To assess non-invasive ventilation knowledge and skills among nurses and physicians in different contexts: equipment and contextual influences.
MethodCross-sectional, descriptive study in 4 intensive care units (ICU) (1 surgical, 3 medical-surgical), 1 postsurgical recovery unit, 2 emergency departments (ED) and 3 wards, in 4 hospitals (3 university, 1 community) with 407 professionals. A 13-item survey, validated in the setting, was applied (Kappa index, 0.97 (95% CI [.965–.975]).
ResultsNurses (63.7% response); physicians (39% response). The overall percentage of correct responses was 50%. Scored from 1 to 5, with lower scores reflecting more knowledge, nurses scored 3.27±.5 vs 2.62±.5 physicians, respectively (mean difference,.65 (95% CI: .48–.82, p<.001). There were no differences between hospitals or units (p=.07 and p=.09). A notable percentage of respondents incorrectly identified the patient-ventilator synchronization strategy as “covering the expiratory port” (intentional leaks) and pressing the mask against the patient's face (unintentional leaks) (28.2% ICU, 22.5% ED, 8.3% postoperative resuscitation, 61.5% wards), with no difference between nurses and physicians (27.9% vs 23.4%, p=.6). Only 50% of nurse respondents correctly answered a question about measuring mask size and just 11.7% of the nurses knew the “2-finger fit” adjustment.
ConclusionsThere was no difference in nurses’ and physicians’ knowledge according to the setting studied. The lack of knowledge regarding NIV therapy depended on training received and material available. To reduce the existent confusion between intentional and nonintentional leak, the use of a single type of NIV supply and providing an appropriate level of training for nurses is recommended.
Evaluar el conocimiento y habilidades de enfermeras y médicos en ventilación mecánica no invasiva en diferentes contextos: equipamiento e influencias contextuales.
MétodoEstudio descriptivo transversal en 4 unidades de cuidados intensivos (una quirúrgica, 3 polivalentes), una reanimación posquirúrgica, 2 áreas de urgencias y 3 salas de hospitalización, de 4 hospitales (3 universitarios y uno general) con 407 profesionales. Se administró una encuesta con 13 ítems, evaluando la validez del contenido (índice de Kappa 0,97 [95% IC: 0,965-0,975]).
ResultadosRespondieron el 63,7% de las enfermeras y el 39% de los médicos. El porcentaje de respuestas correctas fue del 50%. Con una puntuación del 1 al 5, en la que a menor puntuación más conocimiento, las enfermeras puntuaron 3,27±0,5 vs. 2,62±0,5 los médicos (diferencia de la media 0,65 [IC 95%: 0,48-0,82; p<0,001]). No hubo diferencias entre hospitales o unidades (p=0,07 y p=0,09). Un porcentaje notable de profesionales identificó como estrategia para mejorar la sincronización paciente-ventilador «tapar el puerto espiratorio» (fugas intencionadas) y apretar la máscara a la cara del paciente (fugas no intencionadas) (28,2% unidad de cuidados intensivos, 22,5% urgencias, 8,3% reanimación posquirúrgica, 61,5% hospitalización), sin diferencia entre enfermeras y médicos (27,9% vs. 23,4%, p=0,6). El 50% de las enfermeras respondieron correctamente cómo seleccionar el tamaño adecuado de máscara y el 11,7% conocía que la máscara debe ajustarse permitiendo el paso de 2 dedos.
ConclusionesNo hubo diferencias en el conocimiento por unidades entre enfermeras y médicos. La falta de conocimiento relacionada con la terapia de la ventilación mecánica no invasiva es dependiente de la formación recibida y del material disponible en la unidad. Para reducir la confusión entre fugas intencionadas y no intencionadas se recomienda usar un solo tipo de ventilador y mantener un entrenamiento regular de las enfermeras.
We have determined a lack of protocols on how to implement and monitor NIV in different units where this technique is used (ICU, ED, postsurgical recovery and wards) as well as material diversity, both expendable material (interface and fixing systems) and ventilators (conventional or NIV specific). Surveys in Italian wards and French ICU highlighted the insufficient training of nurses in knowledge and skills to manage the NIV. In Spain only one previous study on knowledge of nursing staff on NIV has been carried out.
What this study provides?The lack of knowledge regarding NIV therapy is dependent on training received and material available. Doctors are the master trainers which does not allow nurse to training specific nursing skills. The greater the variability of ventilators, the greater the confusion with the adequate expendable material causing errors in tolerance to air leaking (intentional versus non intentional).
Study implicationsThe NIV experts (nurses and doctors) validated survey can be used to evaluate the level of knowledge and skills of staff and use it as a starting point to perform adequate training to improve implementation and monitoring of NIV.
The main objectives of noninvasive mechanical ventilation (NIV) are avoiding tracheal intubation, to facilitate early extubation and avoid reintubation1 and reducing the risk of ventilator-associated pneumonia.2 Over the past 20 years, NIV use has increased internationally, as reported by Esteban et al.3 for Europe and by Walkey and Wiener4 in the United States. Despite increased use, however, there continue to be disparities in applying the treatment and a lack of protocols, care standards and data registries, mostly due to the unit where most patients are admitted for NIV therapy.5–8 Numerous studies have identified risk factors for NIV failure, differentiating between ARF and acute hypercapnic respiratory failure (AHRF),3,4,9–11 and a recent systematic review included NIV complications12 even though these were reported in only 45% of the studies reviewed.
Interface selection is the key element in therapeutic success or failure because it affects patient comfort and avoids excessive air leakage, both of which are important in optimizing patient-ventilator synchronization.13,14 Health professionals also must be able to properly select patients for NIV and identify signs of NIV failure, promptly initiating tracheal intubation and invasive mechanical ventilation when indicated since delays are responsible for the high mortality rates when NIV is unsuccessful.3
The success of NIV therapy depends on effective teamwork. Doctors order the therapy and specify the unit where it should be initiated, while nurses (or respiratory therapists, in the United States, Australia and some European countries15,16) are responsible for the tasks that are essential for optimal NIV results: selecting the correct interface, positioning it properly, providing patient care and recording data. Crimi's international survey5 asked physicians about the interface of choice, as they were not only responsible for the ventilator election but also the interface, while in Spain the interface election is a nursing duty, as evidenced by previous studies carried on by our research team.8,17 Cabrini18 in Italian wards and Montravers19 in French ICU highlighted the insufficient training of nurses in knowledge and skills to manage the NIV. In Spain only one previous study on knowledge of nursing staff on NIV has been carried out17 and due that the NIV success depends on the team work between nurses and doctors (physiotherapists are not usually involved in the therapy) the present study aimed to evaluate NIV knowledge and skills among nurses and physicians in different types of hospitals (university versus community) and units: intensive care (ICUs), recovery (postsurgical and emergency departments) and general wards.
MethodsA cross-sectional, descriptive, multicenter study was carried out at 3 university hospitals (Hospital Universitari de Bellvitge, Hospital Dr. Josep Trueta de Girona, Hospital Clínic de Barcelona) and 1 community hospital (Consorci Hospitalari de Vic) during the first semester of 2016. Participants included all nurses and physicians (n=407) from 4 ICUs (1 surgical, 3 medical-surgical), 3 recovery units (1 postsurgical, 2 in emergency departments [EDs]) and 3 general wards. There were not respiratory therapists in the participating units.
