Budd-Chiari syndrome is defined as occlusion to hepatic venous flow, excluding congestive heart disease and sinusoidal obstructive syndrome. There are two classifications of Budd-Chiari syndrome: primary, which involved thrombosis of the suprahepatic veins without associated compression or invasion by malignancy or parasitosis and secondary, where this is due to other causes.1 Secondary causes include compression of hepatic venous structures by space-occupying lesions such as benign and malignant neoplasms.
We present the clinical case of a 54-year-old woman with a medical history of a space-occupying lesion of cystic nature in the caudate hepatic lobe, in direct contact with the exit of the suprahepatic veins, intervened on two occasions in another hospital. In 2016 a laparoscopic unroofing was performed. After this intervention, due to recurrence of the lesion, a right hepatectomy was performed in 2021; however complete excision of the lesion was not possible due to the involvement of the left and middle suprahepatic veins. The anatomophathogical findings were consistent with a diagnosis of hepatic cystadenoma.
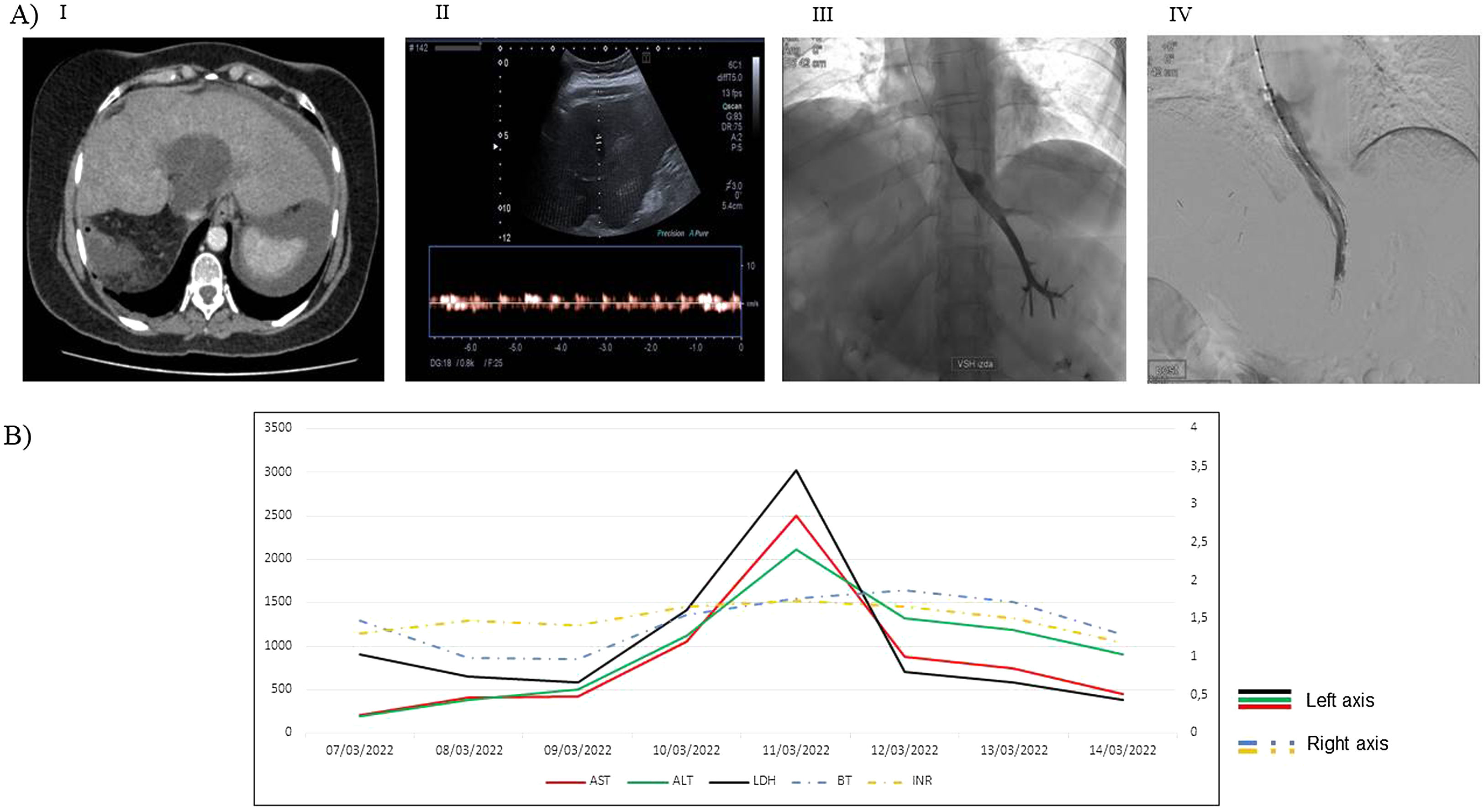
The woman presented to the emergency department with general malaise and repeated syncope, without presenting infectious symptoms. Blood analysis showed an altered liver profile with elevated cytolysis enzymes, as well as LDH and INR prolongation. An abdominal CT (comuted tomography) scan visualized the cystoadenoma as a multiloculated formation measuring 4cm×8cm×7cm, centered in the caudate lobe, with involvement of the inferior vena cava and the presence of a small amount of ascites (Fig. 1). During the first 72h of admission, the woman presented progressive worsening of clinical symptoms with increased general malaise, asthenia, severe nausea and pallor. Analytical controls showed a tenfold increase in transaminases, a threefold increase in LDH and an INR prolonged above 1.5.
(A) Summary of imaging test: (i) Serous cystadenoma on abdominal CT scan. (ii) Left hepatic suprahepatic vein on ultrasound showing reduced velocity. (iii) Slowed contrast washout with sharp area due to extrinsic compression. (iv) Early contrast washout after self-expanding prosthesis. (B) Analytical evolution (the peak coincides with the placement of the prosthesis). (i) Aspartate aminotransferase (AST). (ii) Alanine aminotransferase (ALT). (iii) Lactate dehydrogenase (LDH). (iv) Total bilirubin (BT). (v) International normalized ratio (INR).
An urgent abdominal ultrasound was performed, revealing a stable cystic lesion with respect to the CT scan taken at admission, as well as a tubular structure compatible with the left suprahepatic vein, dilated and with a slowed Doppler signal (Fig. 1), and increased ascites.
In view of the overall worsening, an emergency phlebography was performed, which showed a single suprahepatic vein (left) with delayed contrast washout and with a progressive sharpening area where a prosthesis was placed, proving the adequate subsequent washout (Fig. 1). After the intervention, the woman presented a rapid clinical improvement, with progressive normalization of the analytical values, verified by ultrasound the correct flow in the remaining suprahepatic vein, with normalizing caliber and the resolution of ascites.
Hepatic cystadenomas are rare but nevertheless constitutes the most frequent hepatic cystic neoplasm.2 It is called hepatic mucinous cystic neoplasm, although in some cases the serous component predominates,3 and there are different classifications depending on the presence or absence of ovarian stroma or the type of predominant lining epithelium.3,4
We present a clinical case of Budd-Chiari syndrome with associated liver failure of unusual cause which required early action to remedy a serious situation. We also highlight that the clinical and analytical manifestations of suprahepatic vein obstruction are similar regardless of the etiology.
FundingThere are no financing for this manuscript.
Conflicts of interestThere are no conflicts of interest for this manuscript.