Direct-acting antivirals have greatly simplified the treatment of hepatitis C virus (HCV), yet circuits that bring diagnosis and treatment closer to people who inject drugs (PWID) are needed to achieve the elimination targets of the WHO. With this purpose we have established an externalized nurse-driven circuit among former and active PWID in an addiction centre (AC) and a harm reduction centre (HRC).
Methods and settingsThe nursing staff offered HCV screening, diagnosis and treatment to the AC and HRC users, administered medication after the hepatologist's remote prescription to those with an active infection who accepted being treated, and implemented educational and harm reduction interventions.
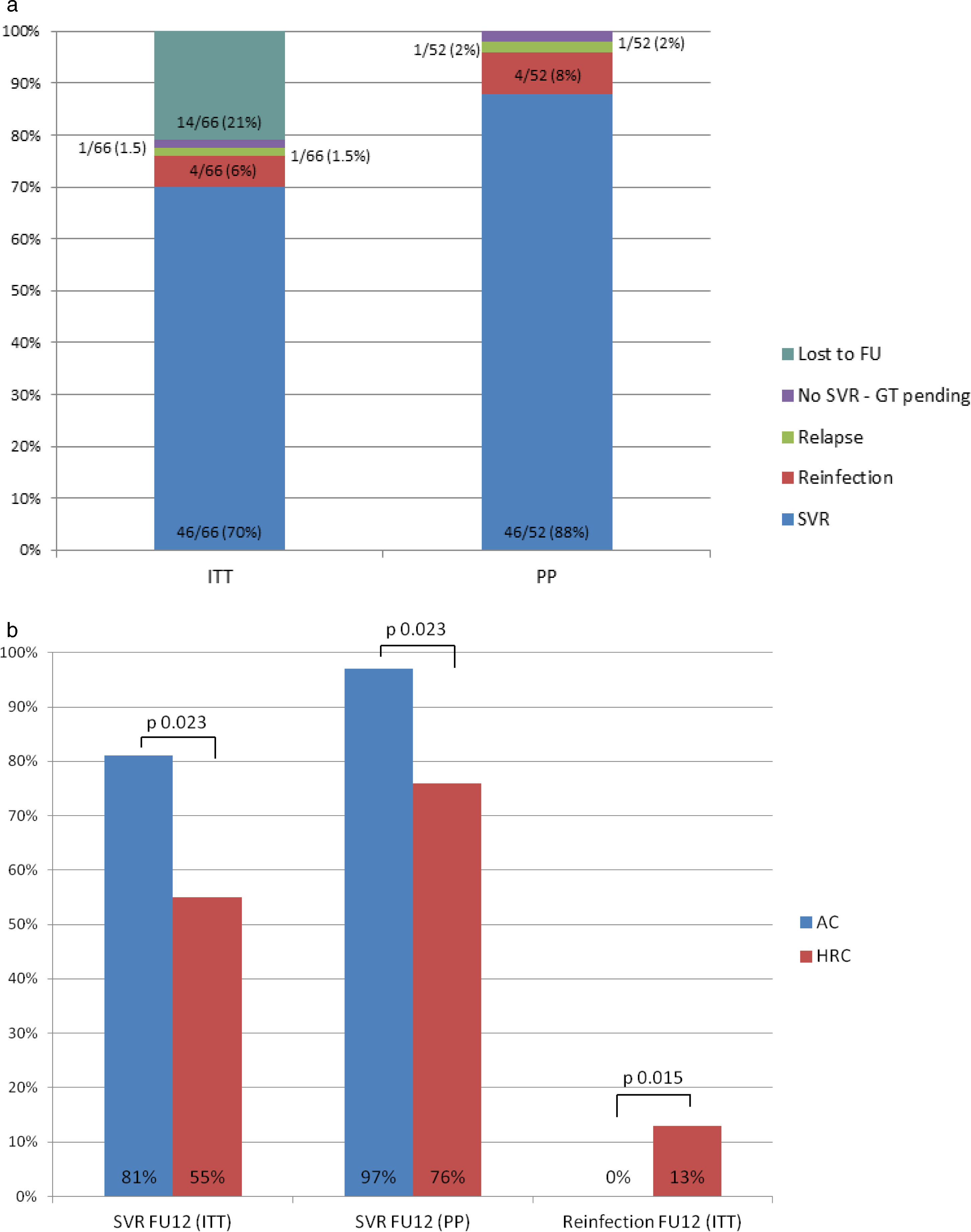
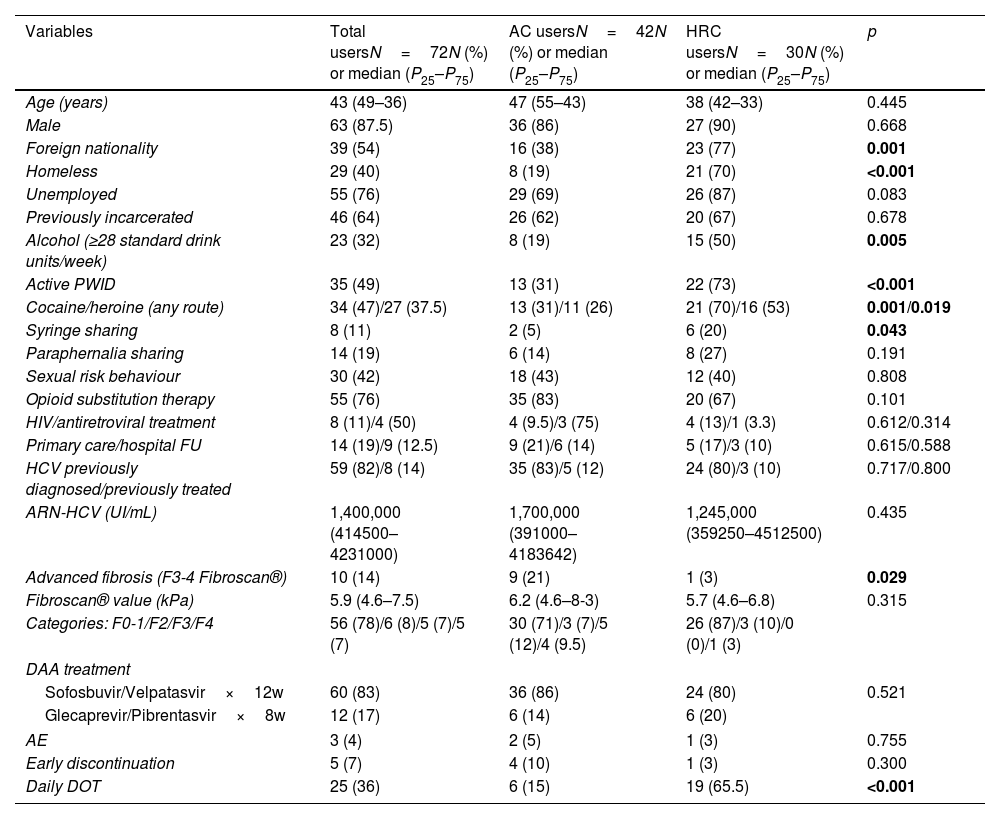
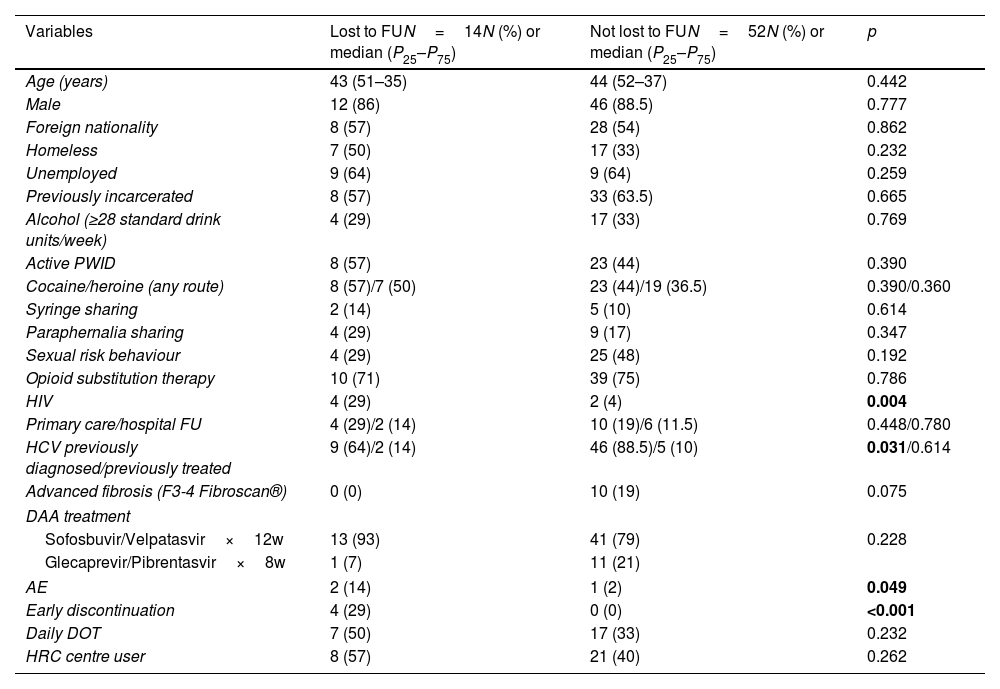
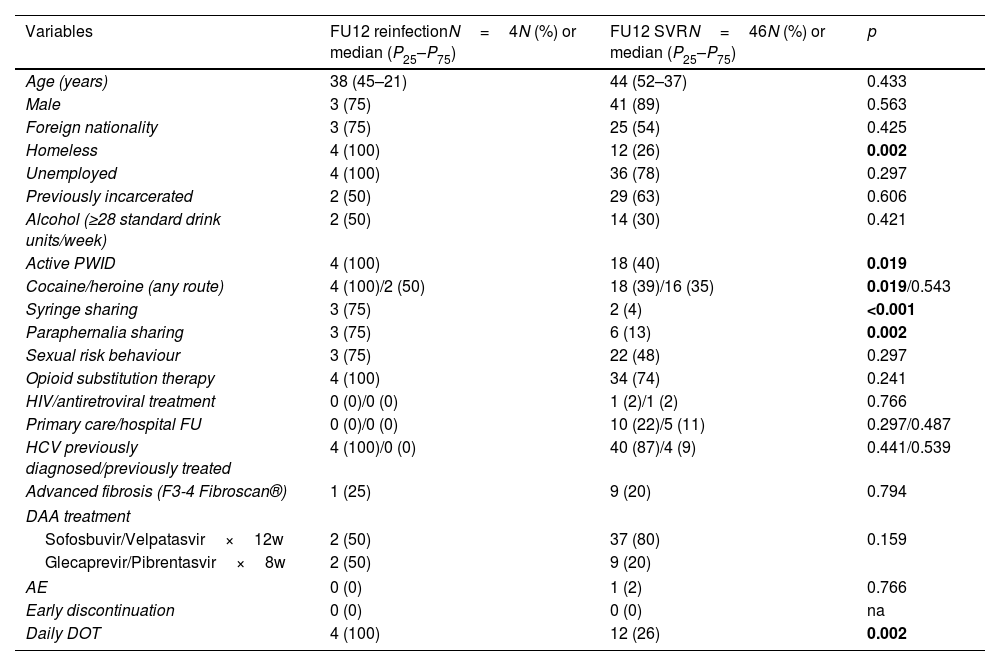
Participants and resultsBetween October 2018 and March 2021, 566 users accepted screening. 134 (24%) had an active infection, with a higher prevalence among HRC users (42% vs 17%; p<0.001), who were more frequently foreigners, homeless and reported active drug use and syringe sharing. Treatment initiation was similar between