The COVID-19 pandemic has been associated with a decrease in the colorectal cancer (CRC) incidence, due to the disruption of screening programmes and a downscaling of endoscopic activity. The endpoint of this study is to evaluate if the pandemic has led to a change in CRC diagnostic rate and presentation in our population.
MethodsMulticenter retrospective study of all public hospitals of the Aragon region, attending a population of 1,329,391 inhabitants. We have analyzed all CRC cases detected and endoscopic units workload the year before the pandemic onset (1 March 2019–14 March 2020) and the first year of the COVID-19 pandemic (15 March 2020–28 February 2021).
ResultsThe diagnosis of CRC cases dropped a 38.9% (888 pre-pandemic vs 542 pandemic cases). Also, there were 30.3% less colonoscopies performed (24,860 vs 17,337). During the pandemic, CRC cases were diagnosed in older patients (72.4±12.2 vs 71.2±12.1 years, p=0.021), and had more frequently severe complications at diagnosis (14.6% vs 10.4%, p=0.019). Moreover, most CRC cases were diagnosed in symptomatic patients (81.4%). No significant difference was found in CRC stage at diagnosis, although stage IV was more frequent (20.1% vs 16.1%). Most hospitals reported a lower workload of endoscopic activity.
ConclusionCRC diagnostic rate was lower after the onset of the pandemic. CRC was diagnosed in older patients and was more frequently associated with complications. After the onset of the pandemic, the endoscopic units did not reach the workload performed previously.
La pandemia del COVID-19 ha provocado una disminución en la incidencia de cáncer colorrectal (CCR) tras la suspensión de los programas de cribado y la reducción de la actividad endoscópica. El objetivo del estudio es evaluar si la pandemia se ha asociado a un cambio en la incidencia y presentación del CCR en nuestra población.
MétodosEstudio multicéntrico, retrospectivo de todos los hospitales públicos de Aragón, con 1.329.391 habitantes. Analizamos todos los CRC detectados y la carga laboral de las unidades de endoscopia del año prepandémico (1 marzo 2019 – 14 marzo 2020) y el primer año de la pandemia (15 marzo 2020 – 28 febrero 2021).
ResultadosEl diagnóstico de CRC descendió un 38,9% (888 casos prepandemia vs. 542 en pandemia). Se realizaron un 30,3% menos de colonoscopias (24.860 vs. 17.337). El CRC en pandemia se diagnosticó en pacientes de mayor edad (72,4±12,2 vs 71,2±12,1 años; p=0,021) y presentaron más complicaciones graves en el momento del diagnóstico (14,6 vs. 10,4%; p=0.019). La mayoría de los CRC se diagnosticaron en pacientes sintomáticos (81,4%). No hubo diferencias en el estadio al diagnóstico aunque el estadio iv fue más frecuente (20,1 vs. 16,1%). La mayoría de los hospitales reiniciaron la actividad endoscópica con una menor carga laboral.
ConclusiónLa tasa diagnóstica de CRC descendió tras el inicio de la pandemia, el CRC fue diagnosticado en pacientes mayores y se asoció con más complicaciones al diagnóstico. Tras el inicio de la pandemia, la mayoría de los hospitales reiniciaron su actividad con una menor carga laboral.
Colorectal cancer (CRC) is the third most common cancer worldwide, ranking second in terms of mortality.1 Its incidence raises in parallel with economic progress, so its global incidence is expected to markedly increase in the following years.2 CRC cancer screening has proven to reduce its incidence and mortality, and most western countries have implemented screening programmes based on faecal occult blood test followed by colonoscopy if positive. However, the implementation of this programmes has strained endoscopic units, increasing the colonoscopy workload and waiting lists.3–5
Since December 2019, the novel coronavirus disease 2019 (COVID-19), caused by the SARS-CoV-2 virus has been spreading throughout the world. On March 2020, it was declared a pandemic by the World Health Organization.6 COVID-19 pandemic has posed and unprecedented challenge to most health systems, causing the downscaling of almost all other clinical activities. CRC Screening Programmes around the world have been paused,7 and the number of colonoscopies performed for other indications have also declined dramatically.8,9 Indeed, Gastrointestinal Endoscopy societies recommended to postpone most non-urgent endoscopic procedures at that time.10,11 After the first wave of the pandemic, with the arrival of vaccination, screening programmes and endoscopic activity have been gradually resumed, but the effect of its previous discontinuation on CRC incidence and mortality are still not known.12,13
Several studies have reported a decrease of CRC diagnosis up to 20–40% during COVID-19 pandemic in the same population, reflecting underdiagnosed CRC cases.14–18 It can be hypothesized that these underdiagnosed cases would be detected at a more advanced stage, which implies a worse long-term prognosis.