Nurses and doctors hired as regular staff with no restriction of time and professional category were included (weekend staff was also included). Only doctors that were never on call were excluded as considered that they could prescribe the NIV but did not supervise the maintenance. Independent variables to identify the sample analyzed such as professional years of professional experience, in the service and with NIV were controlled.
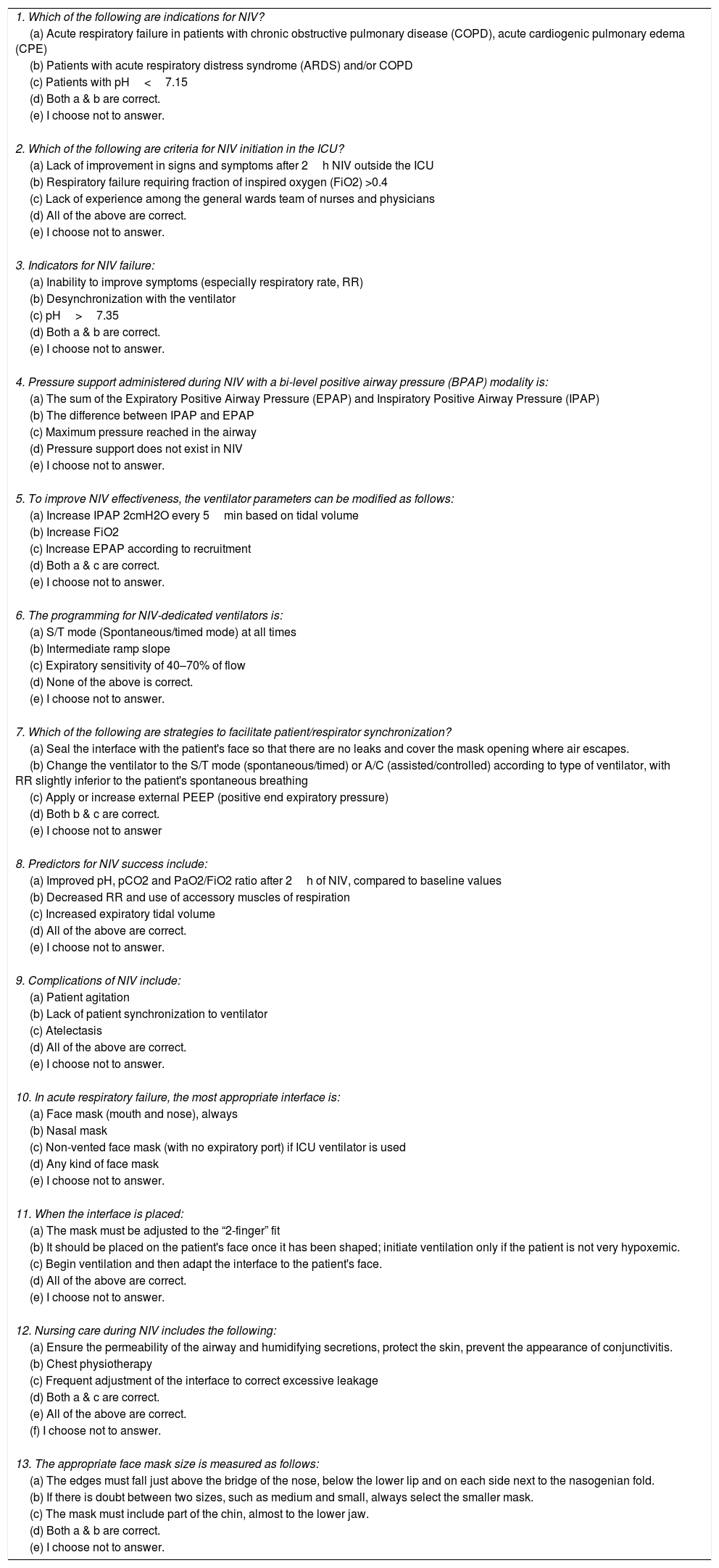
Data collectionResearchers with academic and clinical NIV experience designed and validated a survey, with 13 closed-ended multiple-choice questions.
The items were generated from a bibliographic review performed by the research team and content validity was assessed via a Delphi procedure in 28 health professionals from all participating hospitals. Regarding expertise in NIV and healthcare area the physician:nurse ratio was stracted. ICU, 6 physicians, 13 nurses (1:6); ED, 2 physicians, 5 nurses (1:3); and 2 nurses from general wards participated. They commented on three aspects of the survey: Clarity (Are any questions ambiguous? If so, which ones? Suggestions to make them more clear?), Face validity (Can any questions be deleted?), and Content validity (Any additional questions that must be included?). The survey was revised according to feedback received. No items were removed of added, however wording was modified in 4 items. The final version had a Kappa Index of 0.97 (95% CI [0.965–0.975]. The ideal time of response was not calculated as a high variability was observed in the pilot study. An English translation of the original, validated instrument is provided below (Table 1) and the correct answers are attached as Annex 1.
Survey of NIV knowledge and skills for health professionals.