groups. Overall sustained viral response (SVR) for intention-to-treat (ITT) and per protocol (PP) was 70% and 88% respectively. Overall adherence was good in both groups; however, SVR was higher in AC users compared to HRC users (ITT-SVR 81% vs 55%). All reinfections (6% by ITT) occurred in the HRC group. Overall loss to follow-up rate was 21%.
ConclusionsThis patient-centred nurse-driven circuit demonstrates that HCV treatment can be successfully delivered to PWID even with active drug use and socio-economic complexity. User-specific characteristics need to be considered when setting up these interventions to maximize success.
Los antivirales de acción directa han simplificado el tratamiento del virus de la hepatitis C (VHC), pero es necesario acercar el diagnóstico y el tratamiento a las personas que se inyectan drogas (PQID). Con este propósito hemos establecido un circuito externalizado, liderado por enfermeras y dirigido a PQID antiguos y activos en un centro de adicciones (CA) y un centro de reducción de daños (CRD).
MétodosLas enfermeras ofrecieron cribado, diagnóstico y tratamiento del VHC a los usuarios del CA y del CRD, administraron la medicación tras prescripción remota del hepatólogo a aquellos con infección activa que la aceptaron e implementaron intervenciones educativas y de reducción de daños.
Participantes y resultadosEntre octubre 2018 y marzo 2021, 566 usuarios aceptaron el cribado. 134 (24%) tenían una infección activa, con mayor prevalencia entre usuarios del CRD (42% vs 17%; p<0,001), que más frecuentemente eran extranjeros, estaban en situación de calle, reportaban consumo activo de drogas y compartir jeringuillas. La respuesta viral sostenida (RVS) global por intención de tratar (ITT) y por protocolo (PP) fue del 70% y el 88% respectivamente. La adherencia global fue buena en ambos grupos; sin embargo, la RVS fue mayor en usuarios del CA que del CRD (RVS-ITT 81% vs 55%). Todas las reinfecciones se produjeron en el CRD.
ConclusionesEste circuito centrado en el paciente liderado por enfermeras demuestra que el tratamiento del VHC puede administrarse exitosamente a PQID, incluso con consumo activo y complejidad socioeconómica. Debemos tener en cuenta las características específicas de los usuarios al establecer estas intervenciones para maximizar su éxito.
Artículo
Comprando el artículo el PDF del mismo podrá ser descargado
Precio 19,34 €
Comprar ahora