Another foreseeable outcome of the disruption of the screening programmes has been that the proportion of CRC cases presenting with abdominal symptoms has increased during the pandemic.18 Of note, several studies have reported that the number of CRC cases who needed and emergency admission and that of patients presenting with bowel obstruction have also significantly increased,18–20 highlighting the short-term effect of the COVID-19 pandemic on CRC presentation. The short-term effect of COVID-19 pandemic on CRC stage at diagnosis is still a point of contention. Several studies did not find significant differences in CRC stage prior or after the pandemic.14,18,20,21 Conversely, other groups have reported that CRC patients were diagnosed at significantly more advanced stages after the onset of the pandemic.17,22
In this study, we have compared CRC diagnostic rate, presentation and clinical features between the first year after the state of emergency and lockdown due to COVID-19 pandemic in Spain with a same length period prior to the pandemic, in a region with a population of more than one million inhabitants. In addition, we have analyzed how endoscopic activity has been resumed in this region after the first wave of the pandemic.
Patients and methodsStudy populationWe performed a multicentre observational retrospective study, with the participation of the seven reference hospitals of the region of Aragon (Spain), covering the health assistance of 1,329,391 inhabitants. The number of CRC cases diagnosed in this population, along with their clinical characteristics were compared between two periods: pre-pandemic (1 March 2019–14 March 2020) and pandemic (15 March 2020–28 February 2021). These periods were chosen as in Spain, the state of emergency and population lockdown was declared on 13 March 2020.
According to CRC patients’ characteristics, we evaluated sociodemographic features and presence of gastrointestinal symptoms before diagnosis, serious complications at diagnosis (intestinal obstruction, perforation, or lower bleeding that requires hospitalization) location, and CRC stage. Patients were identified from the database of the Pathology services and/or multidisciplinary tumour committee in each hospital.
Colonoscopy indication was registered, considering as main indications: evaluation of gastrointestinal symptoms, CRC screening (including all the colonoscopies performed in asymptomatic average-risk patients due to a positive faecal occult blood test, both in the local CRC population-based screening programme setting and in opportunistic screening), and follow-up colonoscopies in patients with previous history of adenomas, CRC, genetic predisposition syndromes or family history of colonic neoplasia.
We also evaluated the resumption of activity in the endoscopy units by comparing the number of endoscopies performed during the pandemic and the pre-pandemic period. The workload at which the activity was restarted and the patients’ time on the waiting list from the request for the colonoscopy to its realization have been analyzed and compared, considering 100% the pre-pandemic endoscopic activity. Diagnostic delays were evaluated in both periods, comparing the difference in days from the date of the colonoscopy request to the date of its performance.
Ethics approvalThe study protocol was reviewed and approved by the local Ethics committee (Aragon Health Research Institute) – Approval data 24 March 2021. Study code PI21/093. Patient informed consent for data analysis was waived because individual patients were not identified.
Statistical analysisQualitative variables were expressed as frequencies and percentages, whereas continuous variables were reported as the mean with standard deviation (SD) or median with interquartile range (IQR). Normality was tested using Kolmogorov–Smirnov test.
Differences between the two independent groups were evaluated with Chi-square (χ2) test for qualitative variables and with T Student's test or Mann–Whitney test for continuous variables.
For all tests, a two-sided p-value<0.05 was considered statistically significant. The statistical analysis was performed using the SPSS software v26.0 (IBM Corporation®) license of the University of Zaragoza.
Study aimsThe primary endpoint of this study was to assess whether the COVID-19 pandemic has led to a change in CRC diagnostic rate and presentation in our population, comparing pandemic and pre-pandemic periods of the same length. Secondary endpoints were to analyze and compare the CRC stage at diagnosis between both periods and to evaluate the restart of endoscopic activity after the pandemic between the participating hospitals.
