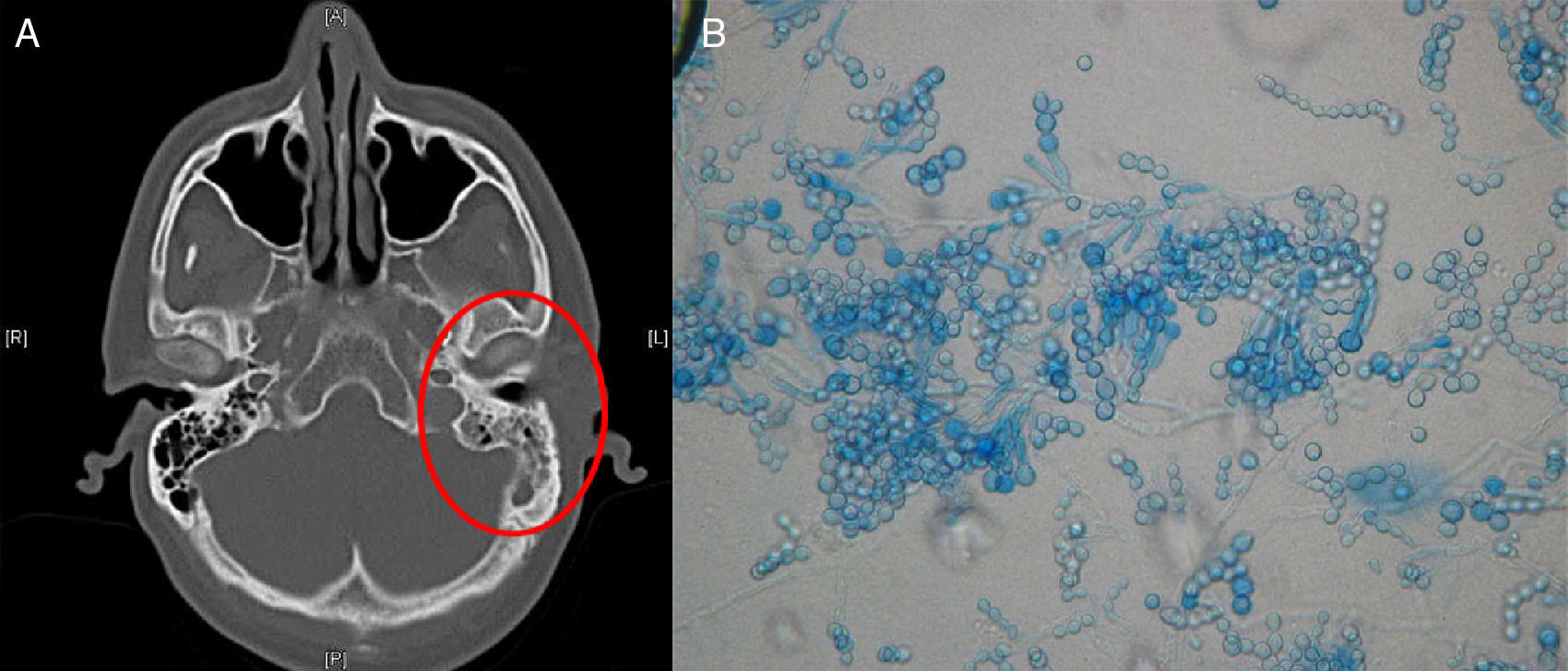
This article studies the case of a 38-year-old male patient with no history of interest. He reported regular contact with farm animals and takes part in water sports. He came to the clinic with purulent otorrhoea and oedema of the left external auditory canal (EAC). He received topical empirical treatment with gentamicin and dexamethasone. After 10 months, he returned to the clinic due to still having painless otorrhoea. Examination with an otoscope revealed dermal and cartilaginous necrosis and non-marginal perforation of the eardrum, associated with indurated dermatitis of the auricle. He had non-tender lymphadenopathy in the left posterior triangle of the neck. He had no fever, dysphonia or weight loss. Human immunodeficiency virus screening and tests for autoimmune disorders were negative. Biopsies were taken from the EAC for microbiological and anatomical pathology testing and a computed axial tomography (CT scan) of the ear was ordered. The patient was treated with linezolid and oral ciprofloxacin. The CT scan showed opacification of the left epitympanic region, with a soft tissue mass in the internal and lateral portion, with opacification of the mastoid cells and tympanic cavity, secondary to the concomitant inflammatory process due to perforation of the eardrum which is consistent with the diagnosis of outer ear infection with integrity of the ossicular chain (Fig. 1A).
