To determine nurses’ knowledge level regarding physical restraint use in intensive care units and its associated factors.
MethodA cross-sectional multicentre study was carried out in 12 critical care units of 8 hospitals in Spain (n=354 nurses). An ‘ad-hoc’ knowledge survey was developed, and their content was validated by experts. The survey obtained a test-retest stability of ICC=.71 (95% CI: .57–.81) in a previous pilot study. A final 8-item tool was designed. Sociodemographic and professional variables from the participants were collected; as well as structural and clinical variables from the units analysed. A descriptive and association analysis between variables was performed. A p-value<.05 was deemed statistically significant.
ResultsTwo hundred and fifty nurses answered the survey (70.62%). Mean age of the participants was 36.80 (SD 9.54) with 10.75 (SD 8.38) years of professional experience in critical care. Seventy-three point six percent had never received previous training about physical restraints. Knowledge mean value was 4.21 (SD 1.39) (range 0–8). Knowledge level was associated with the referral hospital (p<.001). Nurses with a higher knowledge level are more likely to work in units with informed consent sheets for physical restraint use (p<.001); flexible family visiting (p<.001); analgo-sedation protocol (p=.011), and units in which nurses had autonomy to manage analgo-sedation (p<.001). Individual sociodemographic and professional data was not associated with knowledge level.
ConclusionsFurther training regarding physical restraint use is needed for critical care nurses. The work environment where nursing care is given has a great influence on nurses’ knowledge level about this intervention.
Determinar el grado de conocimientos de las enfermeras sobre el uso de contenciones mecánicas en las unidades de críticos y los factores relacionados.
MétodoEstudio multicéntrico, observacional, en 12 unidades de críticos de 8 hospitales en España (n=354 enfermeras). Se elaboró una encuesta ad-hoc de conocimientos cuyo contenido fue validado por expertos. La encuesta obtuvo una estabilidad test-retest de CCI=0,71 (IC 95%: 0,57-0,81) en un estudio piloto previo. El instrumento final quedó conformado por 8 ítems. Se recogieron datos sociodemográficos y profesionales de los participantes, así como variables estructurales y clínicas de las unidades a estudio. Se llevó a cabo un análisis descriptivo y de asociación entre variables. Se consideró estadísticamente significativo un valor de p<0,05.
ResultadosRespondieron 250 enfermeras (70,62%), con una edad media de 36,8 (DE 9,54) años y una media de 10,75 (DE 8,38) años de experiencia profesional en unidades de críticos. El 73,6% no había recibido formación previa sobre contenciones mecánicas. La media de conocimientos fue de 4,21 (DE 1,39) (rango 0-8). El grado de conocimientos se asoció al hospital de referencia (p<0,001). Las enfermeras con mayor grado de conocimientos es más probable que trabajen en unidades con consentimiento informado para el uso de contenciones mecánicas (p<0,001); visita familiar flexible (p<0,001); y que dispongan de protocolo de analgosedación (p=0,011), o que la enfermera tenga autonomía en el manejo de la analgosedación (p<0,001). Ningún dato sociodemográfico ni profesional individual se asoció al grado de conocimientos.
ConclusionesEs necesaria una mayor formación de las enfermeras sobre el uso de contenciones mecánicas. El entorno de trabajo donde se desarrollan los cuidados tiene una gran influencia en el grado de conocimientos de las enfermeras sobre esta intervención.
The more nurses know about physical restraint, the less they report its use. Educational programmes have been demonstrated as effective in improving the level of knowledge of intensive care nurses and in reducing the use of restraint, with no higher occurrence of adverse events.
What is the contribute of this?Nurses in critical care units have moderate knowledge of physical restraint, therefore more training and awareness is needed on this subject. Individual sociodemographic and professional characteristics have little influence on levels of knowledge. The working environment where care is delivered greatly influences the level of knowledge of this intervention.
Implications of the studyContent on the reflective use of physical restraint must be included in training courses on patient safety in hospitals and universities. Identifying structural and clinical factors that affect the level of knowledge about physical restraint will enable organisations to act to improve the training of their practitioners in this regard. Further and ongoing research is needed on how knowledge affects this issue in actual practice.
More than half the patients admitted to intensive care units (ICU) experience agitation caused by pain, delirium, abstinence from smoking or alcohol, sedation withdrawal, electrolyte imbalance, fever, inability to communicate and distress, and other additional factors.1,2 To manage these episodes, and with the aim of preventing self-removal of life-sustaining devices such as endotracheal tubes, nurses routinely employ physical restraint (PR), using wrist, chest or abdominal restraint straps, for example.3,4
According to Bleijlevens et al.,5 PR is “defined as any action or procedure that prevents a person's free body movement to a position of choice and/or normal access to his/her body by the use of any method, attached or adjacent to a person's body that he/she cannot control or remove easily”.
However, the use of these measures is not free from controversy, since they have not been demonstrated as safe or effective in preventing these adverse events6,7 and, moreover, they infringe upon the inherent qualities of the person, such as their dignity and autonomy. Similarly, the use of PR has been associated with increased agitation and prevalence of delirium; it jeopardises the relationship of trust between the nurse and their patient, by placing the patient in a position of greater vulnerability.1,8,9
Although both the international recommendations and the document on quality indicators lead by the Spanish intensive care medical and nursing societies advise that the decision to use PR should be multidisciplinary, prescribed by a doctor and recorded in writing in the clinical history,10–12 currently, in most ICU, it is the nurses who decide, place, maintain and remove these devices autonomously.3,4,13,14
In light of this reality, since the beginning of the nineteen eighties many papers have focussed on identifying the knowledge of critical care nurses about PR and its correlation with attitudes and clinical practice. Overall, the results of these studies conclude that ICU nurses have moderate knowledge about PR.15–19 Eskandari et al.,16 in a sample of Malasian nurses from both hospital and critical care units, report that the level of knowledge is influenced by academic qualification, knowledge of the hospital policy on PR, the unit studied and previous training on restraint, which is also reported by Suliman et al.19 However, this association between knowledge and academic qualifications or years of professional experience is not corroborated in other studies.18,20 Likewise, a correlation has been demonstrated between the level of knowledge and self-reported practices; the use of PR being less likely the greater the level of knowledge.15,16
Along these same lines, the implementation of programmes with educational sessions on the myths and risks of PR, alternatives, the ethical considerations linked to this practice, the results of scientific evidence, institutional regulations and nursing care required have proven effective in improving levels of knowledge and minimising the use of restraint without an increased occurrence of adverse events. However, these studies were undertaken in different contexts to ours, with small samples, and monitoring of the effect of this training over time was limited.20–23
The instruments used in the various studies to assess knowledge are heterogeneous, which makes comparison of results difficult. The best-documented of these instruments is the Physical Restraint Questionnaire (PRQ),18,24,25 which has been adapted and modified in different languages.15,16,19,23,26 However the statements in this subscale of the PRQ are very general, they were prepared before the international recommendations on the use of PR in ICU, and do not cover specific questions in relation to the specificities of the critical patient.