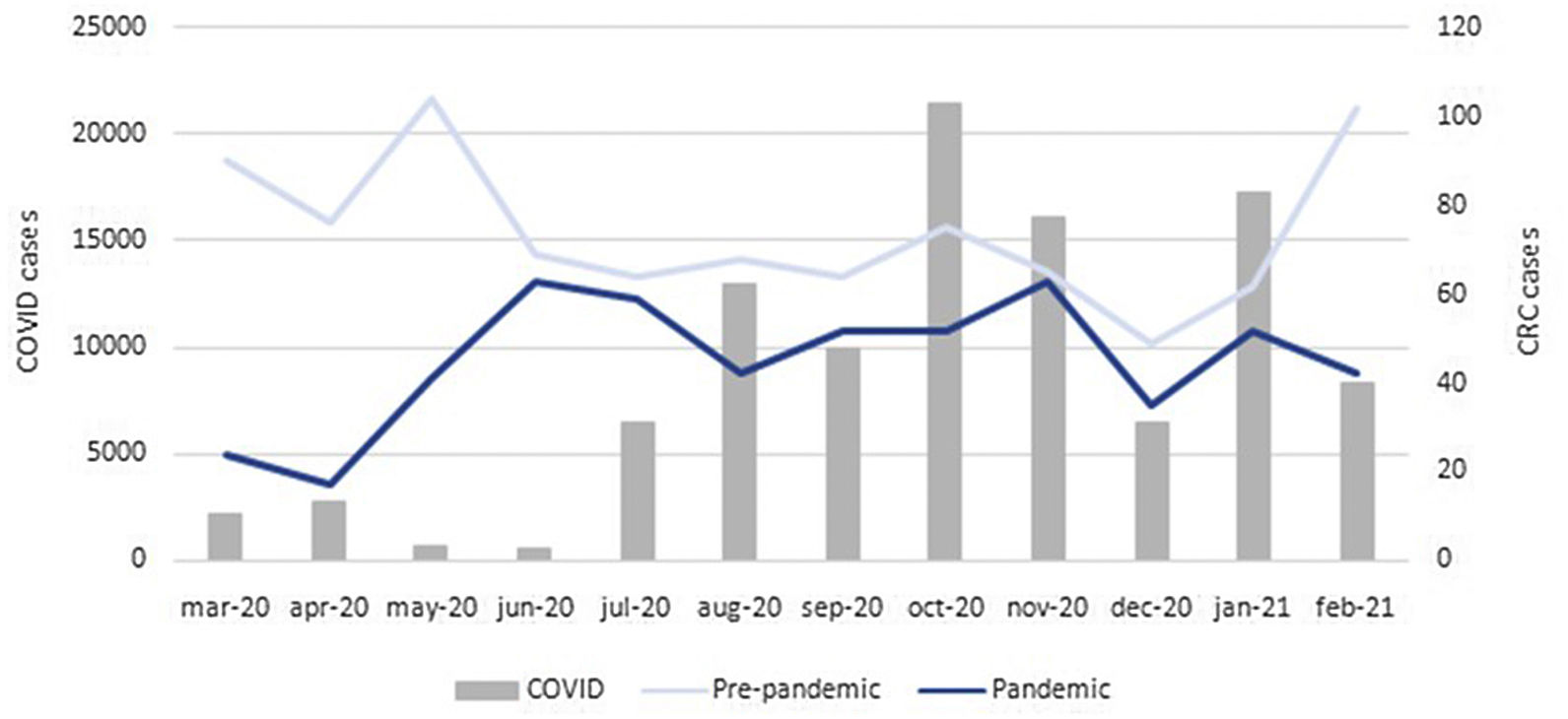
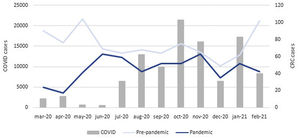
ResultsSeven hospitals with a reference population of approximately 1,329,391 inhabitants participated in the study. A total of 1430 CRCs were diagnosed, 888 (62.1%) in the pre-pandemic period and 542 (37.9%) in the pandemic period, which means a 38.9% decrease in the number of CRC cases diagnosed in the same population in a year's time. The absolute number of CRC cases diagnosed monthly in both periods along with the number of COVID-19 confirmed cases in Aragon are represented in Fig. 1. Regarding the number of colonoscopies performed, 24,860 were performed in the pre-pandemic period. During the pandemic period, this figure dropped up to a 30.3% (17,337 colonoscopies).
