Amyloidosis is a disease characterized by the deposit of amyloid protein material in the organs causing their dysfunction. Different types of amyloidosis have been described according to the aetiology. These include primary amyloidosis (AL) and secondary amyloidosis (AA), among others. It can also be classified according to its location: systemic or localized amyloidosis. Localized amyloidosis most frequently affects the respiratory and lower urinary tract and subcutaneous tissue.1 Isolated intestinal involvement is infrequent. In fact, in a meta-analysis published by Alsheri et al., there were only 14 cases identified that were published between 1960 and 2019.2 This report presents the case of a patient with AL localized in the intestine with an atypical presentation based on migratory stenosis that responded to oral corticosteroid treatment.
A 72-year-old man with no toxic habits and no medical history was admitted because of 3 days of evolution of abdominal pain, vomiting and constipation. The patient had suffered 4 similar episodes in the previous two months.
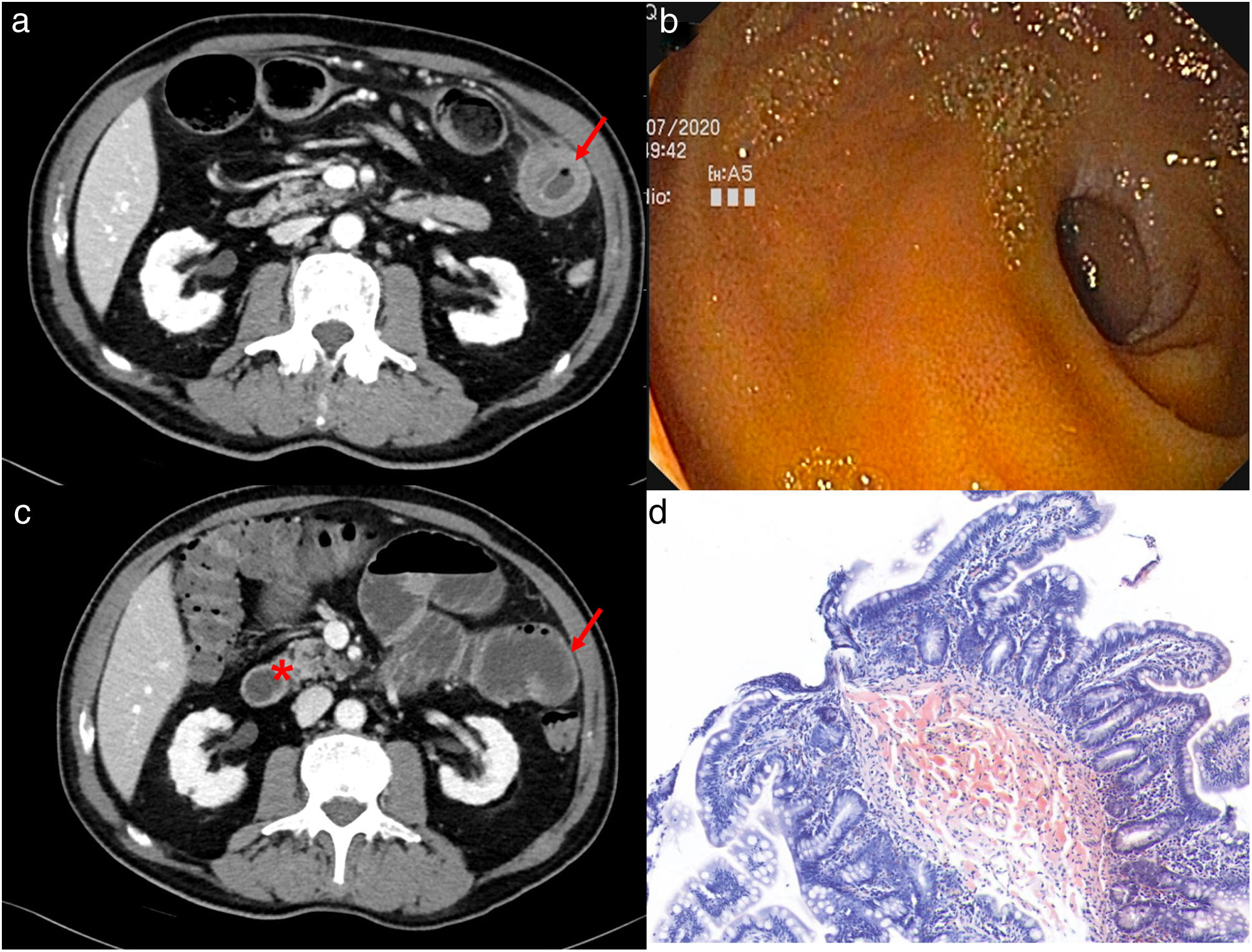
Blood analysis showed an increase of acute phase reactants (15,000 leukocytes and 8mg/dl C-reactive-protein). Abdominal computed tomography (CT) revealed a progressive calibre change in the right iliac fossa without identifying the cause and three segmental thickenings in the jejunum (Fig. 1a). An upper intestinal enteroscopy was performed, visualizing a stricture in the jejunum with prestenotic dilatation and two ulcerations with fibrin. Biopsies were taken (Fig. 1b). 72h after the procedure, he presented clinical worsening so a CT-scan was repeated. Jejunal thickenings in different locations to those observed in the previous scans were seen (Fig. 1c). While waiting for the results of the biopsies, a systemic steroid treatment was started under inflammatory bowel disease suspicion. The patient evolved favourably, presenting both clinical and radiological resolution.
The histological study showed nodular deposits of amorphous eosinophilic hyaline material in the submucosa, Congo red positive and permanganate resistant, compatible with primary intestinal amyloidosis (Fig. 1d). The study was completed with bone marrow aspirate, a subcutaneous fat biopsy, a cardiac resonance and a urine study, ruling out systemic involvement.
The digestive tract is involved in up to 60% of AL cases. However, the isolated involvement of this organ is exceptional. The clinical presentation depends on the area, abdominal pain and intestinal obstruction in the small intestine (commonly in jejunum) and rectal bleeding when involving the colon (commonly in sigma).2
Localized AL has a low risk of progressing to a systemic disease and therefore has a better prognosis than systemic AL. Localized AL is often managed with local endoscopic and surgical treatment. A systemic treatment is usually avoided due to unfavourable risk/benefit.3 In our case, local treatment was ruled out due to the location of the lesions and their migratory nature. After the clinical response to the steroid therapy, a progressive withdrawal of treatment was attempted. However, the patient presented recurrence of the suboclusive symptoms when the dose of steroids was reduced below 10mg. It was decided that the treatment would be maintained chronically at the lowest effective dose.
An extensive review of literature found no cases of intestinal localized AL treated with steroids. However, in systemic AL, corticosteroids are used extensively with other chemotherapy agents such as bortezomib.4
In conclusion, intestinal localized AL is a rare entity. Systemic steroid therapy could be helpful in those cases where local treatment cannot be performed. Studies to confirm the hypothesis that our case suggests are needed.
Patient consentThe patient has given his informed consent to publish the information included in the article.
Authors’ contributionsBelen Garcia and Eduard Brunet reviewed the case, the available literature data and wrote the manuscript. Alex Casalots, Carlota Cano, Carlos Feijoo and Sonia Piernas critically reviewed the text and provided important intellectual content. All authors definitively approved the submitted version.
FundingNone.
Conflicts of interestNone of the authors have disclosed any conflict interest regarding the present case report.