In our country, we only have 2 studies on the prevalence of the use of PR in ICU, which varies from 15% to 45%.13,27 Moreover, it has been documented that the management of these restraining devices varies according to the units studied.28 In the context of ICU, no paper has explored the knowledge of critical care nurses about PR, or the factors that might influence this knowledge. Therefore, the aim of this study was to establish the level of knowledge of nurses on the use of PR in critical care units and related factors.
MethodStudy design and scopeA multi-centre, observational study carried out in 12 critical care units of 8 public and private hospitals in Spain.
SubjectsThe participants were nurses working in the abovementioned adult critical care units during the study period. Nurses were included who were members of the hospitals’ regular staff, under full-time, part-time or temporary contracts, provided they were usually assigned to the department, with professional experience of more than one year, and who agreed voluntarily to take part in the study. Nurses with contracts of less than 10h per week, professionals on leave, long-term sick-leave, temporary incapacity for work or any other type of leave from work exceeding one year were excluded from the study. Each unit was asked the total population of nurses likely to participate in the study. The target population was 360 professionals. The entire population was given the questionnaire consecutively.
VariablesThe variables were organised into 3 groups: variables relating to knowledge about PR; sociodemographic variables (age, sex), and the professional variables of the respondent (academic qualification, years of professional experience in critical care, work shift, type of work contract, previous training on PR); and structural and clinical variables of the units under study (type of hospital, type of unit, number of beds, nurse: patient ratio, type of family visits, existence of a PR protocol, people who decide the use or removal of PR; prescription for the use of PR, request for informed consent prior to the use of PR, recording the use of PR, existence of a multidisciplinary analgo-sedation protocol; autonomy of the nurse in managing analgo-sedation at the bedside). Having undertaken any course, session or talk in conferences on PR was specified for the previous training on PR variable.
InstrumentsTwo measurement instruments were used: a survey on knowledge that included the sociodemographic and professional variables; an annexed document with all the structural and clinical variables of the units.
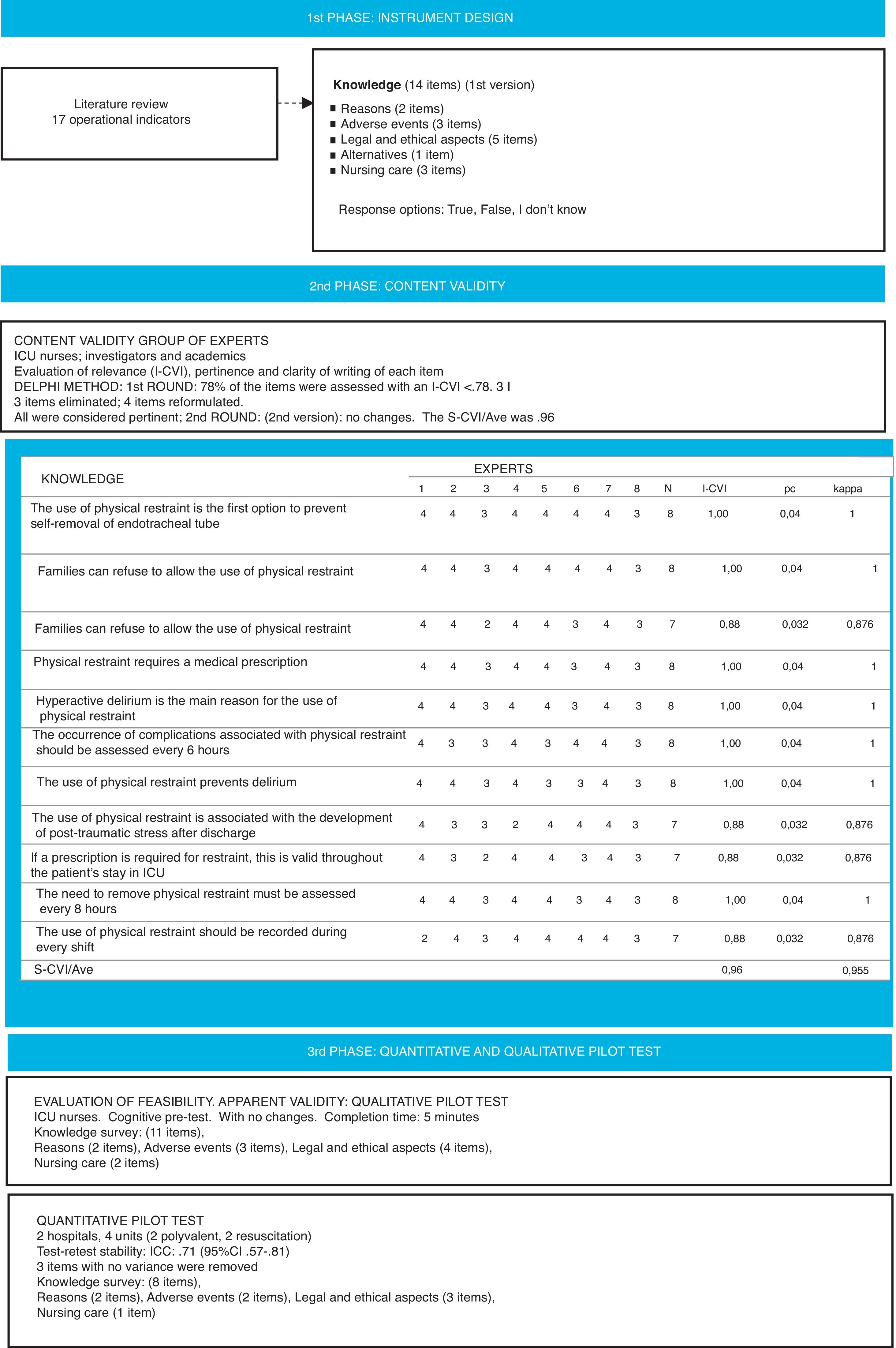
Design and generation of the questionnaire itemsThe survey on knowledge was designed from a list of 17 indicators generated based on a review of the literature on PR, and the subscale of knowledge of the PRQ was taken as the benchmark. The keywords used in the review were: (restraint, physical, restraint OR mechanical restraint); (critical care OR intensive care units); (nurs* OR critical care nurs*). The criteria for uniformity of expression recommended by Argimon and Jiménez29 were used for drawing up the survey items and understanding, relevance to the context of critical care and its importance were considered. The first version comprised 14 items with 3 response options: “true”, “false”, “I don’t know”. The items covered aspects relating to the reasons for using PR (2 items), adverse events (3 items), ethical recommendations (5 items), nursing care (3 items), and alternatives to using PR (one item).