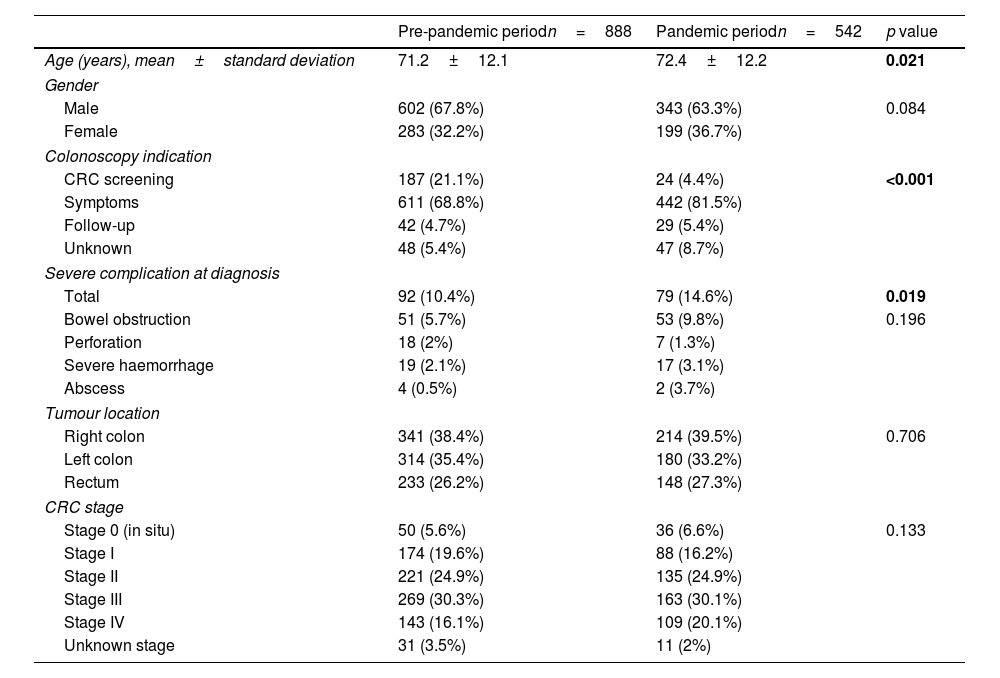
Demographic and clinical characteristics of CRC patients diagnosed in both periods are summarized in Table 1.
Demographic and clinical features of all CRC cases (1430) diagnosed in both periods.
| Pre-pandemic periodn=888 | Pandemic periodn=542 | p value | |
|---|---|---|---|
| Age (years), mean±standard deviation | 71.2±12.1 | 72.4±12.2 | 0.021 |
| Gender | |||
| Male | 602 (67.8%) | 343 (63.3%) | 0.084 |
| Female | 283 (32.2%) | 199 (36.7%) | |
| Colonoscopy indication | |||
| CRC screening | 187 (21.1%) | 24 (4.4%) | <0.001 |
| Symptoms | 611 (68.8%) | 442 (81.5%) | |
| Follow-up | 42 (4.7%) | 29 (5.4%) | |
| Unknown | 48 (5.4%) | 47 (8.7%) | |
| Severe complication at diagnosis | |||
| Total | 92 (10.4%) | 79 (14.6%) | 0.019 |
| Bowel obstruction | 51 (5.7%) | 53 (9.8%) | 0.196 |
| Perforation | 18 (2%) | 7 (1.3%) | |
| Severe haemorrhage | 19 (2.1%) | 17 (3.1%) | |
| Abscess | 4 (0.5%) | 2 (3.7%) | |
| Tumour location | |||
| Right colon | 341 (38.4%) | 214 (39.5%) | 0.706 |
| Left colon | 314 (35.4%) | 180 (33.2%) | |
| Rectum | 233 (26.2%) | 148 (27.3%) | |
| CRC stage | |||
| Stage 0 (in situ) | 50 (5.6%) | 36 (6.6%) | 0.133 |
| Stage I | 174 (19.6%) | 88 (16.2%) | |
| Stage II | 221 (24.9%) | 135 (24.9%) | |
| Stage III | 269 (30.3%) | 163 (30.1%) | |
| Stage IV | 143 (16.1%) | 109 (20.1%) | |
| Unknown stage | 31 (3.5%) | 11 (2%) | |
The mean age of patients was 71.6±12.1 and 945 (66.1%) were males, considering all patients included. There were no significant differences regarding sex between both periods (67.8% males pre vs 63,3% males post, p=0.084), but in the pandemic period the age at diagnosis was significantly higher (mean age 71.2±12.1 years pre vs mean age 72.4±12.2 years post; p=0.021).
