This was a 36-year-old male patient with a history only consisting of mononucleosis in childhood, smoking, occasional use of alcohol and snorting of cocaine.
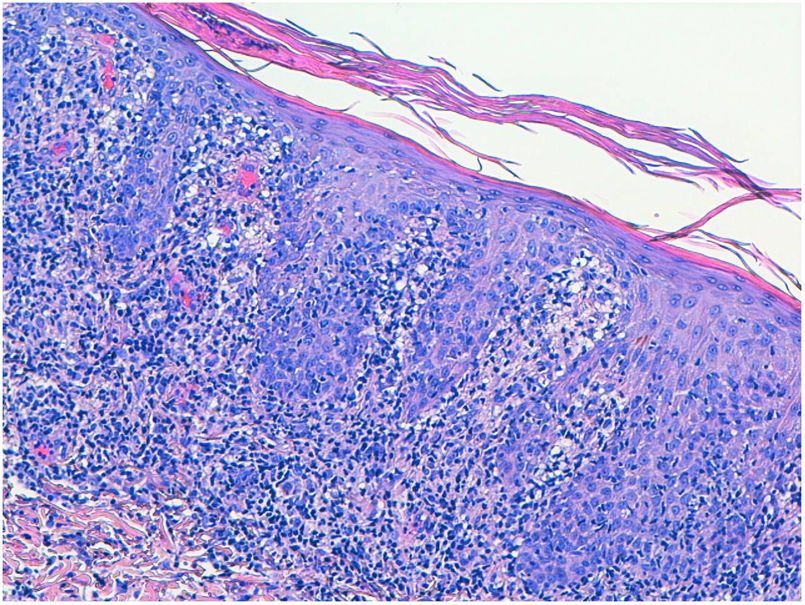
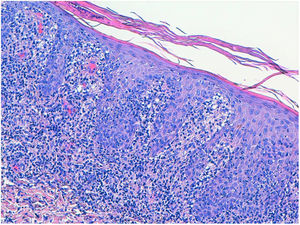
One month earlier, he had developed lesions (Fig. 1), at first vesicular, predominantly on the trunk, scalp and limbs. The lesions were not pruritic, but had a tendency to progress by becoming larger and developing a necrotic background and a raised erythematous border. Viral aetiology (chickenpox) was initially suspected and he was given a seven-day course of topical and oral antiviral treatment, but without improvement. Examination revealed the above-mentioned lesions and left laterocervical lymphadenopathy, with no other abnormalities of note.
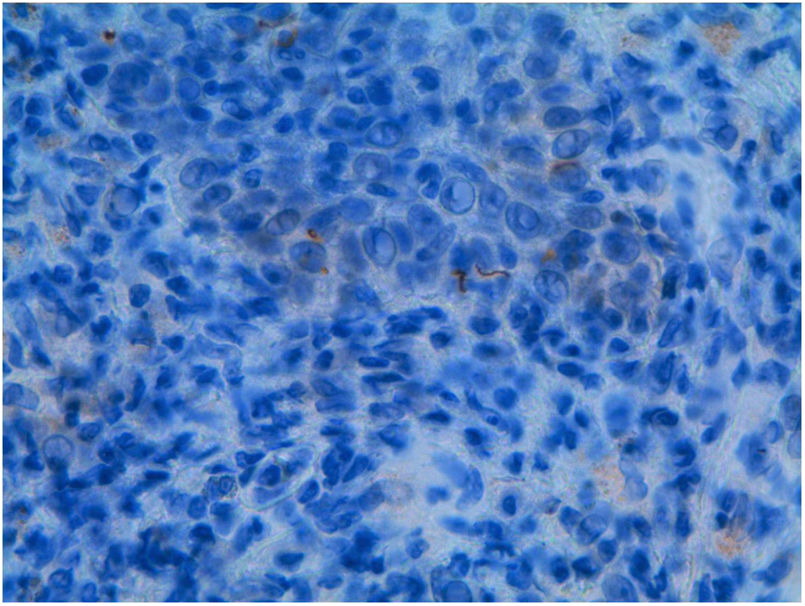
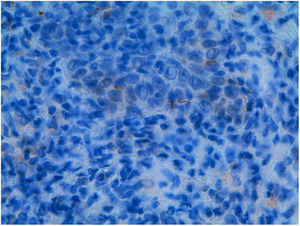
OutcomeHIV serology came back positive, with plasma viraemia 133,000 copies/mL (log 5.1) and CD4 lymphocytes 220/mm3. Screening for other sexually transmitted diseases ruled out hepatitis A, B and C, with the result for treponemal tests positive, TPPA 4 (+) and positive for Treponema pallidum antibodies. RPR 1/1 was negative due to possible prozone effect (false negative result in non-treponemal tests that can be observed in patients with HIV infection). Pathology study of the lesions using immunohistochemical techniques (Figs. 2 and 3) showed the presence of spirochetes in the epidermis. The symptoms in conjunction with the pathology results pointed to the diagnosis of malignant syphilis (MS). In view of the patient's situation, we performed an ophthalmological examination and lumbar puncture to rule out silent involvement of other organs due to his state of immunosuppression, with both being normal.
He was started on antiretroviral treatment with dolutegravir, emtricitabine and tenofovir. We treated the condition as late latent syphilis due to his state of immunosuppression, with three weekly doses of benzathine penicillin G 2.4 MU.
At follow-up after five weeks, the necrotic lesions had disappeared, leaving hyperpigmented macules.
DiscussionCo-infection between HIV and syphilis is complex and patients may have altered serological response to infection, inadequate response to treatment or atypical clinical manifestations.1 MS is a secondary, aggressive ulcerative form of syphilis, affecting a patient’s general condition as a result of occlusive endarteritis caused by the infection.2 It presents with disseminated pustules which evolve into ulcerated nodules with a necrotic or hyperkeratotic surface, occasionally with a rupioid or ostraceous appearance.3,4 They predominate on the trunk and limbs, but can also affect the mucous membranes, palms, soles and scalp. Fever and constitutional symptoms may precede cutaneous symptoms. The immune status of these patients does not seem to be a determining factor for the development of MS, as 80% of those infected with HIV have more than 200 CD4/mm3 and none of them had suffered from a previous opportunistic infection.
All of that points to a possible interaction between Treponema pallidum and the HIV or a functional immunological defect as possible reasons for the development of the disease, rather than a quantitative immunological deficiency.5
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Suso Estívalez C, Arazo Garcés P, Torrecilla Idoipe N, García Bruñén JM. Lesiones costrosas a estudio. Enferm Infecc Microbiol Clin. 2020;38:498–499.