To assess surgical management and postoperative results associated with early extubation in patients undergoing tetralogy of Fallot corrective surgery at a public hospital in Argentina.
MethodsA retrospective review was made from clinical records from patients who underwent corrective surgery for tetralogy of Fallot. A total of 38 clinical records that met the inclusion criteria for the retrospective review were included in the analysis.
Results16% were extubated early. Milrinone was the only drug that showed differences in patients who were extubated early (p=0.01). Extracorporeal circulation time, aortic clamping time, transfusion with cryoprecipitates, saturation of oxygen pressure, and haematocrit at the end of the surgical procedure showed no differences (p>.05). In the postoperative period, the ICU stay was shorter for the patients who were extubated early (p=0.0007), but there were no differences in the total hospital stay (p=0.26).
ConclusionsEarly extubation in the institution, although found to be low frequency, has proved as a safe and effective alternative to shorten these patients’ stay in ICU.
Analizar el manejo intraquirúrgico y los resultados posquirúrgicos asociados a la extubación temprana en los pacientes sometidos a cirugía reparadora de tetralogía de Fallot en un hospital público argentino.
MétodosSe realizó una revisión retrospectiva de los expedientes clínicos de los pacientes a quienes se les practicó cirugía para corrección de tetralogía de Fallot. Se incluyeron en el análisis un total de 38 expedientes que cumplieron con los criterios de inclusión establecidos en el protocolo para la revisión retrospectiva.
ResultadosEl 16% fue extubado de manera temprana. Milrinona fue la única droga que mostró diferencias en los pacientes a quienes se extubó de manera temprana (p=0,01). El tiempo de circulación extracorpórea, el de clampaje aórtico, la transfusión con crioprecipitados, la saturación de la presión de oxígeno, y el hematocrito al finalizar el procedimiento quirúrgico no evidenciaron diferencias (p>0,05). En el período posquirúrgico, la estadía en UTI fue más corta en los pacientes que fueron extubados de manera temprana (p=0,0007), pero no hubo diferencias en la estadía hospitalaria total (p=0,26).
ConclusionesLa extubación temprana en la institución si bien resultó de baja frecuencia ha demostrado ser una alternativa segura y eficaz para disminuir la estancia en UTI de estos pacientes.
Several studies confirm the safely and efficacy of early extubation in patients with paediatric cardiovascular surgery. Compared with standard strategies, this increases the patient's well-being, reduces hospital stay and lowers complications.
Early extubation is a safe and effective means of lowering the patient's stay in the ICU following corrective tetralogy of Fallot surgery, although not all patients are eligible for this practice.
What are the study implications?This study has clinical implications for management of the surgical team in patients with tetralogy of Fallot. It also has implications for clinical management of patients’ stay in the ICU and hospital resources.
Early extubation in adult patients who have undergone surgical procedures to resolve heart conditions has been demonstrated to be safe and also to lower hospital costs.1 After several years, multiple studies provided sufficient evidence for these procedures to be applied to paediatric patients in corrective congenital heart surgery. Despite this, up until several years ago some controversy existed regarding this practice in the paediatric population2; however, at present there is a considerably large volume of studies which demonstrates that early extubation may be applied safely in cases of intermediate to high surgical complexity, even in newborns.3–14
The term “early extubation” is a concept which is included within the “fast-track approach” and is used to define the removal of the endotrachial tube in patients within 6–8h after termination of surgery.12 Early extubation pursues the aim of achieving early mobilisation with its consequent reduction in Intensive Care Unit (ICU) stay and therefore earlier hospital discharge.
Although early extubation has been applied routinely for adult patients there are still fairly polarised opinions regarding its application in children and more so in cases of corrective surgery for congenital cardiopathies including that of tetralogy of Fallot.15 So, what are the advances to be gained from early extubation in the paediatric population which would lead to greater safety? Historically, it was always necessary to extubate paediatric age patients as early as possible, due to the fact that in past decade sedation techniques and the development of mechanical ventilation technologies were not optimal for these patients.