Content validityA panel of 8 expert nurses at a national level were invited to analyse the instrument's content validity, known for their professional careers in the area of intensive care, nurse teaching and research who assessed the relevance, pertinence and clarity of wording of each proposed item based on the Delphi method.30 The principal investigator (PI) and the experts communicated by email throughout the process.
The content validity index (CVI) was used to assess the instrument.31 This is a classical index where each expert rated the relevance of each item (I-CVI), on a 4-point Likert scale, where 1=not at all relevant, 2=quite relevant, 3=very relevant and 4=extremely relevant. They were also asked to assess the clarity of the writing as “good”, “acceptable” or “poor”. A suggestions section was added where the experts could clarify their assessments, state whether they considered any item not to be relevant, and make comments and proposals for improvement. The I-CVI was calculated for each item, the probability of a chance agreement among the experts (Pc), and the modified kappa index. Finally, the CVI of the entire survey was calculated from the mean score for the items (S-CVI/Ave). Bearing in mind that the expert panel comprised more than 5 people, items with an I-CVI of ≥.78 were considered to have acceptable validity, and an excellent agreement was considered if the modified kappa index was ≥.74. Similarly, an S-CVI/AVE ≥.90 was considered adequate for the entire survey.31 In the event of lower assessments, the item and the suggestions of the experts were revised. The experts had 3 weeks to return the assessments for the first Delphi round. A database was prepared with the first results with the grouped assessments, and a new document was formed comparing the items of the first version with the new items proposed. The proposed changes could be to (1) remove the item, (2) modify the way it was written, or (3) include a new item in the questionnaire. This document, together with the new version of the questionnaire (version 2), were sent again to the same experts for them to complete the second Delphi round. The assessors had 2 weeks to complete this second round. Finally, the third version of the questionnaire was created with the results of the second round. The content validity analysis by the expert panel was completed from March to May 2017. After the 2 rounds, the survey comprised 11 items (3rd version). Fig. 1 summarises the results of the Delphi rounds on content validity (Fig. 1).
Qualitative and quantitative pilot testsIn order to determine the apparent validity of the survey, its feasibility and understanding, during the first fortnight of May a qualitative pilot test was performed in the Intensive Medicine department of a tertiary level hospital with 10 ICU nurses who voluntarily agreed to participate, through non-probabilistic and convenience sampling. The PI discussed their opinions with each nurse in a cognitive pre-test session. No changes were made to the survey. Later, during June 2017 a quantitative pilot test was performed in 4 critical care units (2 general polyvalent units and 2 resuscitation units) of 2 tertiary level hospitals. One hundred and one participants were included through non-probabilistic and convenience sampling to assess the stability of responses by test–retest. Stability was calculated from the intraclass correlation coefficient (ICC); an ICC value of >.70 was considered acceptable. For this test, each survey delivered had a code number to enable re-identification of the person in the retest. The participants had 3 weeks to respond to the test. The retest was performed 15 days after the first administration, which was correctly completed by 68 participants. The survey obtained a test-retest stability of ICC=.71. (95%CI: .57–.81). The final instrument comprised 8 items, since 3 items that had no variability were removed.
Final knowledge-instrument surveyThis comprised 8 items that explored the knowledge of nurses on the reasons (2 items), adverse events (2 items), legal and ethical aspects (3 items), and nursing care (one item) for patients with PR in ICU. The items were rated with 3 response options “true/false/I don’t know”. The correct responses were assessed with 1, and the incorrect responses or lack of response with 0. The scores ranged from 0 to 8.
Data collectionDuring the months of August and September 2017, a collaborating investigator in each centre was contacted by email or telephone to present the project to them and invite them to participate. These people acted as contacts between the PI, the critical care unit managers and the Nursing Management of each hospital, and performed the formalities to request the favourable opinion of the Ethics and Research Committee (ERC), if considered necessary. Once approval had been obtained, these investigators distributed the knowledge survey among the nurses taking part. The questionnaires were submitted and collected in a sealed envelope to ensure the anonymity of the responses. Once completed, the questionnaires were returned to the same person or a department manager. The data was collected over one month, from October to November 2017. The contact people returned the questionnaires again to the PI, who entered them onto the database. For each study unit the contact person completed the CRF for the structural and clinical data.
Data analysisThe analysis of normal distributions and contrasts was performed using quantile plots, histograms and density functions.32 A descriptive analysis was performed of each item. The qualitative variables were described in absolute frequencies and percentages. All the quantitative variables followed a normal distribution, and therefore were described with the mean plus standard deviation (SD). A bivariate analysis was undertaken to assess the relationship between the survey items with the nurses’ sociodemographic and professional variables, and with the structural and clinical data of each unit. The mean scores on knowledge were compared between the 2 groups using the Student's t-test. In the case of groups of 3 or more categories, the analysis of variance (ANOVA) was used. For the means that achieved statistically significant differences, the Cohen's d or f effect size was calculated, depending on the number of categories in the groups. A 95% confidence level (p<.05) was established for all the hypothesis contrasts. SPSS version 24.0 (IBM-SPSS Statistics) was used.
Ethical considerationsThe project was approved by the ERC of 4 of the hospitals involved in the study (PR183/15). The rest of the hospitals considered that it was not necessary to request approval from their ERC since the project had already been approved by other centres. It was considered that responding to the survey implied that consent had been given. The confidentiality of the responses was ensured according to Organic Law 15/99 on the Protection of Personal Data. Participation was voluntary and anonymous. The manuscript conforms to the criteria of the STROBE guidelines on reporting observational studies.