| 1. Which of the following are indications for NIV? |
| (a) Acute respiratory failure in patients with chronic obstructive pulmonary disease (COPD), acute cardiogenic pulmonary edema (CPE) |
| (b) Patients with acute respiratory distress syndrome (ARDS) and/or COPD |
| (c) Patients with pH<7.15 |
| (d) Both a & b are correct. |
| (e) I choose not to answer. |
| 2. Which of the following are criteria for NIV initiation in the ICU? |
| (a) Lack of improvement in signs and symptoms after 2h NIV outside the ICU |
| (b) Respiratory failure requiring fraction of inspired oxygen (FiO2) >0.4 |
| (c) Lack of experience among the general wards team of nurses and physicians |
| (d) All of the above are correct. |
| (e) I choose not to answer. |
| 3. Indicators for NIV failure: |
| (a) Inability to improve symptoms (especially respiratory rate, RR) |
| (b) Desynchronization with the ventilator |
| (c) pH>7.35 |
| (d) Both a & b are correct. |
| (e) I choose not to answer. |
| 4. Pressure support administered during NIV with a bi-level positive airway pressure (BPAP) modality is: |
| (a) The sum of the Expiratory Positive Airway Pressure (EPAP) and Inspiratory Positive Airway Pressure (IPAP) |
| (b) The difference between IPAP and EPAP |
| (c) Maximum pressure reached in the airway |
| (d) Pressure support does not exist in NIV |
| (e) I choose not to answer. |
| 5. To improve NIV effectiveness, the ventilator parameters can be modified as follows: |
| (a) Increase IPAP 2cmH2O every 5min based on tidal volume |
| (b) Increase FiO2 |
| (c) Increase EPAP according to recruitment |
| (d) Both a & c are correct. |
| (e) I choose not to answer. |
| 6. The programming for NIV-dedicated ventilators is: |
| (a) S/T mode (Spontaneous/timed mode) at all times |
| (b) Intermediate ramp slope |
| (c) Expiratory sensitivity of 40–70% of flow |
| (d) None of the above is correct. |
| (e) I choose not to answer. |
| 7. Which of the following are strategies to facilitate patient/respirator synchronization? |
| (a) Seal the interface with the patient's face so that there are no leaks and cover the mask opening where air escapes. |
| (b) Change the ventilator to the S/T mode (spontaneous/timed) or A/C (assisted/controlled) according to type of ventilator, with RR slightly inferior to the patient's spontaneous breathing |
| (c) Apply or increase external PEEP (positive end expiratory pressure) |
| (d) Both b & c are correct. |
| (e) I choose not to answer |
| 8. Predictors for NIV success include: |
| (a) Improved pH, pCO2 and PaO2/FiO2 ratio after 2h of NIV, compared to baseline values |
| (b) Decreased RR and use of accessory muscles of respiration |
| (c) Increased expiratory tidal volume |
| (d) All of the above are correct. |
| (e) I choose not to answer. |
| 9. Complications of NIV include: |
| (a) Patient agitation |
| (b) Lack of patient synchronization to ventilator |
| (c) Atelectasis |
| (d) All of the above are correct. |
| (e) I choose not to answer. |
| 10. In acute respiratory failure, the most appropriate interface is: |
| (a) Face mask (mouth and nose), always |
| (b) Nasal mask |
| (c) Non-vented face mask (with no expiratory port) if ICU ventilator is used |
| (d) Any kind of face mask |
| (e) I choose not to answer. |
| 11. When the interface is placed: |
| (a) The mask must be adjusted to the “2-finger” fit |
| (b) It should be placed on the patient's face once it has been shaped; initiate ventilation only if the patient is not very hypoxemic. |
| (c) Begin ventilation and then adapt the interface to the patient's face. |
| (d) All of the above are correct. |
| (e) I choose not to answer. |
| 12. Nursing care during NIV includes the following: |
| (a) Ensure the permeability of the airway and humidifying secretions, protect the skin, prevent the appearance of conjunctivitis. |
| (b) Chest physiotherapy |
| (c) Frequent adjustment of the interface to correct excessive leakage |
| (d) Both a & c are correct. |
| (e) All of the above are correct. |
| (f) I choose not to answer. |
| 13. The appropriate face mask size is measured as follows: |
| (a) The edges must fall just above the bridge of the nose, below the lower lip and on each side next to the nasogenian fold. |
| (b) If there is doubt between two sizes, such as medium and small, always select the smaller mask. |
| (c) The mask must include part of the chin, almost to the lower jaw. |
| (d) Both a & b are correct. |
| (e) I choose not to answer. |
Note: Several versions of the survey were generated, alternating the order of questions and responses, in order to make it more difficult to share correct answers.
The survey was given in paper format to the participants by the principal investigator of each hospital. At the cover page the study purpose and aims were explained, as well as the fact that returning a completed survey indicated informed consent to participate. All surveys were collected 30 days after completion. A container was enabled for this purpose. Confidentiality was strictly protected by the aggregation of reported data. The clinical research ethics committee in each participating hospital approved the study.
The following variables were analyzed:
- •
Nurses’ knowledge about proper type, size, and placement of the NIV mask (questions 10, 11 and 13).
- •
Physicians’ knowledge about NIV indication (question 1), unit were should be done (question 2), ventilator programming (questions 4, 5, 6); their responses to question 10 (a nursing question in our setting) also were compared with European studies asking a similar question to physicians.5
• Both professionals: predictors for NIV success and failure (questions 8 and 3, respectively), strategies to facilitate patient/respirator synchronization (question 7), NIV complications (question 9) and nursing care during NIV (question 12).
The variability of knowledge among professionals was calculated assigning the value 1 to the correct answer, the value 3 to the answer “do not response” and the value 5 to the incorrect answer, so the highest score, the lower level of knowledge of the staff. Unit supervisors were contacted to determine which type of ventilator, interface, and other supplies were used routinely (Annex 2) and if NIV-related training had been offered within 3 years (Annex 3).
Data analysisDescriptive analysis of participant responses included frequency and percentage of correct and incorrect answers to each question. In a second analysis, the response variable was coded quantitatively, assigning a value of 1 to a correct answer, 3 to “no response” and 5 to an incorrect answer. The mean (standard deviation) score was described and compared for each item according it's a physician question (items 1, 2, 4, 5, 6), nurses question (items 10, 11, 13) or both (items 3,7,8, 9,12) and finally by units and professions. Inferential analysis was done with Fisher or Chi square test as appropriate for qualitative variables and Student T test for quantitative. Units with similar characteristics (4 ICUs and 2 EDs) were analyzed as subgroups. A p-value <0.05 was considered significant. All statistical analysis was done using IBM SPSS Statistics v. 18 (IBM Statistics®, Markham, ON, Canada).
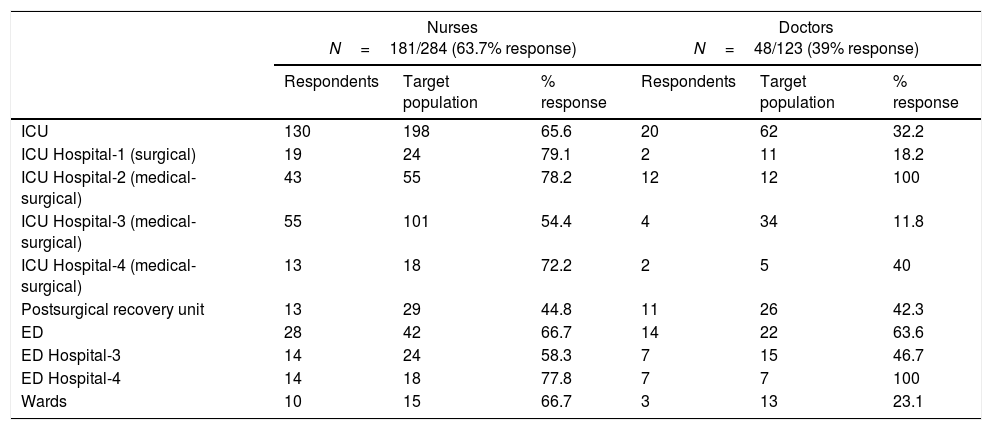
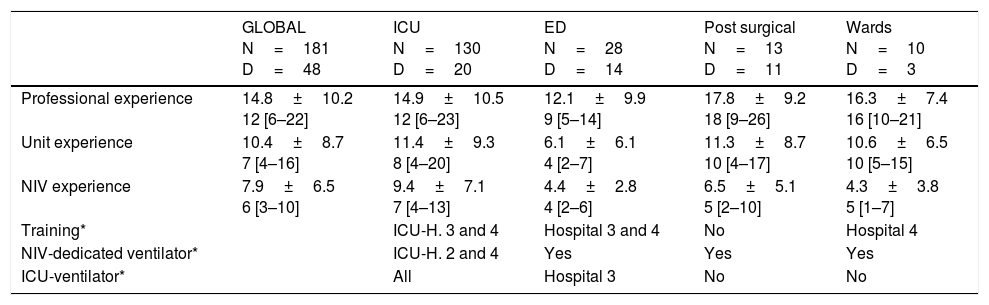
ResultsWe compared the completed surveys with the number of registered professionals in the units (Table 2) and 181 nurses answered the survey (63.7%) and 48 doctors (39%), being higher the participation by units of nurses versus doctors, mainly in wards and ICU. In Table 3 characteristics of registered professionals by unit are described (years of clinical experience in the unit and with NIV therapy). ED professionals had the least in-unit experience (mean difference (MD) of 5.4 years, 95% CI [3.1–7.8], p<0.001) and also with NIV (MD of 4.9 years, 95% CI [3.5–6.5], compared with ICU professionals, as same as professionals on general wards with ICU professionals NIV experience (MD of 5.1 years, 95% CI [2.4–7.7], (p=0.001). These differences were not observed in ED departments in Hospitals 3 and 4 (university and community hospitals, respectively): ED professionals did not differ in years of professional experience (4[1.5–6] vs 4 [2–9], p=0.96), in-unit (both 1 [1–2], p=0.99), or with NIV (5[3.5–6] vs 3[2–5], p=0.08).