High dose opiate techniques subsequently became more popular and were more frequently used to provide greater haemodynamic stability to reduce stress in post-surgical response and in cardiopulmonary bypass. Advances in paediatric cardiovascular surgery have been able to improve surgical techniques, satisfactorily manage cardiopulmonary bypass and introduce short-action sedatives which in turn leads to obtaining the same result without having to resort to prolonged mechanical ventilation.15 As a result, when the aim is to reduce mechanical ventilation time, some authors confirm that controversies have been resolved,7,16–21 since hospital stay and the risk of complications have been lowered.
The purposes of early extubation are to prevent: (a) accidental extubations in the ICU; (b) laryngotrachial trauma; (c) the accumulation of mucus in the endotrachial tube; (d) pulmonary hypertensive crises; (e) complications associated with mechanical ventilation such as barotrauma, atelectases or infections. Furthermore, patients who require mechanical ventilation often require sedation and some type of haemodynamic support.17,18,22,23 It may also be added that patients who are extubated early may be more quickly mobilised and re-initiate oral feeding so that intestinal function may be more quickly recuperated. For some authors the question continues to be whether they should apply early extubation to this patient in the same manner as any other patient.
We should note that there are authors with a more conservative focus based on patient safety, who argue that none of the benefits suggested in the preceding paragraph would overcome the significant risks associated with early extubation.7,12,13,16,20,24–28 They admit that extubation per se has no risks, but that the latter arise from poor patient selection as candidates for this procedure, and suggest this requires lowering.20
Among the most common adverse events are reintubation and hospital readmission due to acute complications, but the benefits are considered superior by some authors,7,11,29–35 since it has been estimated that between 1%26 and 3%37–39 of early extubated patients will require a reinturbation.
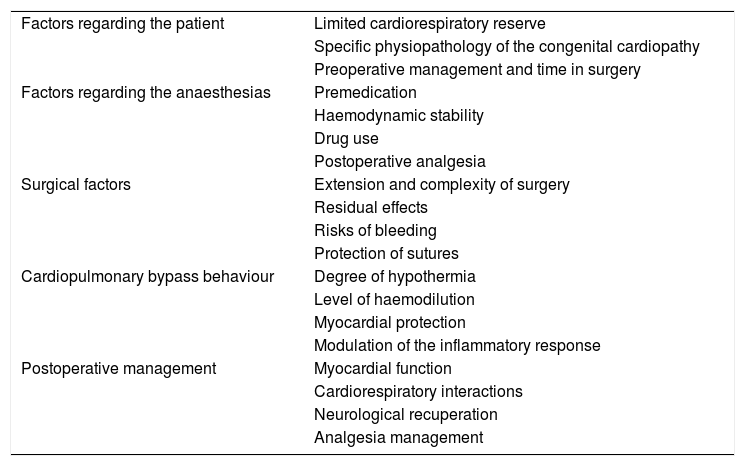
Among the factors which impact in the decision for early extubation of a patient are those contained in table one39 (Table 1).
Factors impacting the decision for early extubation after paediatric heart surgery.
| Factors regarding the patient | Limited cardiorespiratory reserve |
| Specific physiopathology of the congenital cardiopathy | |
| Preoperative management and time in surgery | |
| Factors regarding the anaesthesias | Premedication |
| Haemodynamic stability | |
| Drug use | |
| Postoperative analgesia | |
| Surgical factors | Extension and complexity of surgery |
| Residual effects | |
| Risks of bleeding | |
| Protection of sutures | |
| Cardiopulmonary bypass behaviour | Degree of hypothermia |
| Level of haemodilution | |
| Myocardial protection | |
| Modulation of the inflammatory response | |
| Postoperative management | Myocardial function |
| Cardiorespiratory interactions | |
| Neurological recuperation | |
| Analgesia management |
The purpose of this study was to determine the intra and post operative characteristics of patients who have undergone repair surgery for tetralogy of Fallot, with and without early extubation, in the Prof. Dr. Juan P. Garrahan Centro Quirúrgico del Hospital de Pediatría S.A.M.I.C. in Argentina, during the months of January 2016 and July 2017.