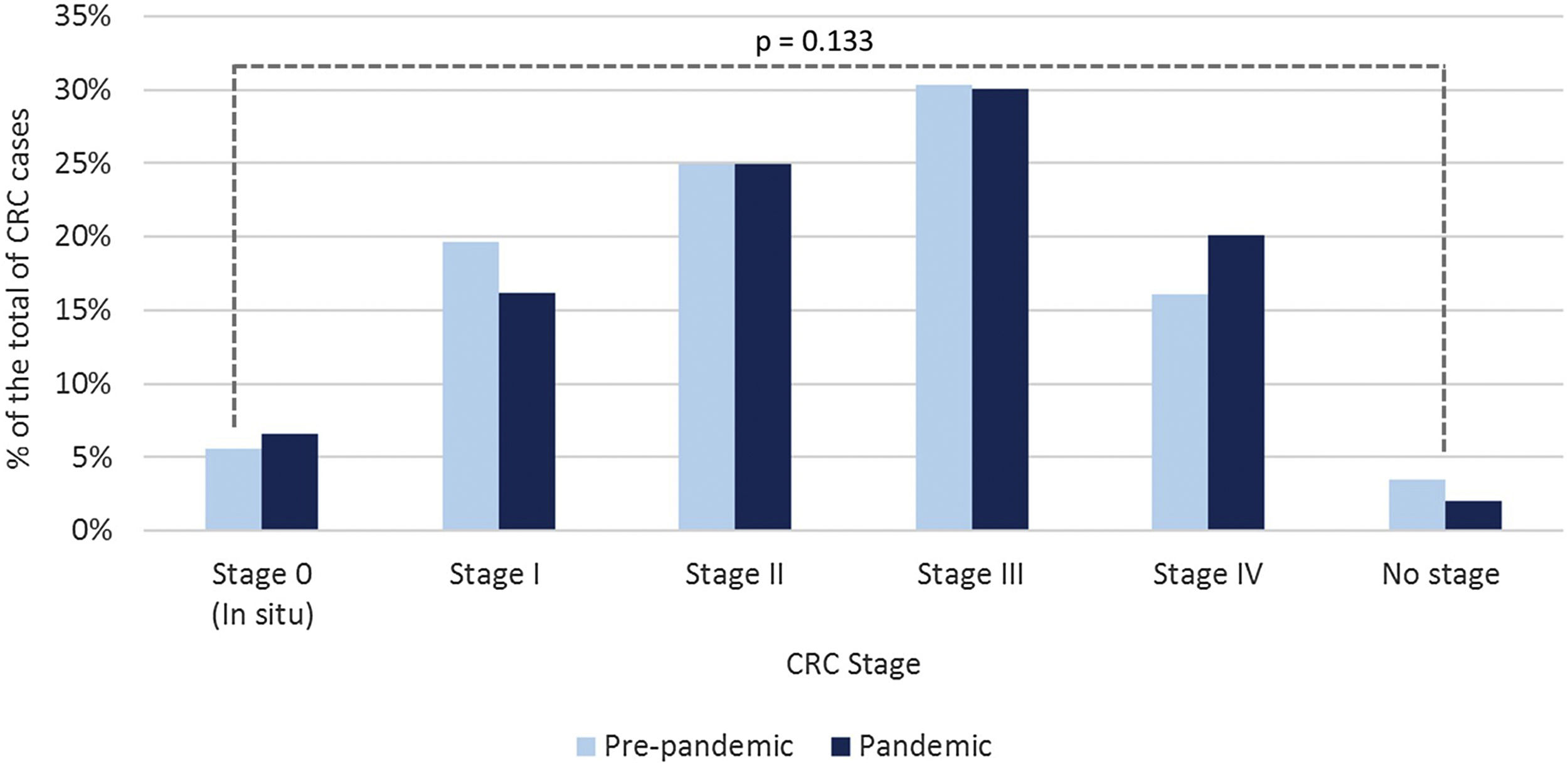
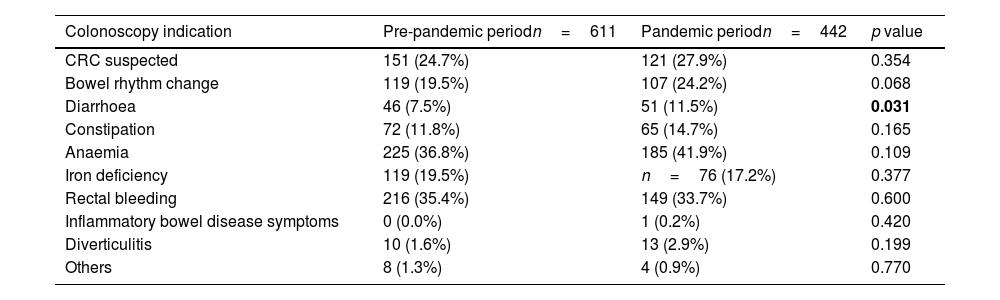
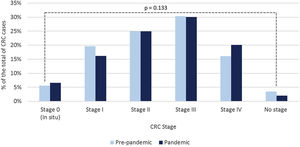
Regarding colonoscopy indications, significantly fewer tumours were identified by CRC screening in the pandemic period, being most CRC (81.5%) detected in colonoscopies requested to evaluate gastrointestinal symptoms (p<0.001). Diarrhoea was the only symptom more frequently reported as the cause of colonoscopy referral in the pandemic period (Table 2). CRC cases detected in surveillance/follow-up colonoscopies did not differ between both periods (p=0.617). The debut at diagnosis with a serious complication (perforation, abscess, obstruction, or bleeding requiring admission) was significantly higher (p=0.019) during the pandemic period. No significant differences were found in CRC stage at diagnosis between both periods (p=0.133).
Prevalence of gastrointestinal symptoms of the 1053 symptomatic patients referred to colonoscopy in both periods.
| Colonoscopy indication | Pre-pandemic periodn=611 | Pandemic periodn=442 | p value |
|---|---|---|---|
| CRC suspected | 151 (24.7%) | 121 (27.9%) | 0.354 |
| Bowel rhythm change | 119 (19.5%) | 107 (24.2%) | 0.068 |
| Diarrhoea | 46 (7.5%) | 51 (11.5%) | 0.031 |
| Constipation | 72 (11.8%) | 65 (14.7%) | 0.165 |
| Anaemia | 225 (36.8%) | 185 (41.9%) | 0.109 |
