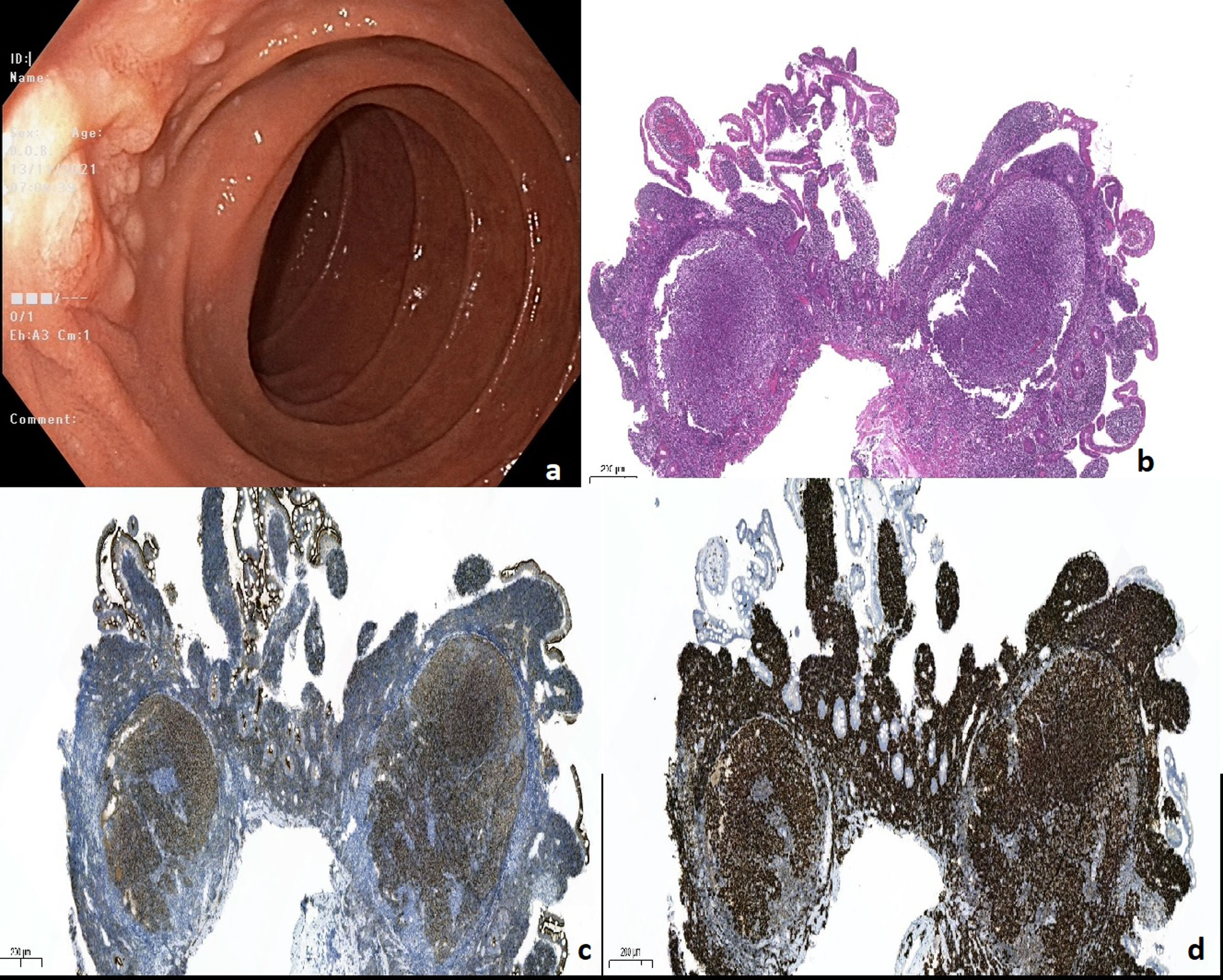
A 64-year-old male without complaint and remarkable past medical history was referred from check-up clinic for screening esophagogastroduodenoscopy and colonoscopy. It was learned from his family history that his father had lymphoma. Physical examination was normal and there was no sign of hepatomegaly, splenomegaly or lymphadenopathy. All laboratory findings, which include lactate dehydrogenase were normal. Esophagogastroduodenoscopy showed normal gastric mucosa and multiple whitish nodular lesions around the papilla of Vater (Fig. 1a). Multiple biopsies were taken from the stomach for investigation of Helicobacter pylori and the periampullary area of the duodenum on suspicion of duodenal adenomas. Ileocolonoscopy revealed no abnormality.
The histopathological examination of biopsy specimens from the stomach was negative for H. pylori. However, the histopathological examination of duodenal samples revealed a neoplasm that had pushed the dendritic cell network to the periphery, formed follicles, involved the lamina propria, contained centrocytes and a small number of centroblasts (Fig. 1b). The immunohistochemical staining of neoplastic cells from duodenal samples were positive for CD20, CD10 (Fig. 1c), BCL-6, and BCL-2 (Fig. 1d) but negative for CD5 and Cyclin D1. Ki-67 proliferation index was low. Based on these findings, the diagnosis was compatible with follicular lymphoma (FL).
Positron emission tomography with computed tomography scan showed neither adjacent nor distant metastasis. The final diagnosis of primary follicular lymphoma of the duodenum (D-FL), stage 1 was made. After discussing the treatment options with the patient and explaining the good prognosis of early-stage of disease without treatment, a “watch and wait” policy was chosen. In the first year follow-up of our patient, who has completed the ten months after diagnosis, it was planned to repeat gastroscopy, perform capsule endoscopy to evaluate the jejunum and ileum in our unit, and perform laboratory tests including LDH in the hematology outpatient clinic.
FL is one of the most common types of low-grade B-cell lymphoma, constituting 30% of non-Hodgkin's lymphomas.1 D-FL is a rare entity and was included in the WHO classification revision in 2016 as a variant of FL.2 It is usually discovered incidentally and the majority of patients presented with no symptoms.3 The disease involves mainly the second portion of the duodenum, and characteristic endoscopic findings are multifocal polyploid and nodular lesions.4 In the study of Takata et al., when capsule endoscopy (CE) or balloon enteroscopy (BE) was performed in patients with DF-L, jejunal or ileal lesions were found in 85% of the patients.3 Unfortunately, due to some insurance problems, we did not perform CE or BE on our patient, but we plan to do it on the first year follow-up. Patients with D-FL are generally diagnosed with a low-grade lesion at the early stage of the disease.5 Malignant transformation of gastrointestinal follicular lymphoma is extremely rare, although a few cases have been published.6,7 Because of the good prognosis of D-FL and toxic side effects of chemotherapy, for early-stage disease “watch and wait” approach is chosen by most oncologists.8 In advanced disease or if progression develops, a variety of treatments may be used, including local radiation therapy, chemotherapy, and rituximab.1 If we detect signs in favour of disease progression in the annual follow-up of our patient, one of these treatment options may be preferred.
Authors’ contributionsE.A.: Study design and data analysis, patient recruitment, data collection and writing up of the first draft of the paper. T.T.: Study design and data analysis. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
FundingNo specific funding has been received for this study.
Conflict of interestNone.