MethodsA descriptive level study was conducted, through a retrospective review of medical patient files, of patients who underwent surgery for corrective tetralogy of Fallot, to assess the characteristics of the intra-and-postoperative management in patients with and without early extubation.
The study was conducted in the Prof. Dr. Juan P. Garrahan Hospital de Pediatría S.A.M.I.C. This is a public hospital of high complexity located in the Autonomous City of Buenos Aires, undertaking the care of newborns, children and teenagers. It is a national referral hospital for the diagnosis and treatment of the most complex paediatric pathologies. In accordance with statistic published by this institution, in the year 2015, 9671 operations were scheduled and approximately 17,630 anaesthesias.40
During the period under study 819 corrective congenital cardiopathies were performed in the surgical unit of the hospital. These included 38 tratralogies of Fallot, which were subject to the following inclusion criteria:
- -
Ages from 0 months to 10 years.
- -
Patients programmed for elective corrective tetralogy of Fallot surgery who were admitted to the surgical unit of the hospital during the period between January 2016 and July 2017.
The following cases of patient who had presented were excluded:
- •
Predictors and/or background of complicated ventilation and/or intubation.
- •
Neurological disorders.
- •
Swallowing disorders.
- •
Ventilatory assistance requirement for extracardioivascular reasons.
- •
Hospital admittance for reoperation due to bleeding.
- •
Patients who had been admitted for insertion of a pacemaker.
- •
Previous hospital admission for surgery, pericardial or pleural effusions.
- •
Data were collected in an ad hoc template specifically designed for this end, which contained the patient information required. All the records were coded ensuring patient identity anonymity.
- •
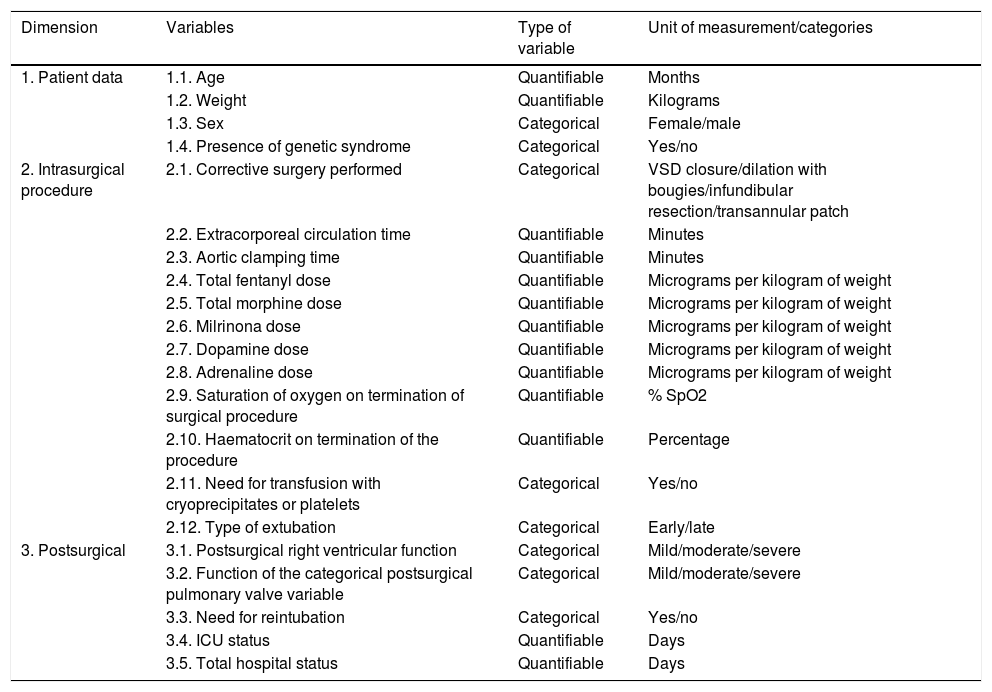
The dimensions and variables studied were those contained in Table 2.
Table 2.Operational function of study variables.