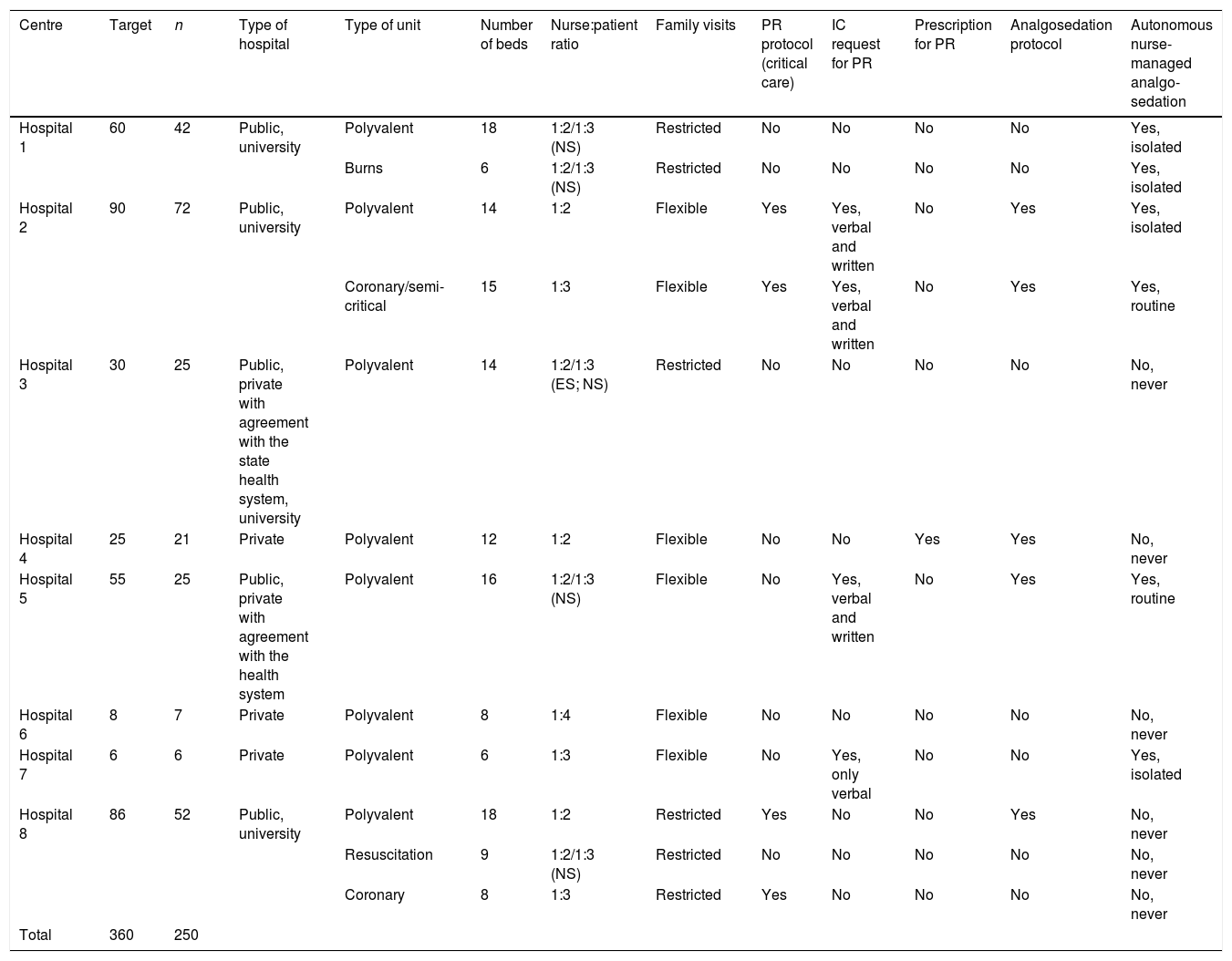
ResultsA total of 354 surveys were distributed, and 254 were collected, 4 of which were blank, therefore 250 were eventually analysed (response rate of 70.62%). The characteristics of the hospitals and the distribution of the participants per hospital are shown in Table 1. In 9 of the 12 units the decision to use and remove PR was made by nurses autonomously without consulting the rest of the team, and in 3 units the use of PR was not recorded in any document.
Characteristics of the centres and distribution of participants.
| Centre | Target | n | Type of hospital | Type of unit | Number of beds | Nurse:patient ratio | Family visits | PR protocol (critical care) | IC request for PR | Prescription for PR | Analgosedation protocol | Autonomous nurse-managed analgo-sedation |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hospital 1 | 60 | 42 | Public, university | Polyvalent | 18 | 1:2/1:3 (NS) | Restricted | No | No | No | No | Yes, isolated |
| Burns | 6 | 1:2/1:3 (NS) | Restricted | No | No | No | No | Yes, isolated | ||||
| Hospital 2 | 90 | 72 | Public, university | Polyvalent | 14 | 1:2 | Flexible | Yes | Yes, verbal and written | No | Yes | Yes, isolated |
| Coronary/semi-critical | 15 | 1:3 | Flexible | Yes | Yes, verbal and written | No | Yes | Yes, routine | ||||
| Hospital 3 | 30 | 25 | Public, private with agreement with the state health system, university | Polyvalent | 14 | 1:2/1:3 (ES; NS) | Restricted | No | No | No | No | No, never |
| Hospital 4 | 25 | 21 | Private | Polyvalent | 12 | 1:2 | Flexible | No | No | Yes | Yes | No, never |
| Hospital 5 | 55 | 25 | Public, private with agreement with the health system | Polyvalent | 16 | 1:2/1:3 (NS) | Flexible | No | Yes, verbal and written | No | Yes | Yes, routine |
| Hospital 6 | 8 | 7 | Private | Polyvalent | 8 | 1:4 | Flexible | No | No | No | No | No, never |
| Hospital 7 | 6 | 6 | Private | Polyvalent | 6 | 1:3 | Flexible | No | Yes, only verbal | No | No | Yes, isolated |
| Hospital 8 | 86 | 52 | Public, university | Polyvalent | 18 | 1:2 | Restricted | Yes | No | No | Yes | No, never |
| Resuscitation | 9 | 1:2/1:3 (NS) | Restricted | No | No | No | No | No, never | ||||
| Coronary | 8 | 1:3 | Restricted | Yes | No | No | No | No, never | ||||
| Total | 360 | 250 |
IC: informed consent; PR: physical restraint; NS: night shift; ES: evening shift.