| Iron deficiency | 119 (19.5%) | n=76 (17.2%) | 0.377 |
| Rectal bleeding | 216 (35.4%) | 149 (33.7%) | 0.600 |
| Inflammatory bowel disease symptoms | 0 (0.0%) | 1 (0.2%) | 0.420 |
| Diverticulitis | 10 (1.6%) | 13 (2.9%) | 0.199 |
| Others | 8 (1.3%) | 4 (0.9%) | 0.770 |
Considering stages III and IV as advanced stage CRC, we found no statistically significant differences between both periods (pre 412 (46.4%) vs post 272 (50.2%); p=0.173), although there was a trend towards a higher percentage of stage IV tumours in the post pandemic period (143 (16.1%) pre vs 109 (20.1%) post). The distribution of CRC stage at diagnosis in both periods is represented in Fig. 2.
Regarding diagnostic delays, we found a statistically significantly shorter delay in the pandemic period (median 27.0 days (IQR 7.0–57.0) pre vs median 19.0 days (IQR 5.0–47.0) post; p=0.006).
The resumption of activity in the endoscopy units after the lockdown declared by the Spanish government was not homogeneous in the seven participating hospitals. Scheduled endoscopic activity was resumed between one month and four months after the lockdown. All the centres restart with a partial activity: 2/7 hospitals began with a volume of work greater than 75%, 3/7 hospitals with an activity between 50 and 75% and 2/7 hospitals with an activity between 25 and 49%.