Dimension Variables Type of variable Unit of measurement/categories 1. Patient data 1.1. Age Quantifiable Months 1.2. Weight Quantifiable Kilograms 1.3. Sex Categorical Female/male 1.4. Presence of genetic syndrome Categorical Yes/no 2. Intrasurgical procedure 2.1. Corrective surgery performed Categorical VSD closure/dilation with bougies/infundibular resection/transannular patch 2.2. Extracorporeal circulation time Quantifiable Minutes 2.3. Aortic clamping time Quantifiable Minutes 2.4. Total fentanyl dose Quantifiable Micrograms per kilogram of weight 2.5. Total morphine dose Quantifiable Micrograms per kilogram of weight 2.6. Milrinona dose Quantifiable Micrograms per kilogram of weight 2.7. Dopamine dose Quantifiable Micrograms per kilogram of weight 2.8. Adrenaline dose Quantifiable Micrograms per kilogram of weight 2.9. Saturation of oxygen on termination of surgical procedure Quantifiable % SpO2 2.10. Haematocrit on termination of the procedure Quantifiable Percentage 2.11. Need for transfusion with cryoprecipitates or platelets Categorical Yes/no 2.12. Type of extubation Categorical Early/late 3. Postsurgical 3.1. Postsurgical right ventricular function Categorical Mild/moderate/severe 3.2. Function of the categorical postsurgical pulmonary valve variable Categorical Mild/moderate/severe 3.3. Need for reintubation Categorical Yes/no 3.4. ICU status Quantifiable Days 3.5. Total hospital status Quantifiable Days
The type of surgical correction made was divided according to the Akhtar11 criteria: VSD closure, dilation with bougies, infundibular resection and transannular patch transannular.
To characterise the type of extubation made with the patients the Friesen criteria was considered.41 Thus, early extubation was classified as all procedures which had occurred within 6h after the patient left the operating theatre. In contrast, delayed extubation was considered to be those which occurred later than 6h after the patient left the operating theatre.
Postsurgical functions of the right ventricle and the pulmonary valve were assessed by transoesophageal echocardiogram and three categories were considered: mild, moderate and severe, according to Friesen.41
For its part, the need for postsurgical endotracheal reintubation was assessed by following the Baisch criteria.16 In this study, the cut-off point was considered to be 24h after the patient left the operating theatre.
Statistical analysis was performed step by step in accordance with the proposed objectives. In accordance with the following detail:
The intrasurgical management characteristics of the patients on whom corrective tetralogy of Fallot surgery was practiced were determined by descriptive statistics with central tendency measures and dispersion for measurable variables and with absolute and percentage frequency for the categorical variables. Differences were also estimated through the Student's t-test for mean differences.
For its part the frequency of patients with early endotrachial extubation was determined with absolute and percentage frequency for measurable variables.
Finally, the duration of stay in the ICU and total hospital stay in patients was determined with central tendency and dispersion statistics for measurable variables and differences between patients with and without early extubation were calculated through the Student's t-test for mean differences.
All analysis was performed using the Info stat professional investment software, working at a significant level of p<−.05.
This study protocol was presented to the Bioethical Committee of the Garrahan Hospital for its evaluation and subsequent approval. All data and results presented complied with patent identity anonymity. Owing to the fact that the study was conducted through a retrospective review of clinical records, there were no risks attached for any patient.
ResultsA total of thirty eight patients were submitted for corrective tetralogy of Fallot surgery in the Prof. Dr. Juan P. Garrahan Centro Quirúrgico del Hospital de Pediatría S.A.M.I.C. during the months of January 2016 and July 2017, and met with the established inclusion criteria for retrospective review.
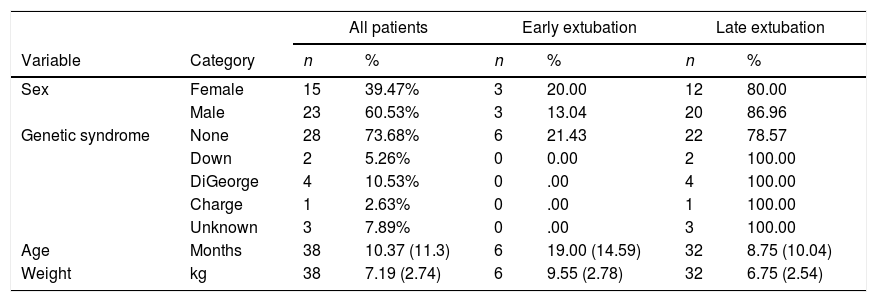
60.5% of the patients were male, aged between 2 and 51 months and weight was between 3.6kg and 15kg. 26.3% of patients had a genetic syndrome, with the DiGeorge syndrome being the most frequent (10.5%) (Table 3).