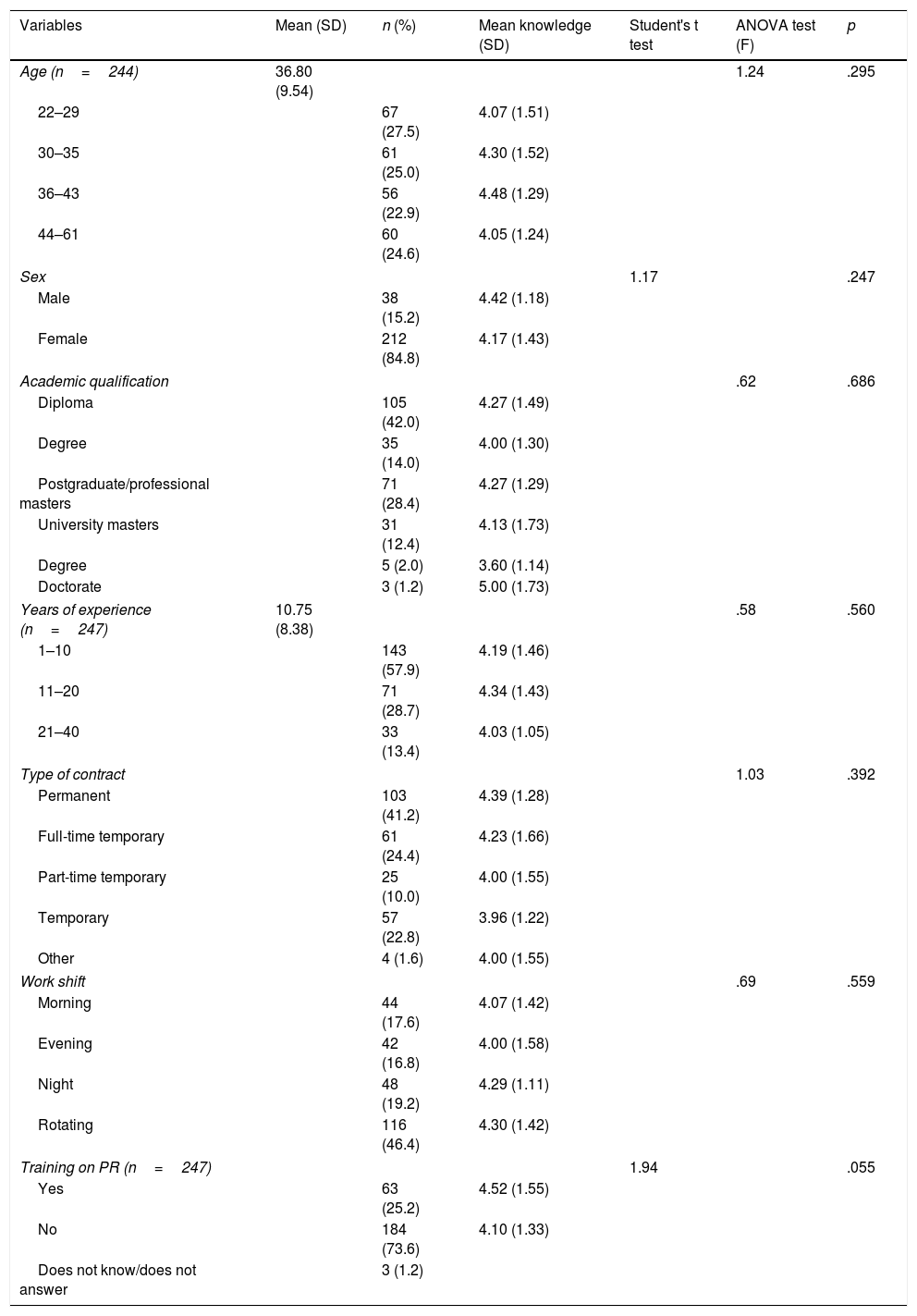
The mean age of the participants was 36.80 (SD 9.54) years, with a mean of 10.75 (SD 8.38) years of professional experience in critical care. Eighty-four point eight percent (n=212) were female. In addition to care, 14.4% (n=36) taught at university, 10.8% (n=27) combined care with research, and 1.2% (n=3) undertook management functions. Seventy-three point six percent of the participants had received no previous training on PR. Table 2 shows the sociodemographic profile of the participants and the relationship of these variables with level of knowledge (Table 2).
Sociodemographic profile and level of knowledge.
| Variables | Mean (SD) | n (%) | Mean knowledge (SD) | Student's t test | ANOVA test (F) | p |
|---|---|---|---|---|---|---|
| Age (n=244) | 36.80 (9.54) | 1.24 | .295 | |||
| 22–29 | 67 (27.5) | 4.07 (1.51) | ||||
| 30–35 | 61 (25.0) | 4.30 (1.52) | ||||
| 36–43 | 56 (22.9) | 4.48 (1.29) | ||||
| 44–61 | 60 (24.6) | 4.05 (1.24) | ||||
| Sex | 1.17 | .247 | ||||
| Male | 38 (15.2) | 4.42 (1.18) | ||||
| Female | 212 (84.8) | 4.17 (1.43) | ||||
| Academic qualification | .62 | .686 | ||||
| Diploma | 105 (42.0) | 4.27 (1.49) | ||||
| Degree | 35 (14.0) | 4.00 (1.30) | ||||
| Postgraduate/professional masters | 71 (28.4) | 4.27 (1.29) | ||||
| University masters | 31 (12.4) | 4.13 (1.73) | ||||
| Degree | 5 (2.0) | 3.60 (1.14) | ||||
| Doctorate | 3 (1.2) | 5.00 (1.73) | ||||
| Years of experience (n=247) | 10.75 (8.38) | .58 | .560 | |||
| 1–10 | 143 (57.9) | 4.19 (1.46) | ||||
| 11–20 | 71 (28.7) | 4.34 (1.43) | ||||
| 21–40 | 33 (13.4) | 4.03 (1.05) | ||||
| Type of contract | 1.03 | .392 | ||||
| Permanent | 103 (41.2) | 4.39 (1.28) | ||||
| Full-time temporary | 61 (24.4) | 4.23 (1.66) | ||||
| Part-time temporary | 25 (10.0) | 4.00 (1.55) | ||||
| Temporary | 57 (22.8) | 3.96 (1.22) | ||||
| Other | 4 (1.6) | 4.00 (1.55) | ||||
| Work shift | .69 | .559 | ||||
| Morning | 44 (17.6) | 4.07 (1.42) | ||||
| Evening | 42 (16.8) | 4.00 (1.58) | ||||
| Night | 48 (19.2) | 4.29 (1.11) | ||||
| Rotating | 116 (46.4) | 4.30 (1.42) | ||||
| Training on PR (n=247) | 1.94 | .055 | ||||
| Yes | 63 (25.2) | 4.52 (1.55) | ||||
| No | 184 (73.6) | 4.10 (1.33) | ||||
| Does not know/does not answer | 3 (1.2) | |||||
ANOVA: analysis of variance; PR: physical restraint; SD: standard deviation.