DiscussionThe COVID-19 pandemic has led to a decrease CRC diagnostic rate. In our population, we have detected a decrease in CRC diagnostic rate as high as 38.9% comparing the first year after the state of emergency declaration in Spanish territory with an analogous period prior to the pandemic. Similar figures have been consistently reported by other studies.14–18 The number of CRC cases diagnosed was lower for all CRC stages in the pandemic period and no significant differences were found in the frequency of advanced stage CRC (stages III+IV) between both periods. However, it should be noted that in the pandemic period the frequency of stage I CRC was lower whereas the proportion of CRC cases in stage IV at diagnosis increased, although both differences did not reach significance. Stage II and III remained stable between both periods. A study from the Netherlands yielded similar results, with a 25% decrease in stage I CRC incidence in the pandemic period, being this figure lower in the rest of stages.23
As aforementioned, we have not found significant differences in the distribution by stages at diagnosis of CRC cases between both periods. The same conclusion was reached by other studies with a similar design performed in Spain,14,18 Italy21 and the UK.20 However, emphasis should be placed in the already mentioned higher proportion of stage IV CRC cases in the pandemic period. A single centre Japanese study comparing 1581 cases diagnosed 3 years before the pandemic onset with 360 CRC cases diagnosed from March to December 2020, similarly, reported no significant differences in stage IV CRC between both periods. However, in contrast to our results, this group found a significant decrease in localized CRC cases during the pandemic (−34.1%) and a rise in regional stage CRC (+56.9%).17 An Australian cohort yielded analogous results, with significantly less patients diagnosed with stage I CRC and proportionally more patients with stage II or III at diagnosis.22
Patients diagnosed with CRC after the onset of the pandemic were significantly older in our population. This may be related to the disruption of the screening programmes, which implies a lower number of colonoscopies performed in 50–70 years old population. Thus, that appears to be a predictable finding. However, other studies with analogous design did not report this difference in CRC patients age,17–21 or even found that CRC patients diagnosed after the pandemic onset were younger.22
In other studies, with a similar design, a higher proportion of CRC patients were diagnosed with rectal cancer after the onset of the pandemic (33.8% vs 28.3% in Italian population,21 44.2% vs 29.9% in Spanish population18). It has been hypothesized that this may be related to a more frequent and evident symptoms in rectal tumours, prompting to endoscopic examination regardless of the shutdown of the screening programmes. Nevertheless, no differences were found in CRC location in our cohort (rectal tumours account for 26.2% of the cases diagnosed in pre-pandemic period, 27.4% in pandemic period). Indeed, this is an inconsistent finding between different studies, as in an Australian cohort rectal location was even less frequent during pandemic period.22
An expected consequence of the shutdown of screening programmes is that most CRC patients diagnosed in the pandemic period presented gastrointestinal symptoms. In our cohort, 81.5% CRC cases were detected in symptomatic patients in the pandemic period, a proportion significantly higher when compared with pre-pandemic period (68.8%). Only 4.4% of the CRC cases diagnosed after the declaration of the state of emergency were detected by screening. It must be highlighted that CRC screening programme was disrupted from March to the end of November 2020 in our region, so many of these CRC diagnosed in the pandemic period may have been detected by opportunistic screening. Similar finding were reported by another Spanish study, with a 94.8% of CRC cases diagnosed outside the screening programme after the onset of the pandemic.18 A more unpredictable finding is that the number of patients presenting with a serious complication has significantly increased, even in this short-term analysis (14.6% vs 10.4%). Likewise, other studies have also reported that only a short delay (months) in referral and diagnosis caused a significant increase of CRC cases in need of urgent surgery20,22 and presenting with bowel obstruction: 8.6% vs 4.3% in data from the UK20; 39% vs 15% in data from Japan,19 9.8% vs 5.4% in our cohort. This finding is especially relevant, as the need of urgent surgery has been associated with a significantly worse prognosis compared with CRC patients managed by elective surgery.24
Regarding the resumption of endoscopic activity, it has been estimated that the colonoscopy capacity should be increased compared with pre-pandemic workload, to catch-up the backlog of screening colonoscopies accrued during the lockdown. To this end, in the Netherlands, colonoscopy availability was increased up to 120%, reporting a catch-up effect in the second half of 2020, with more CRC cases diagnosed compared with pre-pandemic period.23 In contrast, in our region, most hospitals have resumed endoscopic activity with a lower colonoscopy workload compared with the pre-pandemic period (four out of seven centres of our study reported<75% of activity). As a result, the number of CRC cases detected remained lower than pre-pandemic period in every month included in our analysis, and the catch-up effect could not be reached in our population. This failure to have a catch-up effect in CRC diagnosis the year after the onset of the pandemic has been also reported by other studies conducted in Spain14,16 and France.15
Therefore, efforts should be made to increase our colonoscopy capacity. However, most public health systems are unable to perform such a significant increase in the endoscopic workload. In such cases, it has been suggested that increasing FIT cut-off in screening programmes,25,26 using FIT for selecting symptomatic patients in need of colonoscopy,27 or prioritizing patients according to risk factors (male sex, advanced age) could be effective strategies to reduce the number of underdiagnosed CRC.26 It should be mentioned that in a modelling study performed in Italy, disruptions of the CRC screening programme up to 4–6 months would not affect CRC stages or prognosis. Only a sustained backlog beyond 6 months would significantly increase CRC cases detected at advanced stages along with a mortality increase (12% at 5 years) if the delay persists more than one year. Obviously, real-life data regarding how COVID-19 will affect CRC long-term prognosis are not available and are difficult to estimate, but this fact will rely on several factors such as the implementation of the strategies mentioned above or maintaining high participations rates in screening programs.28,29
Finally, although the number of colonoscopies performed during the pandemic period was considerably lower (24,860 vs. 17,337 colonoscopies), the time until these procedures were carried out was shorter than during pre-pandemic period (19 vs 27 days). This finding is difficult to explain, as most studies analyzing delays during the pandemic have reported increased colonoscopy waiting lists9,30,31 and even CRC treatment delays.32 This may be due to an accurate selection of patients in need of colonoscopy, avoiding colonoscopies deemed not necessary and quickly performing selected examinations in high risk patients.