General characteristics of patients undergoing corrective tetralogy of Fallot surgery.
| All patients | Early extubation | Late extubation | |||||
|---|---|---|---|---|---|---|---|
| Variable | Category | n | % | n | % | n | % |
| Sex | Female | 15 | 39.47% | 3 | 20.00 | 12 | 80.00 |
| Male | 23 | 60.53% | 3 | 13.04 | 20 | 86.96 | |
| Genetic syndrome | None | 28 | 73.68% | 6 | 21.43 | 22 | 78.57 |
| Down | 2 | 5.26% | 0 | 0.00 | 2 | 100.00 | |
| DiGeorge | 4 | 10.53% | 0 | .00 | 4 | 100.00 | |
| Charge | 1 | 2.63% | 0 | .00 | 1 | 100.00 | |
| Unknown | 3 | 7.89% | 0 | .00 | 3 | 100.00 | |
| Age | Months | 38 | 10.37 (11.3) | 6 | 19.00 (14.59) | 32 | 8.75 (10.04) |
| Weight | kg | 38 | 7.19 (2.74) | 6 | 9.55 (2.78) | 32 | 6.75 (2.54) |
Age and weight variables are expressed as a mean (SD).
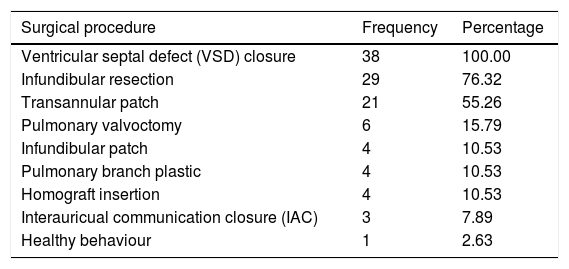
Regarding the intrasurgical period 100% of patients underwent ventricular septal defect (VSD) closure, 76.3% underwent infundibular resection and 55.2% were inserted with a transannular patch. The combination of VSD closure and infundibular resection was the most common combination of procedures performed on the patients during the study period (Table 4).
Frequency of surgical procedures performed on patients submitted to corrective tetralogy of Fallot surgery.
| Surgical procedure | Frequency | Percentage |
|---|---|---|
| Ventricular septal defect (VSD) closure | 38 | 100.00 |
| Infundibular resection | 29 | 76.32 |
| Transannular patch | 21 | 55.26 |
| Pulmonary valvoctomy | 6 | 15.79 |
| Infundibular patch | 4 | 10.53 |
| Pulmonary branch plastic | 4 | 10.53 |
| Homograft insertion | 4 | 10.53 |
| Interauricual communication closure (IAC) | 3 | 7.89 |
| Healthy behaviour | 1 | 2.63 |
With regard to the extubation management of patients after surgery 16% (n=6) were extubated on average 5.33 (SD 2.3) h after surgery, whilst the remaining 84.2% (n=32) were extubated on average 91.7 (SD 161.5) h after termination of surgery (p=.005). Results will now be presented by comparing the data obtained in both groups of patients.