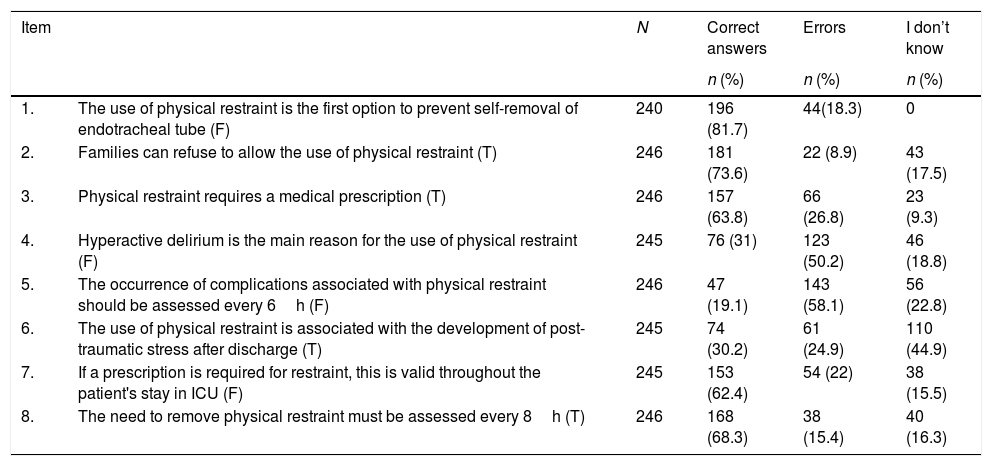
In relation to the results of the knowledge survey, the overall mean was 4.21 (SD 1.39) (range 0–8). The item with the most correct responses referred to the use of PR as a first option to prevent self-removal of the endotracheal tube. More than 50% of the respondents confirmed erroneously that hyperactive delirium was the main reason for using PR; and only 19.1% responded correctly to the statement on the frequency of monitoring on the occurrence of complications associated with its use. The descriptions of correct and erroneous answers per item are shown in Table 3.
Results of the knowledge survey.
| Item | N | Correct answers | Errors | I don’t know | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| 1. | The use of physical restraint is the first option to prevent self-removal of endotracheal tube (F) | 240 | 196 (81.7) | 44(18.3) | 0 |
| 2. | Families can refuse to allow the use of physical restraint (T) | 246 | 181 (73.6) | 22 (8.9) | 43 (17.5) |
| 3. | Physical restraint requires a medical prescription (T) | 246 | 157 (63.8) | 66 (26.8) | 23 (9.3) |
| 4. | Hyperactive delirium is the main reason for the use of physical restraint (F) | 245 | 76 (31) | 123 (50.2) | 46 (18.8) |
| 5. | The occurrence of complications associated with physical restraint should be assessed every 6h (F) | 246 | 47 (19.1) | 143 (58.1) | 56 (22.8) |
| 6. | The use of physical restraint is associated with the development of post-traumatic stress after discharge (T) | 245 | 74 (30.2) | 61 (24.9) | 110 (44.9) |
| 7. | If a prescription is required for restraint, this is valid throughout the patient's stay in ICU (F) | 245 | 153 (62.4) | 54 (22) | 38 (15.5) |
| 8. | The need to remove physical restraint must be assessed every 8h (T) | 246 | 168 (68.3) | 38 (15.4) | 40 (16.3) |
F: false; T: true.
In the analysis per item, the respondents who had received prior training on PR had more knowledge regarding the statements referring to legislation and ethical aspects than the nurses with no prior training (item 2: χ2=12.34 [p=.055], Cramer's V=.16; item 3: χ2=14.50 [p=.025], Cramer's V=.17).
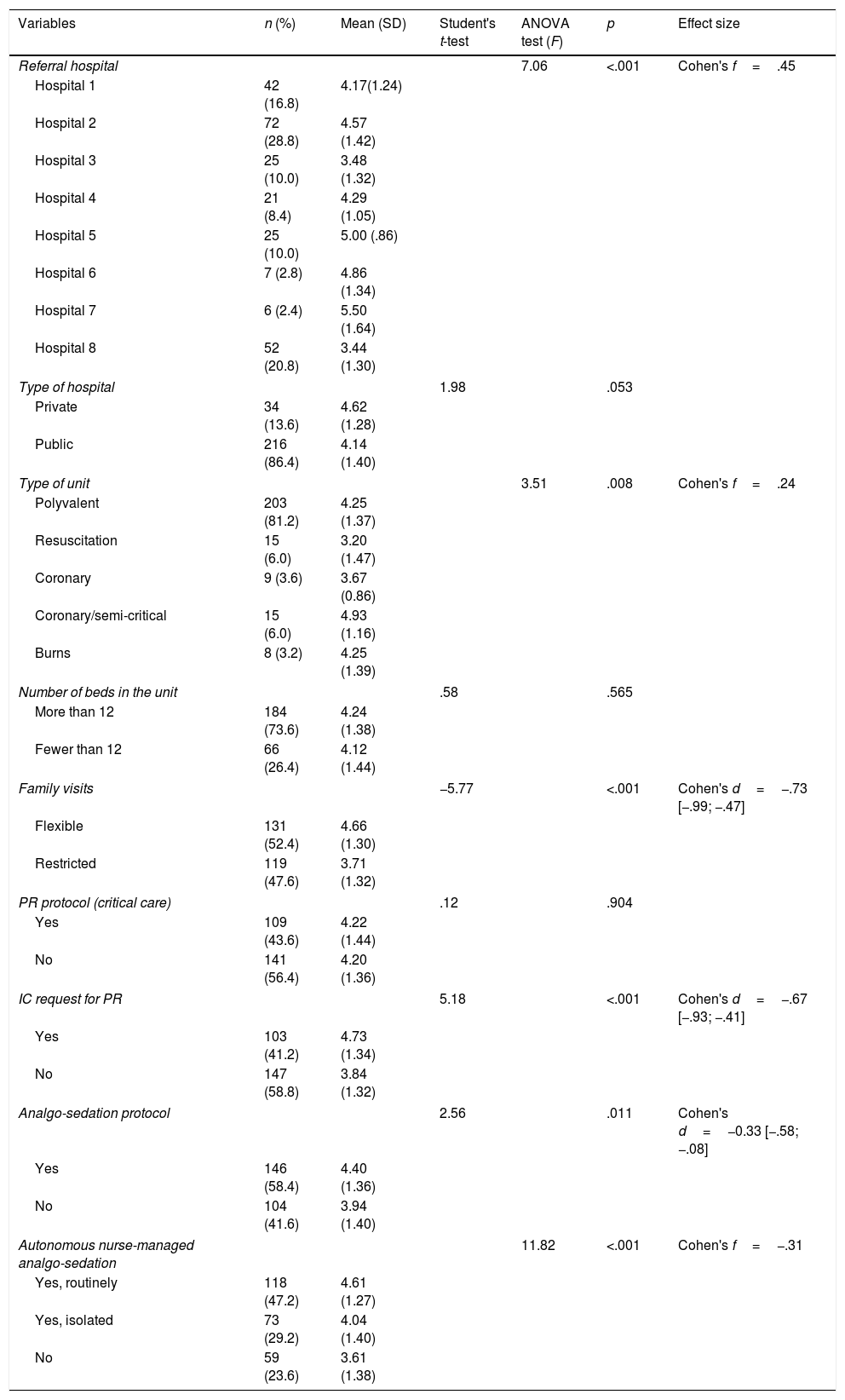
With regard to the relationship with the structural and clinical variables of the units, the level of knowledge was significantly associated with the referral hospital (F=7.06; p<.001; Cohen's f=.45), and the type of unit (F=3.51; p=.008; Cohen's f=.24). Similarly, it is more likely that nurses with a higher level of knowledge will work in units were informed consent is required for PR (p<.001, Cohen's d=−.67 [−.93; −.41]); flexible family visits (p<.001, Cohen's d=−.73 [−.99; −.47]), and that have a multidisciplinary analgo-sedation protocol (p=.011, Cohen's d=−.33 [−.58; −.08]), or that the nurse will have autonomy in managing analgo-sedation (F=11.82; p<.001; Cohen's f=.31) (Table 4). None of the sociodemographic or individual professional data was associated with level of knowledge (Table 2).
Structural and clinical characteristics associated with level of knowledge.
| Variables | n (%) | Mean (SD) | Student's t-test | ANOVA test (F) | p | Effect size |
|---|---|---|---|---|---|---|
| Referral hospital | 7.06 | <.001 | Cohen's f=.45 | |||
| Hospital 1 | 42 (16.8) | 4.17(1.24) | ||||
| Hospital 2 | 72 (28.8) | 4.57 (1.42) | ||||
| Hospital 3 | 25 (10.0) | 3.48 (1.32) | ||||
| Hospital 4 | 21 (8.4) | 4.29 (1.05) | ||||
| Hospital 5 | 25 (10.0) | 5.00 (.86) | ||||
| Hospital 6 | 7 (2.8) | 4.86 (1.34) | ||||
| Hospital 7 | 6 (2.4) | 5.50 (1.64) | ||||
| Hospital 8 | 52 (20.8) | 3.44 (1.30) | ||||
| Type of hospital | 1.98 | .053 | ||||
| Private | 34 (13.6) | 4.62 (1.28) | ||||
