Nocardia spp. is a filamentous, branching Gram-positive bacteria that can cause serious infections in immunocompromised patients.1 Since the 1970s, cases of nocardiosis have been reported in solid-organ transplant recipients.2 In oncohaematological patients, infections caused by Nocardia have been documented in haematopoietic stem cell transplant recipients.3
Acquired bone marrow aplasia is an immunomodulatory disease that presents with bone marrow failure. Treatment for this disease essentially consists of immunosuppression.4 We report 2 cases of systemic nocardiosis in patients with bone marrow aplasia who did not undergo a bone marrow transplant.
Case 1An 83-year-old woman diagnosed with bone marrow aplasia was not offered a bone marrow transplant due to her age.
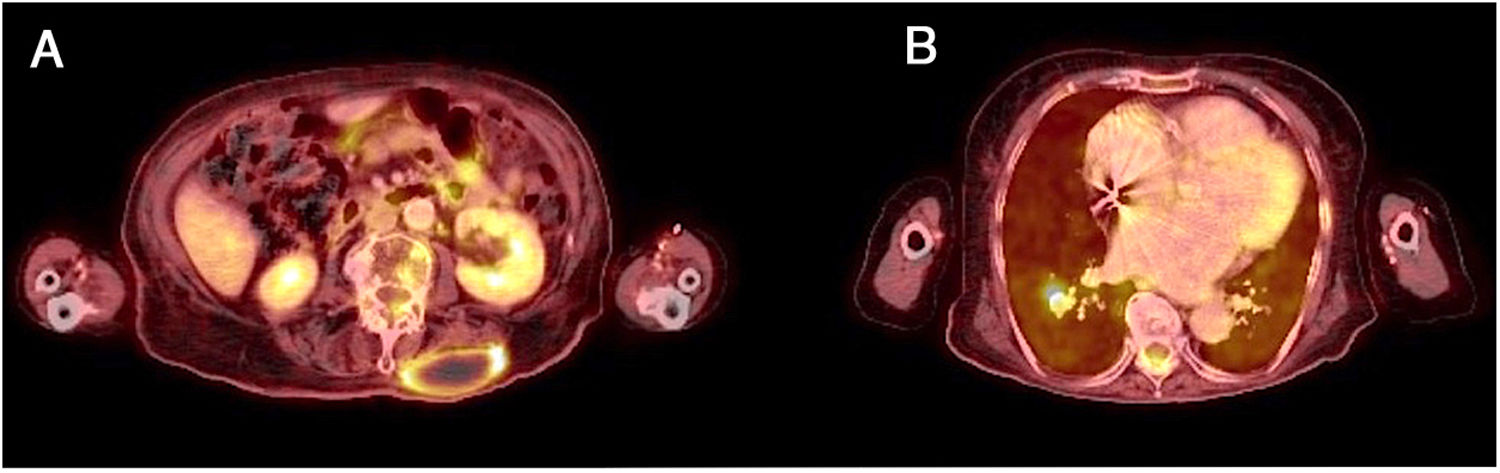
The patient was hospitalised with signs and symptoms consisting of fever for 15 days, asthenia and lumbar pain. Her fever persisted despite treatment with amoxycillin, and a previously absent palpable mass was detected in her lumbar spine. A computed tomography/positron emission tomography (PET-CT) scan showed a left paravertebral collection with peripheral enhancement (Fig. 1A), as well as a hyperenhancing right lung nodule (Fig. 1B). Fine-needle aspiration was performed on the lumbar abscess for microbiological culture which isolated Nocardia cyriacigeorgica susceptible to co-trimoxazole, amikacin, linezolid and doxycycline and resistant to quinolones. Antibiotic treatment was started with meropenem and amikacin for 2 weeks, after which the patient started to improve. The patient was discharged with oral antibiotic treatment with co-trimoxazole and doxycycline. This combination was maintained for 8 months with no adverse side effects, and the patient showed complete resolution of the lesions 6 months after her hospitalisation.
Case 2A 51-year-old man diagnosed with severe acquired bone marrow aplasia at age 23 declined to undergo a bone marrow transplant. For this reason, he remained on immunosuppressant treatment including various agents over time including cyclosporine, steroids and mycophenolate mofetil. At age 46, the patient was fitted with a hip prosthesis due to avascular necrosis of the right femoral head caused by his steroid treatment.
He was hospitalised 6 years later due to fever and increased right leg volume following an accidental fall. The injury was accompanied with local erythema and a marked increase in temperature. A CT scan revealed a large collection extending to the quadriceps and abductor muscles (Fig. 2A). The culture obtained through aspiration of the collection isolated Nocardia farcinica resistant to third-generation cephalosporins but susceptible to carbapenems, amikacin and co-trimoxazole. A study of the central nervous system (CNS) using magnetic resonance imaging revealed a round lesion on the frontal lobe which showed vasogenic oedema and peripheral enhancement (Fig. 2B), consistent with a CNS abscess.
The patient was diagnosed with disseminated nocardiosis with CNS symptoms and initially treated with meropenem, amikacin and co-trimoxazole. He had to be admitted for surgery to drain the periprosthetic abscess; however, his fever disappeared when antibiotics were started. Despite his initial recovery and resolution of nocardiosis-related lesions, including his cerebral nocardiosis, the patient died 3 months later of invasive pulmonary aspergillosis.
The incidence of nocardiosis in other conditions unrelated to transplant — such as bone marrow aplasia — is unknown and likely to be underestimated. It is unclear how Nocardia invades the host; as it is an omnipresent germ, accidental contact can cause infection. Our second case showed a clear relationship between an injury and the development of abscesses in the same area. Nocardiosis generally develops in a subacute or chronic fashion and may go unnoticed; therefore, strong suspicion is essential for its diagnosis.
Most recommendations include initial combination therapy, preferably with 2 active antibiotics, although there is no standard treatment. Following intravenous treatment which may last up to one month, treatment with oral antibiotics must be maintained for 6–12 months. Co-trimoxazole is the antibiotic of choice for outpatient treatment.5
Regarding our cases, choosing an antibiotic regimen was complicated due to the bone marrow toxicity caused by co-trimoxazole. Alternative agents such as doxycycline or quinolones may be selected with the help of an antibiogram for prolonged treatment with good results.
FundingNo specific funding was used for drafting this manuscript.
AuthorsMarquet-Palomanes J: wrote the document.
Martín-Moro F, Fortún J and López FJ: contributed equally to its review.
Please cite this article as: Marquet-Palomanes J, Martín-Moro F, Fortún-Abete J, López-Jiménez J. Nocardiosis sistémica en pacientes con aplasia medular adquirida: descripción de 2 casos. Enferm Infecc Microbiol Clin. 2021;39:51–52.