Percentage response per unit and professional category.
| Nurses N=181/284 (63.7% response) | Doctors N=48/123 (39% response) | |||||
|---|---|---|---|---|---|---|
| Respondents | Target population | % response | Respondents | Target population | % response | |
| ICU | 130 | 198 | 65.6 | 20 | 62 | 32.2 |
| ICU Hospital-1 (surgical) | 19 | 24 | 79.1 | 2 | 11 | 18.2 |
| ICU Hospital-2 (medical-surgical) | 43 | 55 | 78.2 | 12 | 12 | 100 |
| ICU Hospital-3 (medical-surgical) | 55 | 101 | 54.4 | 4 | 34 | 11.8 |
| ICU Hospital-4 (medical-surgical) | 13 | 18 | 72.2 | 2 | 5 | 40 |
| Postsurgical recovery unit | 13 | 29 | 44.8 | 11 | 26 | 42.3 |
| ED | 28 | 42 | 66.7 | 14 | 22 | 63.6 |
| ED Hospital-3 | 14 | 24 | 58.3 | 7 | 15 | 46.7 |
| ED Hospital-4 | 14 | 18 | 77.8 | 7 | 7 | 100 |
| Wards | 10 | 15 | 66.7 | 3 | 13 | 23.1 |
ICU, Intensive Care Unit; ED, Emergency Department.
Hospitals 1, 2, 3 are university hospitals; hospital-4 is a community hospital.
Nurses and doctors years of experience in the unit and with NIV therapy.
| GLOBAL N=181 D=48 | ICU N=130 D=20 | ED N=28 D=14 | Post surgical N=13 D=11 | Wards N=10 D=3 | |
|---|---|---|---|---|---|
| Professional experience | 14.8±10.2 12 [6–22] | 14.9±10.5 12 [6–23] | 12.1±9.9 9 [5–14] | 17.8±9.2 18 [9–26] | 16.3±7.4 16 [10–21] |