| Public | 216 (86.4) | 4.14 (1.40) | ||||
| Type of unit | 3.51 | .008 | Cohen's f=.24 | |||
| Polyvalent | 203 (81.2) | 4.25 (1.37) | ||||
| Resuscitation | 15 (6.0) | 3.20 (1.47) | ||||
| Coronary | 9 (3.6) | 3.67 (0.86) | ||||
| Coronary/semi-critical | 15 (6.0) | 4.93 (1.16) | ||||
| Burns | 8 (3.2) | 4.25 (1.39) | ||||
| Number of beds in the unit | .58 | .565 | ||||
| More than 12 | 184 (73.6) | 4.24 (1.38) | ||||
| Fewer than 12 | 66 (26.4) | 4.12 (1.44) | ||||
| Family visits | −5.77 | <.001 | Cohen's d=−.73 [−.99; −.47] | |||
| Flexible | 131 (52.4) | 4.66 (1.30) | ||||
| Restricted | 119 (47.6) | 3.71 (1.32) | ||||
| PR protocol (critical care) | .12 | .904 | ||||
| Yes | 109 (43.6) | 4.22 (1.44) | ||||
| No | 141 (56.4) | 4.20 (1.36) | ||||
| IC request for PR | 5.18 | <.001 | Cohen's d=−.67 [−.93; −.41] | |||
| Yes | 103 (41.2) | 4.73 (1.34) | ||||
| No | 147 (58.8) | 3.84 (1.32) | ||||
| Analgo-sedation protocol | 2.56 | .011 | Cohen's d=−0.33 [−.58; −.08] | |||
| Yes | 146 (58.4) | 4.40 (1.36) | ||||
| No | 104 (41.6) | 3.94 (1.40) | ||||
| Autonomous nurse-managed analgo-sedation | 11.82 | <.001 | Cohen's f=−.31 | |||
| Yes, routinely | 118 (47.2) | 4.61 (1.27) | ||||
| Yes, isolated | 73 (29.2) | 4.04 (1.40) | ||||
| No | 59 (23.6) | 3.61 (1.38) | ||||
ANOVA: analysis of variance; IC: informed consent; PR: physical restraint; SD: standard deviation.
The results of this paper show that nurses have moderate knowledge overall, which coincides with the results reported by other authors in different contexts to ours and with other measurement instruments.16,18,19,23
Among the reasons for using PR it was noteworthy that 18.3% of nurses still consider the use of PR as a first option to prevent self-removal of the endotracheal tube, an assertion that directly contradicts the international guidelines that recommend the exhaustion of all verbal, environmental and pharmacological alternatives, reserving the use of PR as the last possible option.10,11 Secondly, more than half the respondents erroneously considered that hyperactive delirium is the main reason for using PR. Various authors have reported that the main reason for the use of PR is agitation, which is associated with a greater risk of self-removal of devices. Luk et al.4 report that 43% of patients with PR were restrained due to agitation, and 7% due to delirium. In our country, Martín Iglesias et al.13 identified that 63.5% of patients had psychomotor agitation at the time that PR was started. In line with Freeman et al.,2 in our opinion, this result conveys confusion between the terms agitation and delirium, which are often used indistinctly in the literature. It is true that hyperactive delirium is coincident with psychomotor agitation, but there are other subtypes of delirium where there is no agitation, and furthermore, in critical care units, agitation can be due to many reasons other than delirium. Another possible reason for this confusion could be that the onset of delirium has been independently associated with the use of PR.8
In terms of the frequency of monitoring the complications associated with the use of PR, although the international guidelines recommend a minimum of every 4h, or every 2h if the patient is agitated, more than half the nurses would monitor every 6h. This result coincides with other papers where more than a third of nurses self-report assessing the use of PR every 8h30,33 or when they deem it necessary according to the condition of the patient.34 In the study by Suliman et al.,19 only 17.3% self-report checking the site of restraint every 2h; and 22%, inspecting the skin of the patient with PR.
