A 47-year-old woman, with no risk factors for liver disease, presented at emergency department with diffuse abdominal pain. Hepatic and cholestatic enzymes were elevated (AST 97U/L, GGT 259U/L and ALP 209U/L).
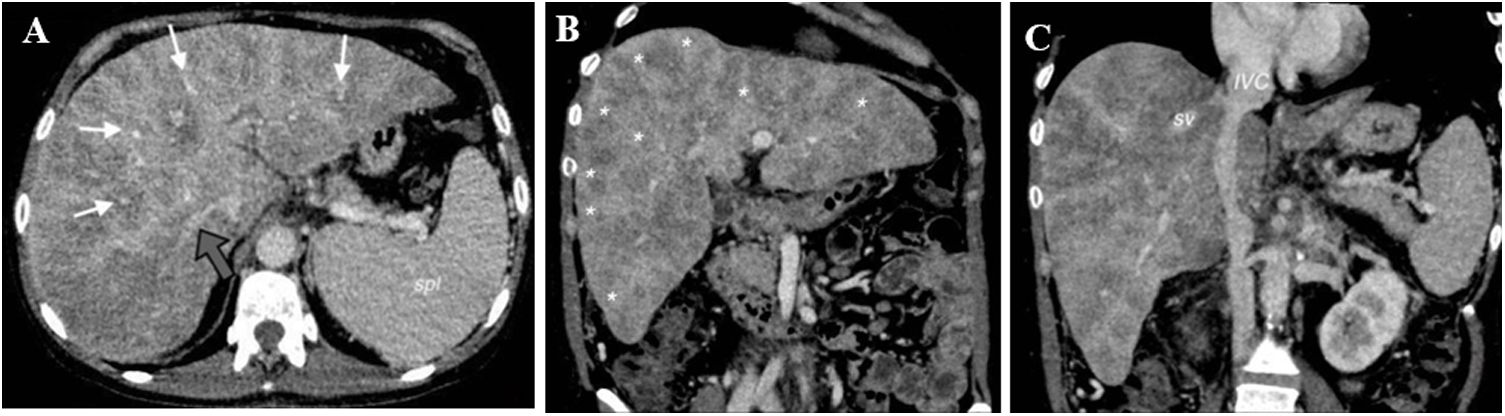
Due to the nonspecific clinical picture, she underwent a contrast-enhanced computed tomography. It showed heterogenous liver parenchyma with large hypodense areas surrounding the hepatic and portal veins, all patent. These findings were reported as probable atypical hepatic fatty infiltration with perivascular pattern (Fig. 1).
Axial [A] and coronal [B and C] contrast-enhanced CT image obtained at the level of the liver during the portal venous phase shows hepatomegalia with patchy and confluent areas of low-attenuation suggesting fat deposition, surrounding the portal and hepatic veins (white and grayarrows on A) in keeping with multifocal perivascular fatty infiltration. There were other regions of normal appearance liver parenchyma attenuation (*). Notice that intrahepatic vessels follow a normal course without mass effect. Suprahepatic veins (sv) and inferior vena cava (IVC) were patent.