| Unit experience | 10.4±8.7 7 [4–16] | 11.4±9.3 8 [4–20] | 6.1±6.1 4 [2–7] | 11.3±8.7 10 [4–17] | 10.6±6.5 10 [5–15] |
| NIV experience | 7.9±6.5 6 [3–10] | 9.4±7.1 7 [4–13] | 4.4±2.8 4 [2–6] | 6.5±5.1 5 [2–10] | 4.3±3.8 5 [1–7] |
| Training* | ICU-H. 3 and 4 | Hospital 3 and 4 | No | Hospital 4 | |
| NIV-dedicated ventilator* | ICU-H. 2 and 4 | Yes | Yes | Yes | |
| ICU-ventilator* | All | Hospital 3 | No | No |
N=nurses, D=doctors, H=hospital.
* Detailed information about supplies used in each unit, along with the number of hours and teaching methods used to deliver training in the study units, is included in Annex 2 and 3.
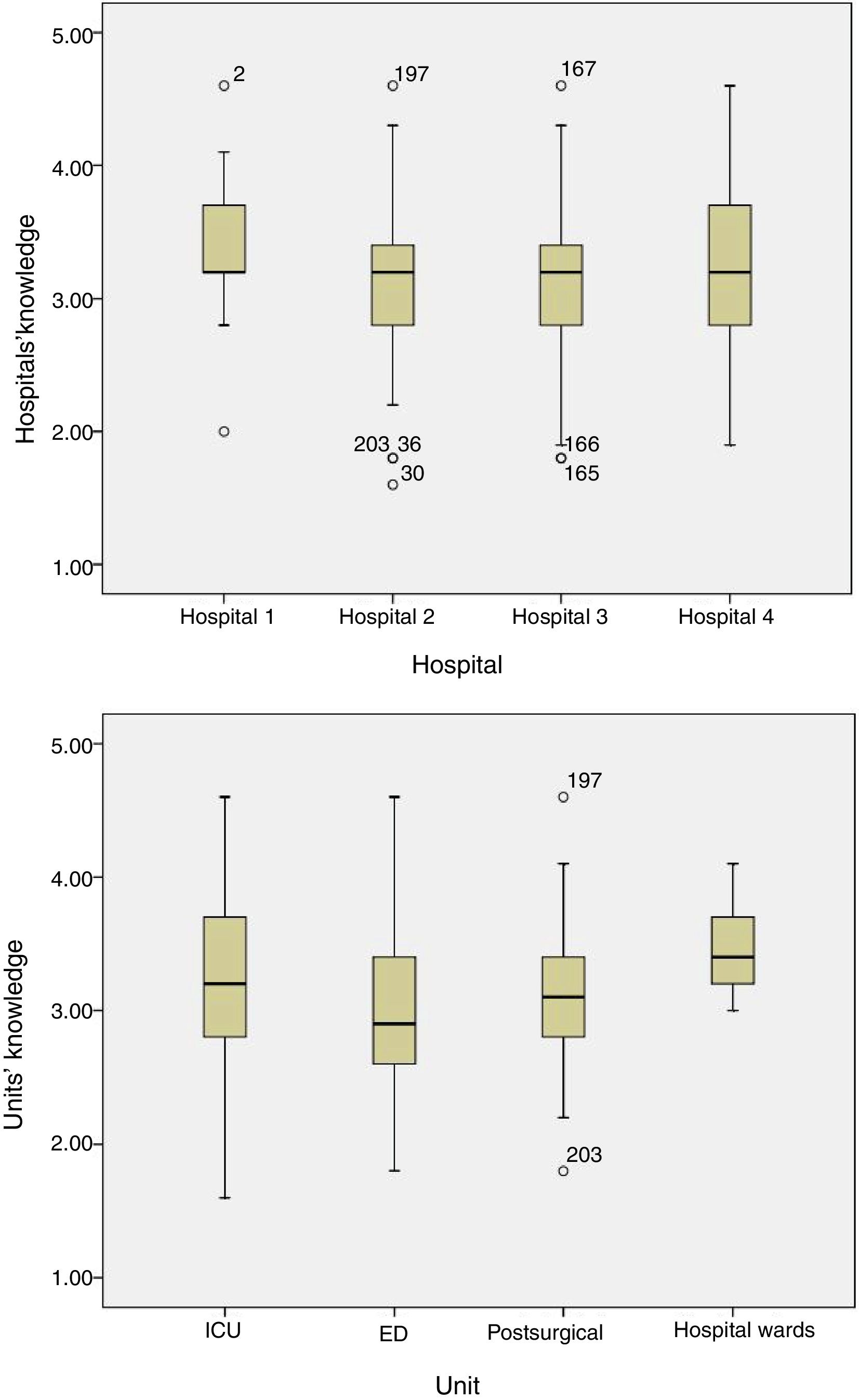
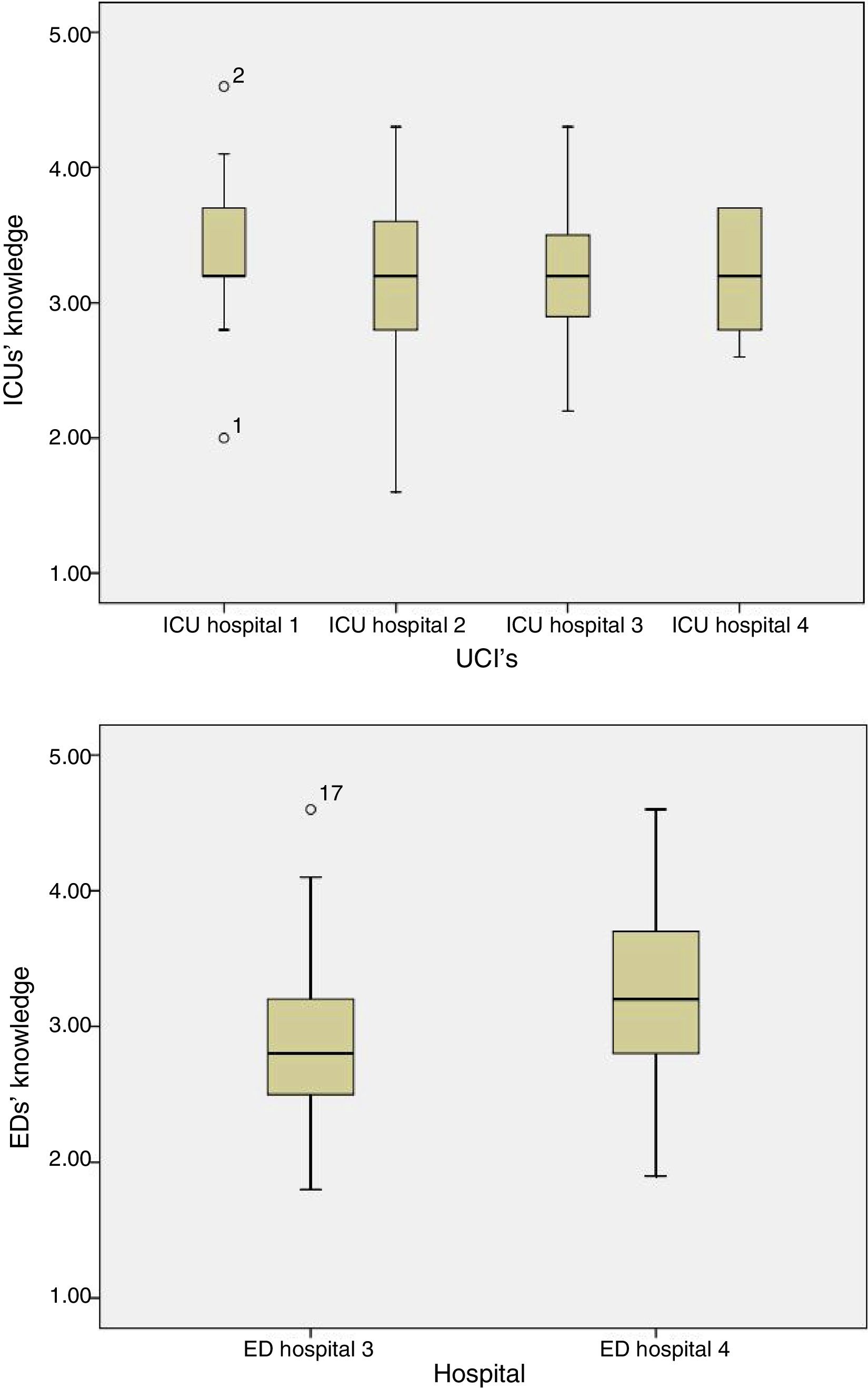
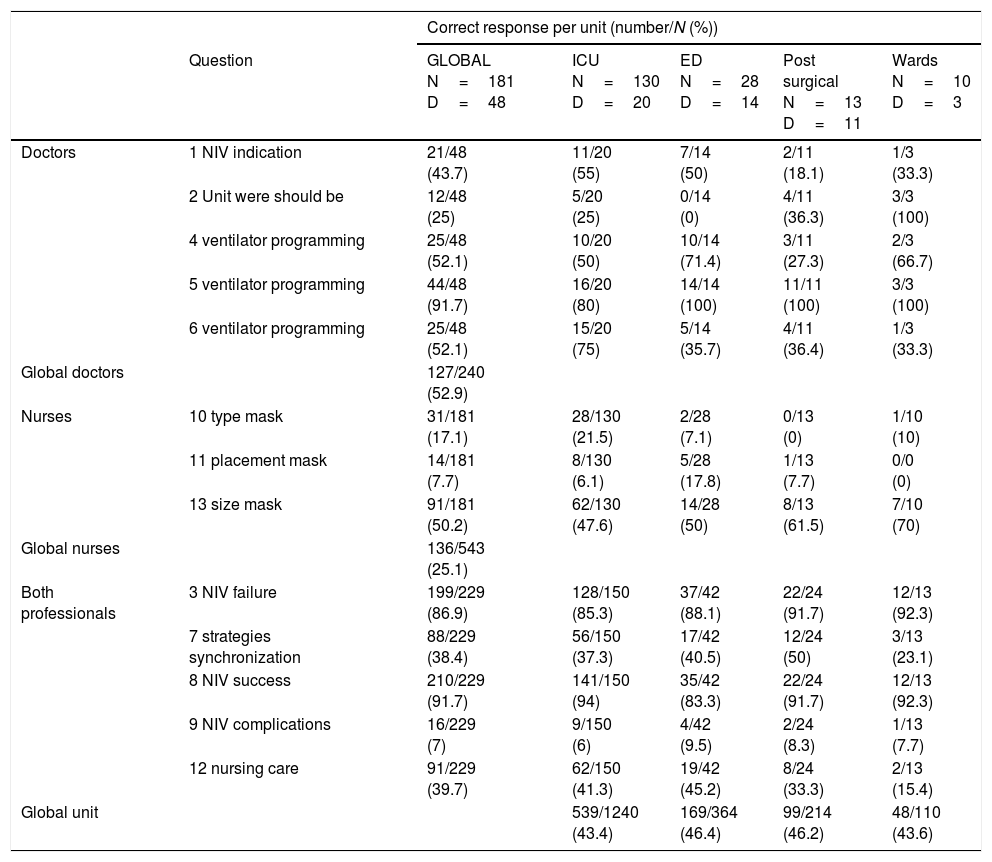
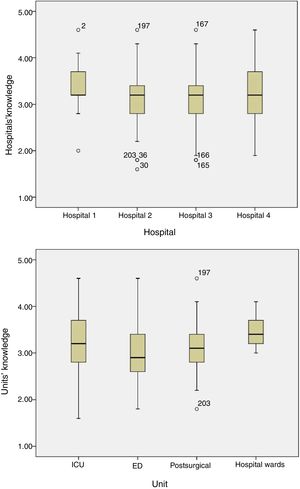
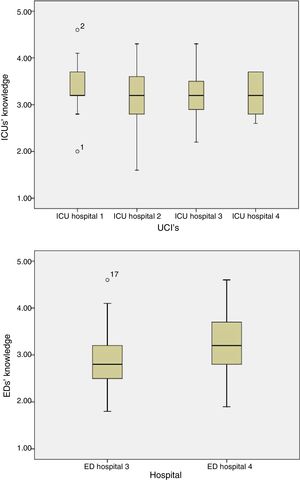
Related to nursing competencies, 25.1% of the surveyed answered correctly. Nearly 50% of responses were correct answers for each unit (Table 4), with no differences between hospitals or unit types (p=0.07 and p=0.09, respectively, Fig. 1) or between ICUs (p=0.2) or ED recovery units (p=0.1) of the different hospitals (Fig. 2).