With regard to the prescription of the intervention, although more than 60% of the respondents answered correctly to the requirement for a prescription and the need to re-assess it, this data contrasts with the fact that in only one private centre, of the 8 included in the study, was PR used under a medical prescription. Acevedo-Nuevo et al.28 already highlighted that the preferred opinion among critical care nurses is that PR measures should be prescribed by nurses, because of their position in risk assessment and the bedside management of patients. De Jonghe et al.,35 in an observational study in 121 French ICU, published that for more than 50% of the patients in 68% of French ICU, PR is started and removed without a medical prescription, and that only 21% of the units have regulations and prescription sheets for the use of PR. Along similar lines, Langley et al.36 describe the communication problems between doctors and nurses regarding this practice, and the reluctance of doctors to prescribe it, considering it unnecessary or a minor decision that does not require their attention, which is evidenced by their lack of knowledge as to whether or not physical restraint is being used on patients.14 In our country, the recommendations on the prescription of PR in hospital have been imported from the legislation on the subject directed at the social services or patients with mental health disorders. However, the reasons for, management and duration of restraining measures in hospitals are very different to those areas, which should be reviewed, legislated and adapted according to real conditions. Due to the ethical considerations engendered by this intervention, the decision to restrain a patient in hospitals should never be taken by a single person; the decision should be taken by the team.
The results of analysing the factors influencing nurses’ knowledge indicated that their working environment affected their knowledge levels, since these were significantly associated with the referral hospital, type of unit, request for informed consent, and the rules of the ICU regarding family visits and analgo-sedation, rather than the nurses’ individual characteristics. It is striking that previous training received on the subject was not significant regarding the level of knowledge, as reported by other authors,16,19 although a trend seems to be emerging. It is noteworthy that all these characteristics convey greater awareness in hospitals to seek alternatives to restraint, and more systematic and individualised management of analgo-sedation.28 It would be appropriate, therefore, to investigate whether knowledge is also acquired through imitating models of behaviour and day-to-day experience in an environment with a specific culture. In this regard, the involvement of hospitals in applying programmes with more than one component that include training of professionals, the creation of multidisciplinary consultation groups, and the daily monitoring of patients with PR have proven effective in significantly reducing the use of PR in ICU,37–39 which should remind organisations of their responsibility in this area.
This study has certain limitations. Firstly, it is a survey and not a questionnaire. Nevertheless, it provides data on the stability and validity of content of the items, which gives greater robustness to the statements made. Secondly, the hospitals were selected by convenience, which might limit extrapolation of the results to the rest of the country. Likewise, the nurses agreed to participate voluntarily. However it does provide us with a first approach to the state of play. Thirdly, the relationship between knowledge and actual practice was not established, therefore we do not know whether a greater level of knowledge is associated with less use of PR in the hospitals analysed. However, the knowledge of the nurses on PR was associated with self-reported practices regarding this intervention,16 and providing educational sessions on the subject was shown to be effective in improving knowledge.21,22 The results and the fact that more than 70% of the nurses surveyed had received no training on physical restraint suggest the need for training sessions on this subject in the centres analysed.
ConclusionsNurses in critical care units have moderate knowledge about PR, therefore more training and awareness-raising on the subject is required. The individual sociodemographic and professional characteristics have little influence on level of knowledge. The working environment where care is delivered, the rules on family visits, requesting informed consent for PR, and the analgo-sedation policy and sedation management by nurses greatly influence the level of knowledge of this intervention. Correlating the level of knowledge and practice would be a proposal for future studies. Likewise, the results help to identify structural and clinical factors that are associated with a higher level of knowledge. Therefore the organisations should act on these results to improve the training of their professionals.
FinancingThis study was financed by the Official College of Nursing of Barcelona (COIB) within the framework of Grants for Research Projects (PR-2080/15).
Conflict of interestsThe authors have no conflict of interests to declare.
We would like to acknowledge the collaboration of all the nurses who voluntarily agreed to participate in the study, and Judith Peñafiel for her advice and statistical support.
Hospital Universitari Joan XXIII, Tarragona:
Laura Claramunt-Domènech, Diana Gil-Castillejos
Hospital Universitario de Getafe, Getafe, Madrid:
María del Mar Sánchez-Sánchez, Susana Arias-Rivera
Hospital Universitario Doctor Josep Trueta, Girona:
Aaron Castanera-Duro, Anna Lobo-Cívico, Andrea García-Lamigueiro
Consorci Sanitari del Maresme, Hospital de Mataró, Mataró, Barcelona:
Ester Aguirre-Recio, Aina Ros Nebot, Immaculada Amenós-Alcaraz
Corporació Sanitària Parc Taulí, Sabadell, Barcelona:
Miriam Secanella-Martínez, Rosa Jam-Gatell
Hospital Mutua Terrassa, Terrassa, Barcelona
Immaculada Sandalinas-Mulero
Hospital Quironsalud, Málaga, Málaga:
Álvaro Ortega-Guerrero
Hospital San Juan de Dios de Córdoba, Córdoba
Francisca Yuste-Bustos
Please cite this article as: Via-Clavero G, Claramunt-Domènech L, García-Lamigueiro A, Sánchez-Sánchez MM, Secanella-Martínez M, Aguirre-Recio E, et al. Análisis de una encuesta sobre conocimientos en contenciones mecánicas de las enfermeras de unidades de críticos. Enferm Intensiva. 2019;30:47–58.
First prize for the best oral communication presented at the XLIV Congreso Nacional de la Sociedad Española de Enfermería Intensiva y Unidades Coronarias (44th National Congress of the Spanish Society of Intensive Nursing and Coronary Units), held in Granada from 10 to 13 June 2018.