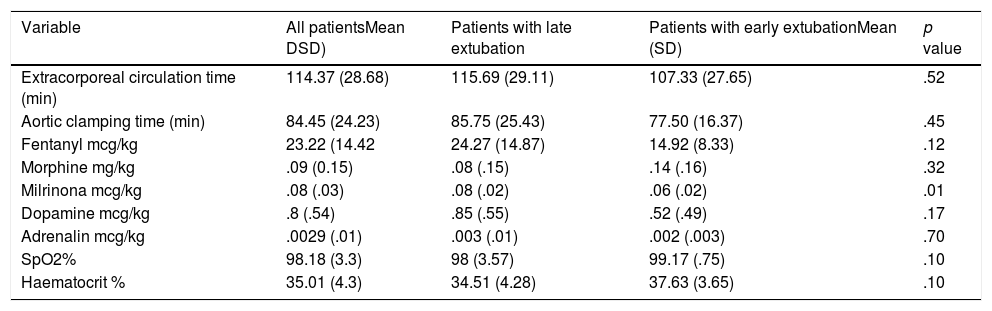
Extracorporeal circulation had a mean of 115.6 (SD 29.1) min in patients with late extubation, whilst this was 107 (SD 27.6) min in patients with early extubation, although no significant differences were found (p=.52). For its part aortic clamping had a mean of 85.7 (SD 25.4) min in the patient group with late extubation and a mean of 77.5 (SD 16.3) min in the early extubation patient group, although differences were not statistically significant either (p=.45) (Table 5).
Means and standard deviations of variables of intrasurgical management in patients who have undergone corrective tetralogy of Fallot surgery.
| Variable | All patientsMean DSD) | Patients with late extubation | Patients with early extubationMean (SD) | p value |
|---|---|---|---|---|
| Extracorporeal circulation time (min) | 114.37 (28.68) | 115.69 (29.11) | 107.33 (27.65) | .52 |
| Aortic clamping time (min) | 84.45 (24.23) | 85.75 (25.43) | 77.50 (16.37) | .45 |
| Fentanyl mcg/kg | 23.22 (14.42 | 24.27 (14.87) | 14.92 (8.33) | .12 |
| Morphine mg/kg | .09 (0.15) | .08 (.15) | .14 (.16) | .32 |
| Milrinona mcg/kg | .08 (.03) | .08 (.02) | .06 (.02) | .01 |
| Dopamine mcg/kg | .8 (.54) | .85 (.55) | .52 (.49) | .17 |
| Adrenalin mcg/kg | .0029 (.01) | .003 (.01) | .002 (.003) | .70 |
| SpO2% | 98.18 (3.3) | 98 (3.57) | 99.17 (.75) | .10 |
| Haematocrit % | 35.01 (4.3) | 34.51 (4.28) | 37.63 (3.65) | .10 |
SD: standard deviation.
Management of anaesthesia drugs during the intrasurgical period is contained in Table 5, with milirone being the only drug with statistically significant differences in patients with early extubation (p=.01). Saturation of oxygen pressure (SpO2) and haematocrit at the end of the surgical procedure showed no statistically significant differences (Table 5).
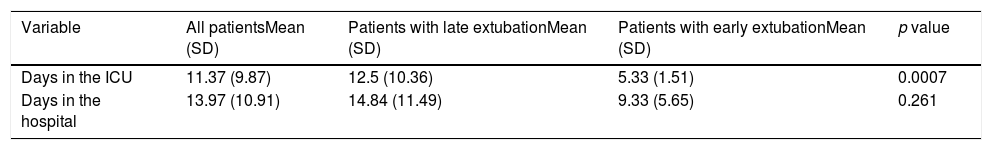
During the postsurgical period, the stay in the ICU was shorter in patients with early extubation (p=.0007), but there were no differences in total hospital stay (p=.26), as may be observed in Table 6.
Means and standard deviations of length of stay in the ICU and total stay in the hospital of patients who underwent corrective tetralogy of Fallot surgery.
| Variable | All patientsMean (SD) | Patients with late extubationMean (SD) | Patients with early extubationMean (SD) | p value |
|---|---|---|---|---|
| Days in the ICU | 11.37 (9.87) | 12.5 (10.36) | 5.33 (1.51) | 0.0007 |
| Days in the hospital | 13.97 (10.91) | 14.84 (11.49) | 9.33 (5.65) | 0.261 |
SD: standard deviation; ICU: intensive care unit.