Percentage response per unit and professional category (N=nurses, D=doctors).
| Correct response per unit (number/N (%)) | ||||||
|---|---|---|---|---|---|---|
| Question | GLOBAL N=181 D=48 | ICU N=130 D=20 | ED N=28 D=14 | Post surgical N=13 D=11 | Wards N=10 D=3 | |
| Doctors | 1 NIV indication | 21/48 (43.7) | 11/20 (55) | 7/14 (50) | 2/11 (18.1) | 1/3 (33.3) |
| 2 Unit were should be | 12/48 (25) | 5/20 (25) | 0/14 (0) | 4/11 (36.3) | 3/3 (100) | |
| 4 ventilator programming | 25/48 (52.1) | 10/20 (50) | 10/14 (71.4) | 3/11 (27.3) | 2/3 (66.7) | |
| 5 ventilator programming | 44/48 (91.7) | 16/20 (80) | 14/14 (100) | 11/11 (100) | 3/3 (100) | |
| 6 ventilator programming | 25/48 (52.1) | 15/20 (75) | 5/14 (35.7) | 4/11 (36.4) | 1/3 (33.3) | |
| Global doctors | 127/240 (52.9) | |||||
| Nurses | 10 type mask | 31/181 (17.1) | 28/130 (21.5) | 2/28 (7.1) | 0/13 (0) | 1/10 (10) |
| 11 placement mask | 14/181 (7.7) | 8/130 (6.1) | 5/28 (17.8) | 1/13 (7.7) | 0/0 (0) | |
| 13 size mask | 91/181 (50.2) | 62/130 (47.6) | 14/28 (50) | 8/13 (61.5) | 7/10 (70) | |
| Global nurses | 136/543 (25.1) | |||||
| Both professionals | 3 NIV failure | 199/229 (86.9) | 128/150 (85.3) | 37/42 (88.1) | 22/24 (91.7) | 12/13 (92.3) |
| 7 strategies synchronization | 88/229 (38.4) | 56/150 (37.3) | 17/42 (40.5) | 12/24 (50) | 3/13 (23.1) | |
| 8 NIV success | 210/229 (91.7) | 141/150 (94) | 35/42 (83.3) | 22/24 (91.7) | 12/13 (92.3) | |
| 9 NIV complications | 16/229 (7) | 9/150 (6) | 4/42 (9.5) | 2/24 (8.3) | 1/13 (7.7) | |
| 12 nursing care | 91/229 (39.7) | 62/150 (41.3) | 19/42 (45.2) | 8/24 (33.3) | 2/13 (15.4) | |
| Global unit | 539/1240 (43.4) | 169/364 (46.4) | 99/214 (46.2) | 48/110 (43.6) | ||
Mean score by unit: Intensive Care Unit (ICU) and Emergency Department (ED).
Hospitals 1, 2, 3 are university hospitals; hospital 4 is a community hospital.
ICU, intensive care unit; ED, emergency department.
Correct answers were scored as 1 point, “no response” as 3 and an incorrect answer as 5. A higher score reflected lower knowledge.
Between the professions, however, nurses generally showed lower knowledge than physicians (3.27±0.5 vs 2.73±0.5, mean difference, 0.54 95%CI [0.37–0.71], p<0.001). Excluding the question about choosing the correct type of mask (#10) improved the physicians’ comparative score (mean difference 0.65 95%CI [0.48–0.82], p<0.001). The percentage of doctors participation is lower that nurse's, by unit and globally (Table 2). Doctor's knowledge cannot be extrapolated to the general knowledge in their units, except for the emergency units where the participation rate was 63.6%.
Physicians’ knowledge resultsNIV indications (question 1)Overall, 43.8% of physicians knew that chronic obstructive pulmonary disease (COPD) or acute cardiogenic pulmonary edema (CPE), have the same level of evidence. The remaining 52.1% responded that it was equally indicated in COPD and acute respiratory distress syndrome (ARDS). Physicians in post-surgical recovery unit had the lowest percentage of correct response.
Unit where NIV should be done (question 2)ED physicians did not consider a lack of NIV experience a criterion for admitting patients to ICU to receive NIV therapy (0% ED vs 100% wards [p<0.001], 36.4% postsurgical recovery unit [p=0.03], 26.3% ICU [p=0.04]).
Ventilator programming (questions 4–6)Most physicians in EDs (10/12) and general wards (2/3) defined pressure support (PS) as the difference between inspiratory positive airway pressure (IPAP) and expiratory positive airway pressure (EPAP), compared to postsurgical (3/11) and ICU (10/20) physicians. All ED, postsurgical, and general-ward physicians, but only 16/20 in ICUs, knew how to use IPAP and EPAP to improve alveolar recruitment and optimize NIV efficacy. Among ICU physicians, 15/20 knew that NIV-dedicated respirators should not always be programmed in spontaneous/timed (S/T) mode or intermediate slope, and that the expiratory trigger is not a programmable parameter in older models. Five of 14 ED and 4/11 postsurgical physicians answered correctly. Two of 3 general-ward physicians indicated they always program in S/T mode. Differences between units were nonsignificant due to the small sample.
Nurses’ knowledge resultsSelection type, size and mask placement (questions 10, 11 and 13)The majority of nurses (69.6%) answered that a face mask should be used with ICU ventilators, but only 17.1% specified a non-vented mask, with no exhalation port; the percentage of correct responses was higher in ICUs than in other units, without reaching statistical significance. There was no difference between health professionals (17.1% nurses vs 29.2% physicians, p=0.07).
Half of all nurses, with no differences between units, knew how to measure the proper mask size, and that the smaller size should be selected if there were any doubt. Few nurses (11.7%) indicated that masks should allow enough space to allow 2 fingers to pass beneath the headgear, and there was a significant difference between ICU and ED nurses (6.2% vs 18.5%, respectively; p=0.03).