There are several entities that could potentially mimic this pattern and should be considered in the differential diagnosis.1,2 For instance, (a) Budd-Chiari Syndrome, that was ruled out in this case because suprahepatic veins were patent,3 (b) malignant hepatic infiltration (hepatocelullar carcinoma, lymphoma or metastasis), also excluded due to the absence of mass effect and enhancement4 and (c) perfusion abnormalities, also excluded since they are hypervascular and not detectable on equilibrium phase images.5
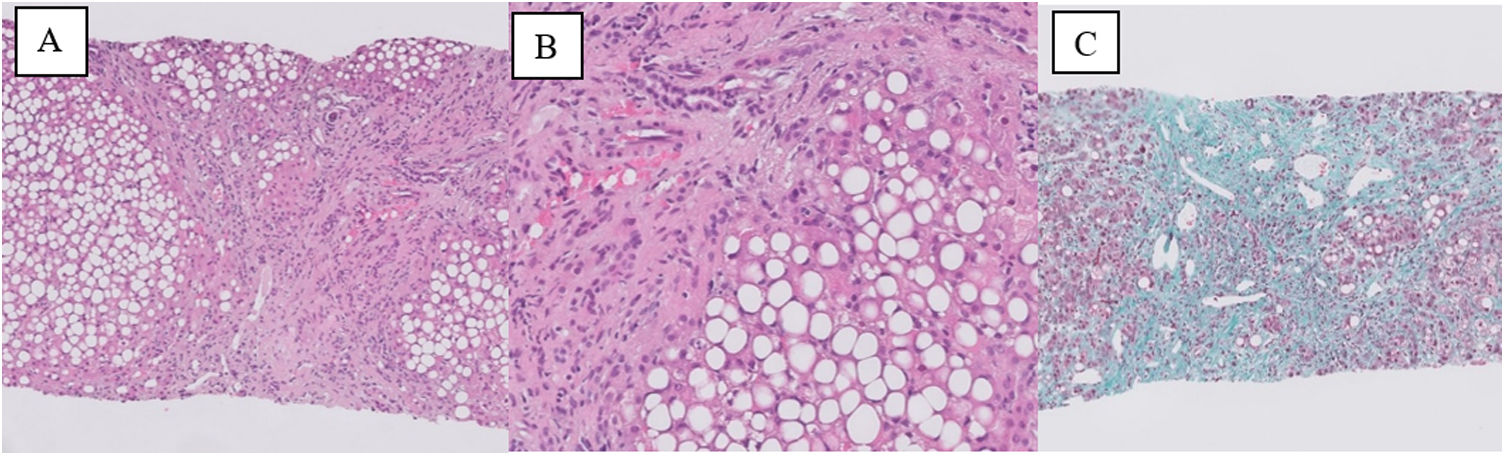
Our suspicion was confirmed afterwards through a biopsy: steatohepatitis and cirrhosis (Fig. 2).
Loss of normal liver architecture, replaced by bands of fibrous tissue surrounding the regenerative nodules (H&E stain [A]). Hepatocytes show severe macrovesicular fatty change (80%), focal necrosis and a mixed lobular inflammatory cell infiltrate (H&E stain [B]). Masson Trichrome stain [C] highlights the fibrous tissue and demonstrates the established cirrhosis.
The crucial role of the radiologist allows an accurate diagnosis of this infrequent presentation of this benign entity and therefore invasive procedures will be avoided.






![Axial [A] and coronal [B and C] contrast-enhanced CT image obtained at the level of the liver during the portal venous phase shows hepatomegalia with patchy and confluent areas of low-attenuation suggesting fat deposition, surrounding the portal and hepatic veins (white and grayarrows on A) in keeping with multifocal perivascular fatty infiltration. There were other regions of normal appearance liver parenchyma attenuation (*). Notice that intrahepatic vessels follow a normal course without mass effect. Suprahepatic veins (sv) and inferior vena cava (IVC) were patent. Axial [A] and coronal [B and C] contrast-enhanced CT image obtained at the level of the liver during the portal venous phase shows hepatomegalia with patchy and confluent areas of low-attenuation suggesting fat deposition, surrounding the portal and hepatic veins (white and grayarrows on A) in keeping with multifocal perivascular fatty infiltration. There were other regions of normal appearance liver parenchyma attenuation (*). Notice that intrahepatic vessels follow a normal course without mass effect. Suprahepatic veins (sv) and inferior vena cava (IVC) were patent.](https://static.elsevier.es/multimedia/02105705/0000004600000004/v2_202304070008/S021057052200214X/v2_202304070008/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)
![Loss of normal liver architecture, replaced by bands of fibrous tissue surrounding the regenerative nodules (H&E stain [A]). Hepatocytes show severe macrovesicular fatty change (80%), focal necrosis and a mixed lobular inflammatory cell infiltrate (H&E stain [B]). Masson Trichrome stain [C] highlights the fibrous tissue and demonstrates the established cirrhosis. Loss of normal liver architecture, replaced by bands of fibrous tissue surrounding the regenerative nodules (H&E stain [A]). Hepatocytes show severe macrovesicular fatty change (80%), focal necrosis and a mixed lobular inflammatory cell infiltrate (H&E stain [B]). Masson Trichrome stain [C] highlights the fibrous tissue and demonstrates the established cirrhosis.](https://static.elsevier.es/multimedia/02105705/0000004600000004/v2_202304070008/S021057052200214X/v2_202304070008/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w96p5LBcBpyJTqfwgorxm+Ow=)