In the postoperative echocardiogram of the patients with late extubation, 50% showed a moderate to severe dysfunction of the right ventricle, whilst in early extubated patients only 16.6% showed moderate to severe dysfunction (p=0.13). Also, in the same test, 40.6% of patients with late extubation showed moderate to severe pulmonary function impairment, whilst all patients who were extubated early had mild pulmonary function impairment (p=.05).
Finally, none of the patients extubated before 6h after surgery presented with postoperative complications, whilst in patients with late extubation 15.6% presented some type of postsurgical complication (p=.29), with a total of 5 complications observed: two complete atrioventricular blocks, two patients with low cardiac output and one reintervention.
DiscussionSeveral associations were found in this study between the variables referring to the surgical act, postsurgical procedures and early extubation of the patients.
Intrasurgical management patterns included the use of anaesthetic drugs, whilst the frequency of patients with early endotracheal extubation was low (16%). Stay in the ICU was shorter in patients who were extubated prior to 6h after termination of surgery, which was consistent with findings from other studies that were also focused on demonstrating the importance this had on cost-effectiveness.29,36 However, hospital stay did not report any significant differences between the two patient groups. This may be explained by the sample size limitation in this study, as background data suggest the contrary.
In addition to the difference in ICU stay, early extubation in this study was associated with a reduction in complications relating to postoperative pulmonary function, which coincided with other authors who also stated that this led to a reduction in care costs.4,22,41
Friesen41 states that extubation after intracardiac repair in tetralogy of Fallow may be delayed for three main reasons: right ventricular dysfunction, pulmonary regurgitation and postoperative bleeding. Good perioperative management (essentially careful preoperative evaluation, careful management of drugs in the intraoperative period and complete surgical repair) made early extubation in these patients possible. The Friesen41 study demonstrated that there was no association between ventricular function and type of extubation, and early extubation was therefore suggested after heart surgery as a safe alternative to prolonged postoperative intubation, although it has not yet become general practice.
A zero rate of postoperative complications in this case study analysed suggests that early extubation in operated patients has been safe and effective, although it may be stated that due to the low frequency of this practice, the choice of potential candidates is still highly conservative, as shown by Akhtar et al.11
Early extubation in patients who have undergone corrective congenital cardiopathy surgery has been a highly sought after goal since the decade of the 1980s in several international surgical centres, as reported by other authors.44,45 Success rates for early extubation were reported as very high by one author,37 as 93% of success in one study with 201 patients. From this time onwards the practice of early extubation began to gain higher acceptance. Rates of early extubation in the Garrahan Hospital were still very low compared with these background data. This could be explained because in patients with tetralogy of Fallot, early extubation continues to pose challenges which involve interdisciplinary work from the surgical team, as reported by some authors.11,42,46
Regarding the management of anaesthesia drugs, according to some authors41–44 in the decade of 1980s, in corrective surgery of tetralogies of Fallot high doses of narcotics were used to prevent response to stress during surgery and to avoid haemodynamic instability and pulmonary vasoconstrictive response during aspirations. However, nowadays low doses of these drugs have proven to be able to obtain potential benefit as early extubation may be performed, with the consequent reduction of cardiac and respiratory morbidity, an increase in cardiac output and a lower rate of ventilator-associated pneumonia.42 In this study the only drug which has been proven to have an association with early extubation was milrinona, which is consistent with other findings.11,18,20,46,47
Regarding fentanyl, in this study the group of patients with early extubation received average doses under 15mcg/kg, whilst patients with late extubation received average doses above 20mcg/kg. Although these doses are lower than those which were used in earlier years,32 in other studies correct management of drugs is determined by the selection of patients who were candidates for early extubation.30,32,45
ConclusionWe may conclude from this study that early extubation is rare, although it is an effective alternative for lowering ICU length of stay. Also, the selection of patients who are candidates for early extubation must be consensual between the different health professionals with established criteria.
One of the limitations of this study was the low frequency of early extubations, preventing any significant differences in comparative analysis to be highlighted. It would therefore be pertinent to increase the same for future analysis.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Chaparro H, Abeldaño-Zuñiga RA. Factores asociados a la extubación temprana en pacientes con cirugía correctora de tetralogía de Fallot. Enferm Intensiva. 2019;30:152–162.