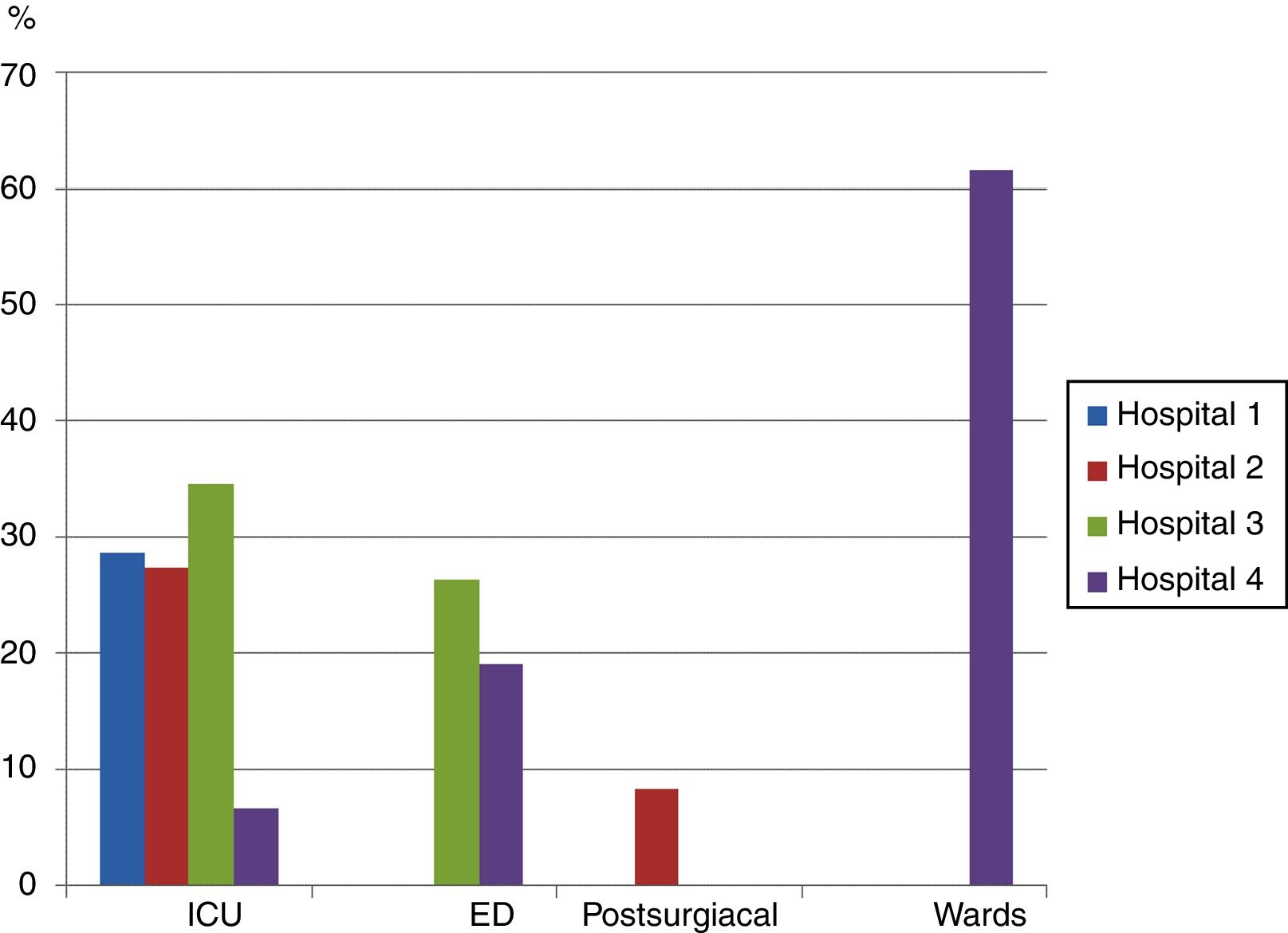
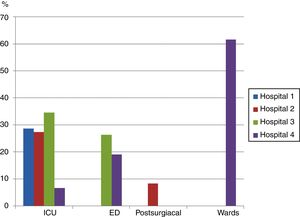
Both professionals resultsStrategies to facilitate patient-ventilator synchrony (question 7)As a strategy to facilitate patient-ventilator synchronization, many professionals chose “seal the interface with the patient's face so that there are no leaks and cover the mask opening where air escapes” (28.2% ICU, 22.5% ED, 8.3% postsurgical, 61.5% general wards, with a significant difference observed between the last two units, p=0.001). There was no significant difference between nurses and physicians (27.9% vs 23.4%, p=0.6); Fig. 3 shows the differences between units and hospitals.
Percentage of doctors and nurses at each unit who responded affirmatively to a question about whether covering the expiratory port and pressing the mask against the patient's face is an appropriate strategy to improve patient-ventilator synchronization.
The difference between the ICUs of hospital 3 and hospital 4 approached significance, p=0.05.
Only the surgical ICU identified agitation as NIV complication compared to other ICUs (33.3% vs 1.8% hospital-2 [p<0.001], 1.7% hospital-3 [p<0.001], and 0% hospital-4, [p=0.02]).
In general, only 7% of respondents identified agitation as a potential complication, with no differences between units or professions (nurses 6.6% vs physicians 8.3%, p=0.7).
Nursing care during NIV (question 12)More ICU and ED professionals (41.3% and 45.2%, respectively) considered respiratory therapy to be necessary during NIV, compared to those on general wards (15.4%, p=0.05). More than half of the physicians (54.2%) and nurses (55.1%) did not consider respiratory physiotherapy a nursing task (p=1). In a comparison of hospitals 3 and 4 (university and community hospitals, respectively), Hospital 3 professionals more frequently included respiratory physiotherapy as part of NIV care (61.9% vs 28.6% in ED, p=0.03, and 50% vs 20% in ICU, p=0.04, respectively).
DiscussionAlthough ICUs had more experience with NIV, this was not reflected in greater knowledge compared to the other units studied, perhaps because of the emergence of NIV-specific ventilators that are better known and more frequently used outside of ICUs. Nurses seemed to be more clear about what kind of interface to select when there was less variety in the supplies to be used. There was no difference between any of the hospitals studied. Nurses showed a lower knowledge than doctors due to the lasts being in charge of NIV nurses training, which means that the training has only been theoretical and have not received proper training in their own competencies (interface size selection and correct placement). This is evident by the responses of both guilds where they all would cover expiratory port in a vented mask (intentional leak) to improve the patient-ventilator synchronization.
Half of the doctors who responded would equally consider NIV in COPD and ARDS, although NIV is indicated at evidence level 1 and 3, respectively.1,20 In fact, annual use of NIV in the United States increased 400% in patients with ARF from 2000 to 2009, compared to 250% in patients with COPD.4 In Spain, Fernandez-Vivas et al.21 analyzed only ICUs and concluded that NIV is underused in COPD and CPE, but its use in patients with ARF, compared to other conditions, had quintupled, from 12% to 64% of cases. In ED studies, Andreu-Ballester et al.22 in Spain and Oszancak et al.23 in the United States reported that NIV use in patients with COPD had shifted from the ICU to the ED.
