled out by anamnesis. Due to the laboratory test alteration of the liver profile, an abdominal ultrasound was requested to complete the study, without finding relevant findings in any of them.
After a short period of hospitalisation, in no case longer than seven days, the patients evolved favourably, improving both clinically and regarding laboratory tests, receiving symptomatic treatment with antipyretics and serum therapy. No patient presented with any complication that led to prolonged admission or required intensive measures, or admission to the ICU.
DiscussionMeasles is currently the most common cause of infant death from an infection that is nonetheless preventable through vaccination. Most deaths occur in developing countries due to complications of the disease.1
This situation has led the WHO to carry out programmes to achieve its elimination. These programmes are based on the correct vaccination of the population, with vaccination coverage ≥95%, as well as the implementation of sensitive and specific surveillance systems based on case detection. Given its high contagiousness, with a secondary attack rate of over 90%, early diagnosis is essential.
Diagnosis was traditionally based on the clinical picture of the patient with the characteristic exanthem, together with high fever and conjunctivitis, coryza and/or cough, and the appearance of specific IgM in serum. However, any clinical suspicion must be confirmed with laboratory tests. IgM usually takes several days to be detectable (≥4 after the exanthem), leading to a delay in diagnosis.7 On the other hand, in post-elimination countries with low circulation of the virus, the negative predictive value of IgM decreases, since the cases in those who have been vaccinated increase, and in these cases it may not appear,4,8 as well as the fact that the positive predictive value decreases, increasing the cases of false positives of IgM.9 In our study, in 14 cases IgM was not detected in the first serum sample obtained. Additionally, a vaccinated and asymptomatic health worker with contact with a case and positive IgG and IgM was ruled out. It has been previously described that in some people with previous contact with the virus, an antigenic immunologic stimulation may occur after a new contact, causing the production of IgM.10
The use of genomic detection techniques such as oropharyngeal or urine sample PCR provides a laboratory diagnosis prior to the appearance of IgM. In our study, 15 patients attended a health centre between 48 h before and on the day of the appearance of the exanthem. This was due both to the presence of nonspecific symptoms and to the existence of contacts diagnosed in the context of an epidemic outbreak. In the case of serum, although it is not an optimal sample for the detection of viral RNA, it has been described that it can be detected in the first few days of the disease, usually being negative when the IgG appear.11 Its fundamental utility would be in patients with a short evolution, in whom, exceptionally, we do not have other samples (oropharyngeal swab or urine) for PCR and who have not received the vaccine. In one study, the highest profitability was found in the first 72 h after the appearance of the exanthem.12 However, obtaining a throat swab, which can be completed with urine, is essential in all suspected cases of measles to ensure adequate diagnostic performance.13,14
In the present study, as well as in previous studies,3,15,16 cases of measles in vaccinated patients have been described. This may be due to both primary and secondary vaccine failure. To differentiate between situations, a post-vaccine serological study would be necessary. However, the presence of IgG with the absence of IgM at the time of diagnosis suggests secondary vaccine failure.17 Vaccinated patients are considered less contagious, but outbreaks can occur.18 In these patients, diagnosis is more complex because the symptoms are milder and because of the difficulty in serological interpretation with absent IgM together with lower viral excretion.17 This reinforces the need to take a full set of samples in all suspected measles cases. In addition, in the surveillance of outbreaks we must take into account the existence of these cases in vaccinated patients, and not rule out cases due to the presence of IgG at the beginning of the clinical picture together with the absence of IgM in samples collected early. In these cases, molecular diagnosis is essential.
The study of IgG avidity in these patients is a tool that can complement the rest of the diagnostic tools and allows us to characterise vaccine failure.19
The analysis of the genotypes detected in an outbreak provides local information, allowing us to rule out cases of vaccine reactions,4,20 such as the two 12-month-olds who received the first dose in our study. On the other hand, molecular surveillance allows to relate cases with others that may occur simultaneously in other locations, and provides information on the predominant genotypes globally.4,7,21–23 In our case, the identified variant of the D8 genotype (MVs/GirSomnath.IND/42.16/-variant) circulated predominantly in Europe. In Spain, throughout 2018 and 2019, various sporadic cases of this variant, originally from India and imported to the rest of Europe, mainly from Ukraine, have been identified. In 2019, this variant was detected in the outbreaks in Valencia, which began at the end of 2018, Barcelona, Tenerife and Madrid.
The outbreak described in this study presents the characteristics of outbreaks in a country in the post-elimination phase, affecting an age group of young adults at the beginning of the outbreak and later unvaccinated children or children who have had one dose of the vaccine. In the group of adults, there are two subgroups: the majority group of unvaccinated people or those with incomplete vaccination, as since the introduction of the triple viral vaccine in 1981, it took a few years to achieve high coverage. As the virus circulation was significantly reduced, they also did not acquire the infection naturally; and another group of fully vaccinated individuals who present with vaccine failure, probably due to an evanescence phenomenon with a decrease in vaccine protection over time.24 This data has already been reported in the Netherlands in people born between 1975 and 1985.25 The low incidence of the disease means there is no booster effect in those who have been vaccinated, increasing the susceptible population over time.
In addition to the characteristic symptoms of measles, pneumonia or hepatitis are sometimes observed, the latter mainly in adults.26,27 In the outbreak that occurred in the health district of Guadalajara, liver involvement as a symptom of the disease is notable. An increase in ALT was observed in 13 patients. Measles-associated hepatitis is usually detected as a transient increase in transaminases during the acute phase of the disease. Liver involvement associated with measles can present two patterns: on the one hand, hepatocellular damage characterised by increased levels of transaminases, which is a reflection of the cytopathic effect due to the direct action of the virus28; and on the other, a second late cholestatic pattern due to the action of the patient's immune system.29
In the event of any suspicion of measles, urgent notification to the health authorities of these cases and their subsequent confirmation is necessary.4,7 For this, oropharyngeal, urine and serum samples must be collected for molecular and serological study, and the temporal relationship between obtaining the sample and the clinical picture must be identified. The collection of the samples for the molecular study should be conducted as early as possible, while a second serum sample may be necessary for the serological study.30 This is even more important in the cases of vaccinated people and adults.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: González-Praetorius A, Fernández-García A, Pérez-Olmeda M, García-Rivera MV, Caballero-López B, Gilaberte-Reyzabal S, et al. Brote de sarampión en el área sanitaria de Guadalajara (España): dificultad en el diagnóstico microbiológico en la era de su eliminación, Enferm Infecc Microbiol Clin. 2022;40:532–538.