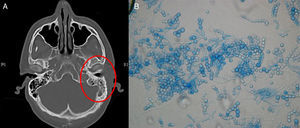
Main diagnostic signs of otitis externa due to Scopulariopsis brevicaulis. (A) Head CT showing opacification of the mastoid cells and chondritis of the EAC, on the left side. (B) Lactophenol blue staining (40×) after 7 days of incubation: spherical conidia with truncate base in chains.
Anatomical pathology revealed hyperkeratosis and chronic inflammation of the soft tissue along with necrotic lesions with thrombotic phenomena. Periodic acid-Schiff and Grocott methenamine silver stains were negative as were microbiological cultures.
At a check-up performed one month later, no improvement was observed and areas of necrosis within the EAC had continued to spread; new specimens were sent for microbiological analysis.
A KOH test showed irregular hyphae and oval conidia in chains. Gram staining showed abundant hyphae. Yeast only grew in cultures after incubation for 48 hours at 37°C. Colonies on Sabouraud agar plates were white, velvety and turned a brown colour at day five. Lactophenol blue staining (×40) of colonies showed septate hyphae, swollen conidiophores and spherical conidia with wide truncate base in chains, which are characteristic of the genus Scopulariopsis (Fig. 1B). Yeast were identified using MALDI-TOF (Bruker®) mass spectrometry, via total extraction of the isolate, revealing Scopulariopsis brevicaulis in the first 7 patterns reported. Although the score was 1.759, the result was deemed to be correct as it was consistent with the morphological identification.1 The National Centre for Microbiology confirmed this identification by morphological analysis. Likewise, antifungal susceptibility tests were conducted based on recommendations of the Subcommittee on Antifungal Susceptibility Testing of the European Committee for Antimicrobial Susceptibility Testing, obtaining the following results, expressed in mg/l: amphotericin B, MIC >16; itraconazole, MIC >8; voriconazole, MIC >8; posaconazole, MIC >8; terbinafine, MIC >16, and caspofungin, MIC=8. Although no antifungal susceptibility testing breakpoints have been defined for this microorganism, observed and expected in vitro activity was limited.2–6
The patient's ear was cleaned surgically and voriconazole (300mg/12h) was administered. A major improvement with re-epithelialisation of the EAC was observed at 6 weeks and control cultures were negative. The same treatment was prescribed for another month without the patient visiting the clinic for a check-up or experiencing any recurrence.
Hennequin et al.7 and Besbes et al.8 reported two patients with otomycosis due to S. brevicaulis who had previously undergone tympanoplasty and cholesteatoma surgery, respectively. Issakainen et al.9 studied 13 cases of otitis externa due to Scopulariopsis spp. and only 7 had underlying diseases.
The patient whose case we are presenting had no predisposing factors and the infection was considered to possibly be due to unperceived microtrauma to the EAC. The patient also showed no onychomycosis, an infection often caused by S. brevicaulis.10
The presence of S. brevicaulis in pure cultures and the patient's clinical outcome and response to treatment, with no other confirmed aetiology, affirmed that this microorganism was the causal agent.
A differential diagnosis of malignant otitis externa was performed, but the absence of osteolytic lesions and granulomas in the EAC ruled out this condition.
Invasive infection due to S. brevicaulis is uncommon and has been described mainly in immunocompromised patients, but may occur in immunocompetent individuals and tends to have a good prognosis.3–6 There is no established therapy, although some authors indicate voriconazole to be the most effective antifungal in vivo and it is a good therapeutic option in association with surgical debridement of the lesion.6
Please cite this article as: de Miguel-Martinez I, Hernandez-Cabrera PM, Armesto-Fernández MA, Martín-Sánchez AM. Otitis externa necrosante causada por Scopulariopsis brevicaulis en un paciente sin factores predisponentes. Enferm Infecc Microbiol Clin. 2018;36:62–64.