The responses from physicians may reflect the usual practice in the unit where they work. Compared to ICU and ED settings, correct responses were lower in post-surgical recovery and general wards, where NIV indication is clearly associated with the prevention of post-operative ARF or exacerbation of AHRF, respectively.
Although ICU physicians were the NIV pioneers, their knowledge of programming NIV-specific ventilators was no greater than in ED or general wards. A recent European survey by Crimi et al.5 showed that intensivists and anesthesiologists prefer conventional ICU ventilators with an NIV module, while internists and pneumologists would choose NIV-specific ventilators.
Nurses working in ICUs, where conventional ventilators are mainly used, were more aware that the mask of choice should be non-vented because those ventilators do not require intentional air leaks, given the presence of both inspiratory and expiratory ventilator circuits. Therefore, it is logical that ICU nurses in university hospitals 1 and 3 showed an intolerance of air leaks; a third of them would cover the exhalatory port to improve patient synchronization with the ventilator because they are not familiar with intentional air escapes. On the other hand, in units that only have NIV-specific ventilators (ED and general wards, Hospital 4; recovery unit, Hospital 2), nurses unfamiliar with non-vented masks would be convinced of the need to use a vented mask with an exhalatory port to release carbon dioxide. The ventilators they use have only one circuit, so they must have greater tolerance for intentional air leaks.
The present study showed that the use of different types of NIV supplies causes confusion; this finding agrees with the conclusions reached by Stieglitz et al.24,25 In units that have both types of equipment (Hospital 2's ICU and Hospital 3's ED, the health professionals were confused; the percentage who would cover the exhalatory port was equal to that in units where only conventional ventilators with a non-vented mask were used (ICUs in hospitals 1 and 3). Only the professional staff of Hospital 4, a community hospital, was clear on this question.
The lack of knowledge among the respondents (mainly nurses) working on general hospital wards was of more concern. Two thirds of them would cover the exhalatory port, even though they were only using NIV-specific ventilators. In a study by Cabrini et al.,18 only 12 of 90 general ward nurses surveyed had received adequate training in NIV therapy. Even though NIV is mainly initiated and monitored by nurses in European hospitals,15 there is a general lack of training that concurs with the results of the present study. This is especially true for the skills for which nurses are responsible: selecting the proper face mask size and securing it correctly. This is probably due to a trial-and-error approach to training, using the supplies available in the unit, with no opportunity to participate in training sessions led by expert nurses and practice on low-fidelity simulators or a standardized patient. Montravers et al.19 surveyed 32 ICUs in France, concluding that nurses had received NIV training in only 39% of the units, and this training was provided by physicians in 87% of cases, along with a few hours of practical training provided by the industry. Neither type of trainer would have any real-world experience with fitting the NIV mask or monitoring patient response to the therapy. It is important that nurses have trainers who know about choosing and fitting the proper mask size (many patients no longer have their own teeth, some have prominent noses, etc.) and who have cared for patients at all hours of the day and night, attempting to ensure that the mask remains in place throughout the therapy. These key nursing tasks are related to the air that escapes and therefore are key to patient-ventilator synchronization.9
This brings us to a discussion of unintentional leaks between the mask and the patient's skin, for which both types of ventilators (conventional and NIV-specific) can compensate without any problems.14 Successful NIV requires a change in attitude: tolerance of leaks while controlling them. Unintentional leaks are related to the “two-finger fit” rule, which avoids pressing the mask too tightly to the face and making the patient uncomfortable. This can lead to cessation of NIV therapy. At the same time, air leaks must be monitored because excessive loss will cause patient-ventilator asynchrony and NIV failure.13,14
Despite evidence of a relationship between sedation and agitation,26 in our study the only professionals who identified agitation as a potential NIV complication were the surgical ICU team, where the patients are postoperative and therefore recently sedated. The lack of awareness in other units is worrisome because a review by Hilbert et al.27 found that between 9% and 22% of patients cannot tolerate NIV because of pain, discomfort, claustrophobia or agitation. This complication can also lead to suspension of NIV therapy because the agitated patient removes the mask or its straps, increasing leakage and, as a result, asynchrony.
Considering the role of respiratory physiotherapy in NIV, most patients admitted to hospital wards with AHRF are stable10,28 and can manage secretions. Therefore, it is reasonable that professionals in these units would not identify respiratory therapy as part of NIV care. In contrast, this therapy is essential for NIV success in patients with ARF receiving care in ICUs, EDs, and post-surgical recovery.29,30 However, we found differences between the community and university hospital settings; in the latter, a higher percentage of respondents in ICUs and EDs saw a need for respiratory physiotherapy. According to Ozsancak et al.,23 in non-university hospitals the most frequent NIV indication is due to AHRF; secretion management would be routine in these patients and the health professionals would not see it as their responsibility. Nonetheless, it is cause for concern that nurses would not recognize physiotherapy as a nursing activity. The most recent edition of Nursing Intervention Classification (NIC),31 continues to list “thoracic physiotherapy” (NIC 3230). In addition, physiotherapy may be very much needed if, according to the European survey by Crimi et al.,5 only 50% of patients receive humidification during NIV therapy. Although classic “chest-clapping” is no longer recommended, new techniques such as high-frequency thoracic or intrapulmonary percussion can be used.29 This highlights the need for ongoing training of nurses to ensure best practice in NIV patient care, not only in choosing and fitting the correct mask but also in managing sedation, agitation and secretions.
LimitationsIn this first phase of our project, a survey was used to assess knowledge and skills; we are aware that this methodology has less internal validity than is provided by direct observation of professionals during NIV therapy. We accepted this risk because we found no evidence of any similar analysis in our field of study.
Results from the physician responses must be interpreted with caution because the response rate was 39%; nonetheless, this exceeds the rate reported in other studies (e.g., 27% in Devlin et al.32) and is about 12% lower than the 51.3% achieved by Crimi et al.5
We did not weight responses by the number of physicians respondents who were surveyed for unit in the quantitative analysis. This fact limits the generalization of the results in this group, although a differential qualitative analysis for unit was done.
ConclusionsThere was no difference in nurses’ and physicians’ knowledge between any of the hospitals studied. To reduce the existent confusion between intentional (vented masks) and not intentional leak (leak between skin and interface) single type of NIV supply must be implemented in the units and maintaining an appropriate level of training in specific skills for both groups such as selection, sizing and fitting of the mask for nurses. They seemed to be more clear about what kind of interface to select when there was less variety in the supplies to be used.
Conflict of interestsThe authors have no conflict of interests to declare.
The authors appreciate the English language review by Elaine Lilly, PhD.
This work was supported by the European federation of Critical Care Nursing associations (EfCCNa Research Awards 2013)
Please cite this article as: Raurell-Torredà M, Argilaga-Molero E, Colomer-Plana M, Ródenas-Francisco A, Garcia-Olm M. Conocimiento y habilidades de enfermeras y médicos en ventilación mecánica no invasiva: equipamiento e influencias contextuales. Enferm Intensiva. 2019;30:21–32.