The strengths of our study are that it provides real-life data, with a higher sample size that most studies with similar design currently available,14,18–20 allowing to support several hypotheses previously advocated about how COVID-19 pandemic has influenced in CRC diagnosis and presentation. Very few studies have provided simultaneous data regarding changes in CRC diagnostic rate, staging and clinical characteristics during the pandemic along with data explaining exactly how endoscopic activity has been resumed23 and the delays accrued in the same population.30 The main limitation is the retrospective design of the study, so we have not been able to provide solid evidence regarding how these changes in CRC diagnostic rate and presentation will influence the prognosis of this disease. Prospective studies with longer follow-up periods are necessary in this setting. It is worth mentioning that the differences found in CRC detection rate and colonoscopies performed could be mostly related to the 2-moth period of almost total endoscopic activity shutdown after the onset of the pandemic (March–April 2020, Fig. 1). These differences may not be as relevant if this period had not been included in the analysis. However, we believe this design allows to reflect the real impact of COVID-19 pandemic.
In conclusion, our results support the fact that CRC diagnosis has dropped the first year after the onset of COVID-19 pandemic, with more patients presenting with abdominal symptoms or even with serious complications. The short-term impact of COVID-19 pandemic on CRC stage at diagnosis has not yet been determined, although it does not appear to be significant in our population. Nevertheless, this may change in the long-term, influenced by several factors such as the prompt and complete resumption of endoscopic activity or the availability of maintaining high participation rates in CRC screening programmes. Efforts to increase colonoscopy capacity or precise strategies to improve selection of high-risk patients in need of colonoscopy are urgently needed to detect the CRC cases and pre-malignant lesions underdiagnosed during this time, an objective which is far from being reached within the time frame of our study. If we are able to increase our endoscopic activity and adequately reactivate the screening programmes, we can minimize this impact in the medium and long term. We are in a window of opportunity to achieve this objective, and if necessary, we can seek the complicity of civil society and patient associations to achieve this essential objective.
Authors’ contributionsMaría Jose-Domper and Angel Lanas design the study. Gonzalo Hijos-Mallada, Enrique Alfaro, Mercedes Navarro, Pablo Cañamares, Inés Ariño, Mara Charro, Carlo Bruno, Marina Solano, Ana Pardillos and Cristina Jimeno collected and analyzed the data. Patricia Carrera-Lasfuentes performed the statistical analysis. Gonzalo Hijos-Mallada, Maria Jose Domper-Arnal and Enrique Alfaro drafted the original manuscript. All authors have revised and approve the final version of the manuscript.
Data availability statementThe datasets generated for this study are available on request to the corresponding authors.
Funding informationGonzalo Hijos-Mallada and María José Domper-Arnal were partially supported by the National Institute Carlos III (Rio Hortega Grants number CM20/00088 and CM19/00094). This study was supported by funds from the research group GIIS027 from the Aragón Health Research Institute (IIS Aragón).
Conflict of interestsThe authors declare no conflict of interest.
The authors wish to thank all the members of the multidisciplinary tumour committees of the seven hospitals involved in this study, who have provided the necessary data to perform this analysis.